- Department of Neurovascular Service, “Mother Teresa” University Medical Center, Tirana, Albania
- Department of Biomedical and Experimental, Faculty of Medicine, University of Medicine, Tirana, Albania.
Correspondence Address:
Gentian Vyshka, Department of Biomedical and Experimental, Faculty of Medicine, University of Medicine, Tirana, Albania.
DOI:10.25259/SNI_1123_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ermir Roçi1, Stela Dodaj1, Gentian Vyshka2. Herpes simplex virus encephalitis mimicking acute ischemic stroke. 17-Feb-2023;14:60
How to cite this URL: Ermir Roçi1, Stela Dodaj1, Gentian Vyshka2. Herpes simplex virus encephalitis mimicking acute ischemic stroke. 17-Feb-2023;14:60. Available from: https://surgicalneurologyint.com/surgicalint-articles/12155/
Abstract
Background: Infections of the central nervous system might present in an acute form such as to be similar with the clinical characteristics of a stroke. This situation will hamper a correct diagnosis and a prompt treatment that can otherwise be successful.
Case Description: We present the case of a herpes virus encephalitis that came up in the emergency department with an admission diagnosis of ischemic cerebral accident. Being the symptomatology unclear, the findings of magnetic resonance of the brain oriented versus an infectious disorder. The lumbar tap confirmed the presence of herpes simplex virus (HSV) 1 virus and an antiviral therapy was administered, leading to resolution of the condition within the 3 weeks of hospitalization.
Conclusion: HSV infections may mimic stroke and therefore should be included in the differential diagnosis of atypical acute nervous conditions. In neurological events of acute nature, especially in febrile patients whose brain imaging is suspicious or inconclusive, the eventuality of a herpetic encephalitis should be kept in mind. This will lead to a prompt antiviral therapy and to a favorable outcome.
Keywords: Brain imaging, Central nervous system infections, Encephalitis, Herpes virus, Stroke, Brain MRI
INTRODUCTION
Herpes simplex virus encephalitis (HSVE) is an infectious disease of the brain tissue which in most cases is caused by herpes simplex virus (HSV)-1, with an annual incidence ranging from 0.2 to 0.4/100,000 patients.[
CASE PRESENTATION
A 49-year-old male was presented to our emergency department as a stroke alert from another hospital of our country, with 2 h history of acute onset of aphasia and right hemiplegia. On neurological examination, the patient was alert, obeys commands, pupils had a diameter bilaterally of 4 mm and were both reactive to light, with right hemiplegia, motor aphasia, left head and eyes deviation, and right indifferent plantar reflex. There was no past history of fever nor seizures.
His wife referred that 3 months ago he experienced a transient ischemic attack with dysarthria, right hemiparesis and right hemihypesthesia which lasted 15 min, but he did not see any doctor and was left untreated. She also referred that 3 years ago, he was hospitalized and treated for meningitis but with no evidence or medical files at hand.
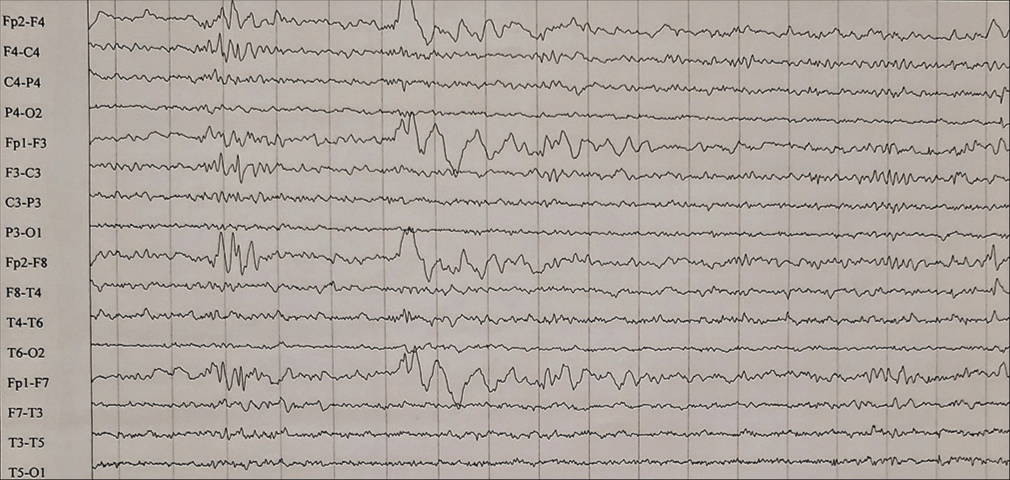
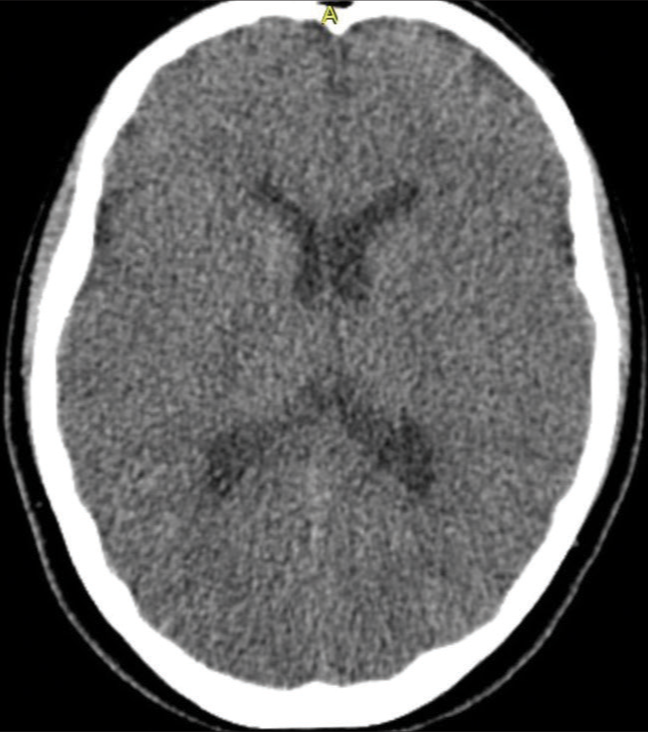
Regarding the fact that it had an acute onset, the clinical presentation was stroke-like, a head computed tomography (CT) scan was performed and after hemorrhage was excluded from the study, intravenous thrombolysis (IVT) with Alteplase was started. At 15 min of the procedure, we noticed mild gingival bleeding and infusion of Alteplase was interrupted. After the bleeding was stopped, the patient was stable hemodynamically and started perseverating only a few words. One hour later, he had an episode of explosive vomiting and shivering, and his body temperature started to increase to 37.5°C. Two hours later, a focal myoclonic seizure of right arm was observed; therefore, the patient was set under treatment with midazolam i/v.
Later on that day, fluctuations of clinical symptoms were observed, the patient became somnolent, opened eyes only after repetitive verbal stimulus, did not obey any command, and motor aphasia was present again. Even though he was treated with antipyretics, shivering did not stop, and he became febrile to 39.5°C, and irresponsive to treatment. Hemodynamically, he showed a hypotension (90/60 mmHg) and tachycardia 130 beats/min. Over the next 12 h, the myoclonic seizures became more frequent and they were generalized twice. He became more somnolent and opened eyes only to painful stimuli, and the only motor response seen was a flexion response of the right superior limb to pain. Viral encephalitis was suspected and empiric treatment with intravenous acyclovir was started for HSVE.
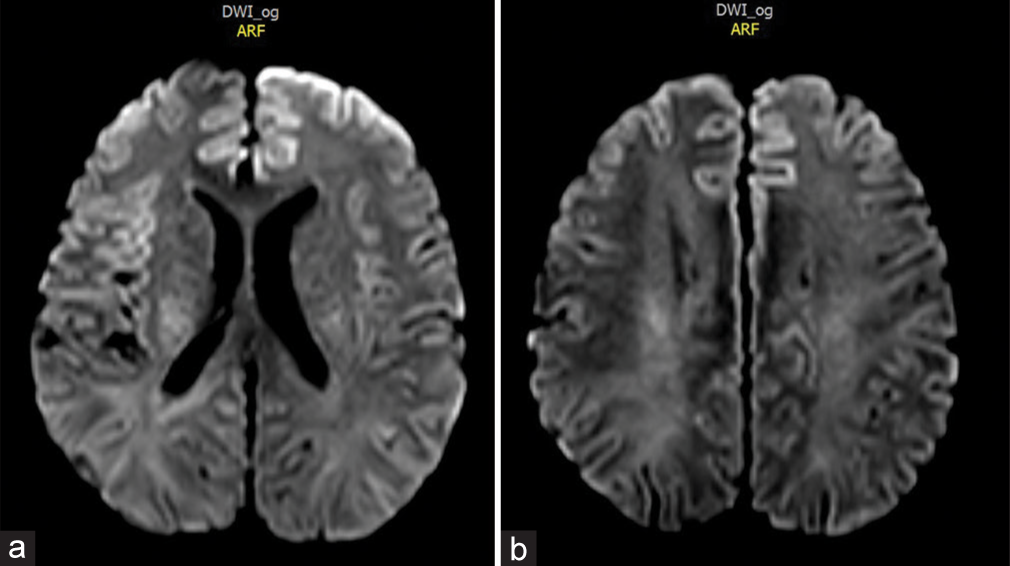
Brain magnetic resonance imaging (MRI) revealed a cortical enhancement in the left frontal lobe in the diffusion-weighted images (DWIs) [
The patient was treated with intravenous acyclovir for 21 days with a dose of 10 mg/kg 3 times daily, accordingly with suggested guidelines.[
DISCUSSION
HSVE can often have poor prognosis and is associated with significant morbidity and mortality (20–30%), despite prompt diagnosis and treatment.[
High index of clinical suspicion, prompt diagnosis, and early treatment are the mainstays of therapeutic success in herpetic encephalitis.[
Performing a lumbar puncture might be controversial if the patient has a thrombolysis recently; however, in our case, the CSF fluid was collected during the 3rd day of hospitalization. Instead, the thrombolysis was attempted upon admission and subsequently stopped due to gingival hemorrhage. The setting of a febrile patient, with unsatisfying response to antipyretics, while in a deeply confusing state and subsequent myoclonus, will raise the suspicion of a neuroinfection.
Since we are living in the SARS-CoV-2 era and several investigations have shown the involvement of the central nervous system along the course of the disease, with encephalitis being one of the occurrences, we must consider this virus as well. We excluded at the admission facility the possibility of a COVID-19 infection in our patient, through a Rapid test and a PCR test, which resulted both negative.[
Brain MRI is the imaging study of first choice, because it ensures a fast diagnosis and untangles HSVE from its mimics. Its typical findings are bilateral but asymmetrical involvement of frontotemporal lobes with cytotoxic edema, hemorrhage, or necrosis; however, in some cases, HSVE might develop unilateral lesions looking like ischemic stroke.[
As shown in our case and from a large database of other reports, when having a patient with unusual symptoms of stroke, HSVE must be under consideration as a differential diagnosis.
CONCLUSION
HSV is the most common cause of viral encephalitis and it might have a wide spectrum of clinical presentations. Rarely, it will mimic the clinical picture of an acute ischemic stroke.[
Among clinical caveats to mention and that would raise suspicion on a herpetic neuroinfection is the almost constant febrile nature of the occurrence, apart from the fluctuating neurological symptoms that sometimes characterize a transient ischemic attack. The latter is frequently missed on plain CT scan images; hence, the importance of a lumbar tap whenever there are clinical doubts. Of course, if thrombolysis is started, a delay of at least 48 h should separate this therapeutic intervention from the puncture to avoid unnecessary risks. This is valid also for patients while in treatment with oral anticoagulants, and algorithms suggesting the necessary diagnostic workup before performing the puncture are available, while evaluating carefully the risk/benefit ratio of the procedure.[
In all cases, an appropriate antiviral therapy could be started while waiting laboratory confirmation of the infective agent, to enhance the chances of a full recovery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ajith Kumar AK, Mendez MD, editors. Herpes simplex encephalitis. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. p.
2. Alwood B, Khan U. Herpes simplex virus-1 encephalitis mimicking an acute stroke. Neurology. 2020. 94: 2353
3. Benson PC, Swadron SP. Empiric acyclovir is infrequently initiated in the emergency department to patients ultimately diagnosed with encephalitis. Ann Emerg Med. 2006. 47: 100-5
4. Buerger KJ, Zerr K, Salazar R. An unusual presentation of herpes simplex encephalitis with negative PCR. BMJ Case Rep. 2015. 2015: bcr2015210522
5. Dupre CM, Libman R, Dupre SI, Katz JM, Rybinnik I, Kwiatkowski T. Stroke chameleons. J Stroke Cerebrovasc Dis. 2014. 23: 374-8
6. Islam MA, Cavestro C, Alam SS, Kundu S, Kamal MA, Reza F. Encephalitis in patients with COVID-19: A systematic evidence-based analysis. Cells. 2022. 11: 2575
7. Kargiotis O, Oikonomi K, Geka A, Psychogios K, Safouris A, Zis P. HSV-encephalitis resembling acute cerebral infarction in a patient with atrial fibrillation: Beware of stroke mimics. Neurologist. 2021. 27: 30-3
8. Küker W, Nägele T, Schmidt F, Heckl S, Herrlinger U. Diffusion-weighted MRI in herpes simplex encephalitis: A report of three cases. Neuroradiology. 2004. 46: 122-5
9. Liberman AL, Prabhakaran S. Stroke chameleons and stroke mimics in the emergency department. Curr Neurol Neurosci Rep. 2017. 17: 15
10. Patoulias D, Gavriiloglou G, Kontotasios K, Tzakri M, Keryttopoulos P, Koutras C. HSV-1 encephalitis: High index of clinical suspicion, prompt diagnosis, and early therapeutic intervention are the triptych of success-report of two cases and comprehensive review of the literature. Case Rep Med. 2017. 2017: 5320839
11. Puchhammer-Stöckl E, Presterl E, Croÿ C, Aberle S, PopowKraupp T, Kundi M. Screening for possible failure of herpes simplex virus PCR in cerebrospinal fluid for the diagnosis of herpes simplex encephalitis. J Med Virol. 2001. 64: 531-6
12. Rota E, Agosti S, Risso R, Morelli N. Lumbar puncture after direct oral anticoagulant (DOAC) reversal: A proposed algorithm for the emergency department. Intern Emerg Med. 2019. 14: 1175-9
13. Sabah M, Mulcahy J, Zeman A. Herpes simplex encephalitis. BMJ. 2012. 344: e3166
14. Sarton B, Jaquet P, Belkacemi D, de Montmollin E, Bonneville F, Sazio C. Assessment of magnetic resonance imaging changes and functional outcomes among adults with severe herpes simplex encephalitis. JAMA Netw Open. 2021. 4: e2114328
15. Shoaib M, Kraus JJ, Khan MT. Herpes simplex virus encephalitis: Atypical presentation as a right middle cerebral artery stroke. Cureus. 2018. 10: e2067
16. Sili U, Kaya A, Mert A. Herpes simplex virus encephalitis: Clinical manifestations, diagnosis and outcome in 106 adult patients. J Clin Virol. 2014. 60: 112-8
17. Stahl JP, Mailles A, De Broucker T. Herpes simplex encephalitis and management of acyclovir in encephalitis patients in France. Epidemiol Infect. 2012. 140: 372-81
18. Zinkstok SM, Engelter ST, Gensicke H, Lyrer PA, Ringleb PA, Artto V. Safety of thrombolysis in stroke mimics: Results from a multicenter cohort study. Stroke. 2013. 44: 1080-4