- Department of Pathology and Laboratory Medicine, University of California Davis Health, Sacramento, California,
- Department of Pathology, Foundation Medicine, Cambridge, Massachusetts, United States.
Correspondence Address:
Alexander Ladenheim, Department of Pathology and Laboratory Medicine, University of California Davis Health, Sacramento, California, United States.
DOI:10.25259/SNI_828_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alexander Ladenheim1, Ananya Datta Mitra1, Mirna Lechpammer2, Denis M. Dwyre1. Hidden treasures: Incidental findings in two cases of chronic subdural hematoma. 23-Jun-2022;13:267
How to cite this URL: Alexander Ladenheim1, Ananya Datta Mitra1, Mirna Lechpammer2, Denis M. Dwyre1. Hidden treasures: Incidental findings in two cases of chronic subdural hematoma. 23-Jun-2022;13:267. Available from: https://surgicalneurologyint.com/surgicalint-articles/11674/
Abstract
Background: Extramedullary hematopoiesis (EMH) and plasmacytomas occurring within the cranium are rare entities.
Case Description: We review two cases in which patients presented with subdural hematoma and underwent evacuation. On routine histopathologic examination of their membranes, both patients were subsequently found to have focal EMH, as well as a clonal plasma cell proliferation in one case.
Conclusion: EMH is rare and usually found in individuals with profound and chronic anemia. However, this entity may be more common in chronic subdural hematomas. Solitary extraosseous plasmacytoma is exceedingly rare in the cranium, and its presence in chronic subdural hematoma membranes is of uncertain significance. The cytokine milieu that promotes organization of chronic subdural hematomas may play a role in the establishment of both of entities in this location.
Keywords: Case report, Extramedullary hematopoiesis, Plasmacytoma, Subdural hematoma
INTRODUCTION
The routine microscopic examination of subdural hematoma membranes is typically unexciting beyond offering some information on the chronicity of the lesion. Here, we present two cases of subdural hematoma which were remarkable for focal clusters of ectopic cells, prompting further workup.
CASE PRESENTATIONS
Case 1
An 86-year-old female with a history of atrial fibrillation on anticoagulation was taken to an outside hospital emergency department after being found down in her home with encephalopathy. A CT scan of the head was performed which showed a 13 mm thick left-sided subdural hematoma with a rightward midline shift of 6 mm. She was then transferred to our institution for further management. Her anticoagulation was discontinued and she underwent reversal with an anti-inhibitor coagulant complex. Repeat imaging on admission showed no interval change. During her hospitalization, the patient’s mental status improved, and she was discharged to an inpatient rehabilitation facility.
Approximately 10 days later, follow-up CT head showed evidence of rebleeding with an interval increase in the size of the left subdural hematoma to 15 mm and an increase in the rightward midline shift to 8 mm [
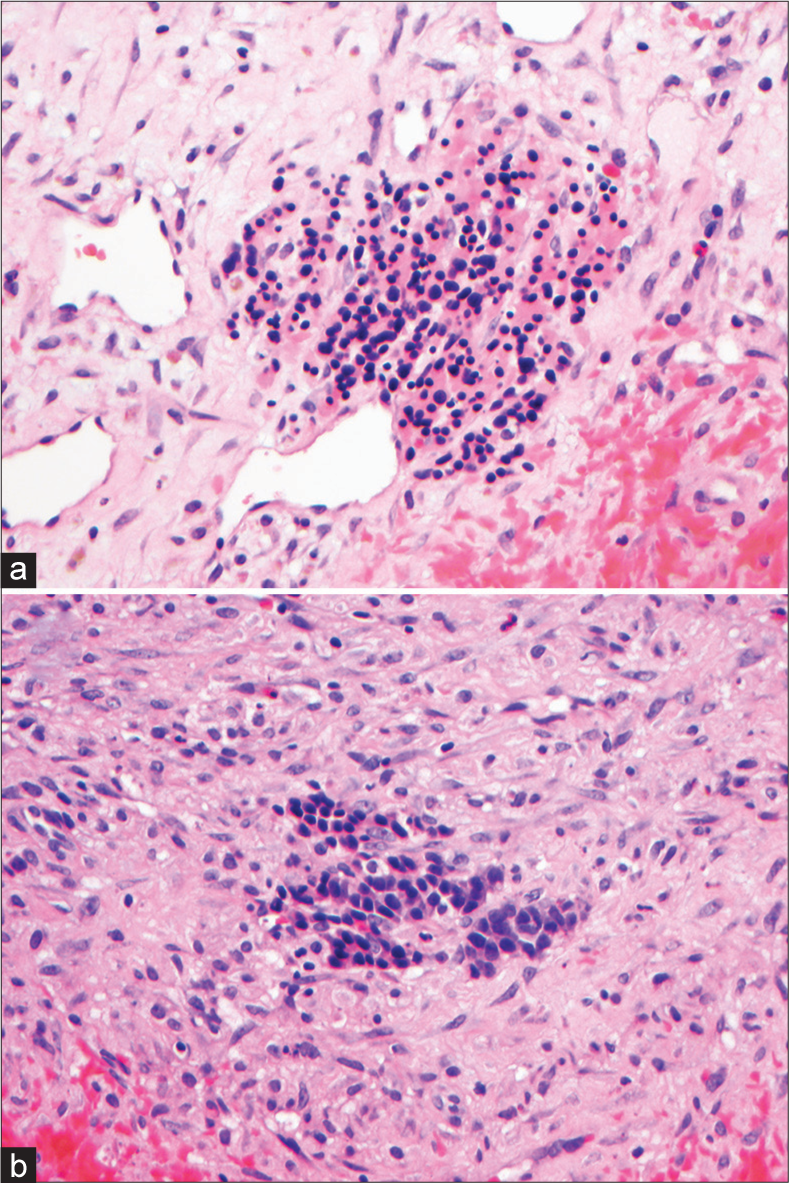
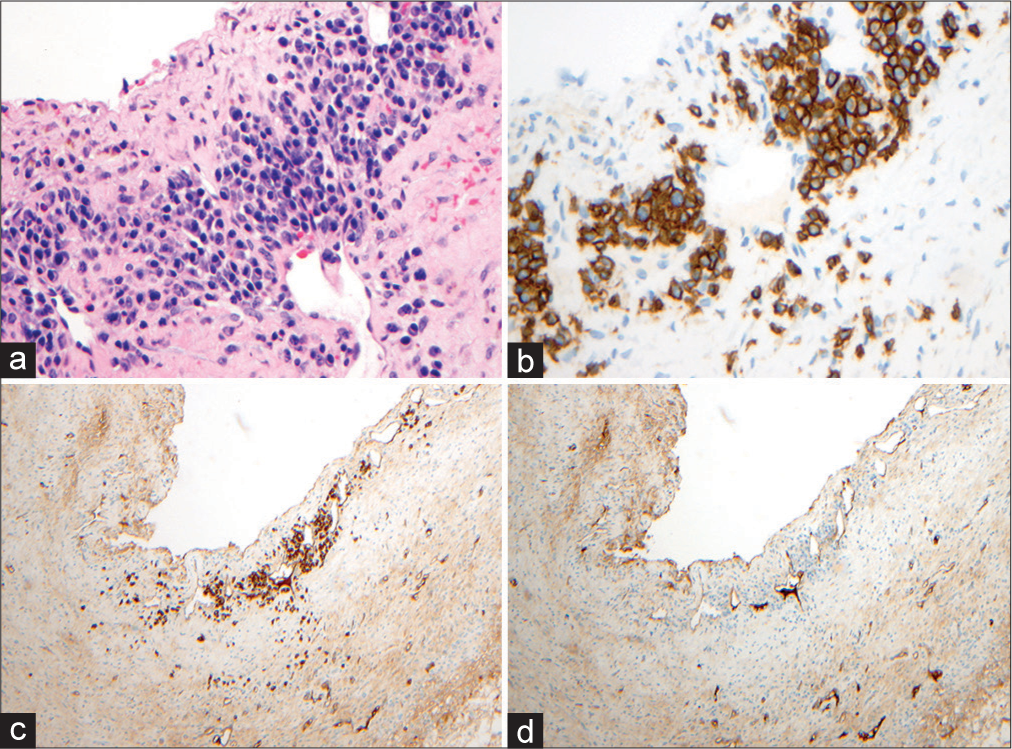
The specimen consisted of fragments of brown-red tissue measuring 6.7 × 4.5 × 1.6 cm in aggregate and was grossly consistent with a chronic and organized subdural hematoma. On microscopic examination, there were several small clusters of cells with the appearance of erythroid islands and immature mononuclear cells noted within the membranes [
In addition, in one tissue block, there was a cluster of cells morphologically resembling plasma cells [
Case 2
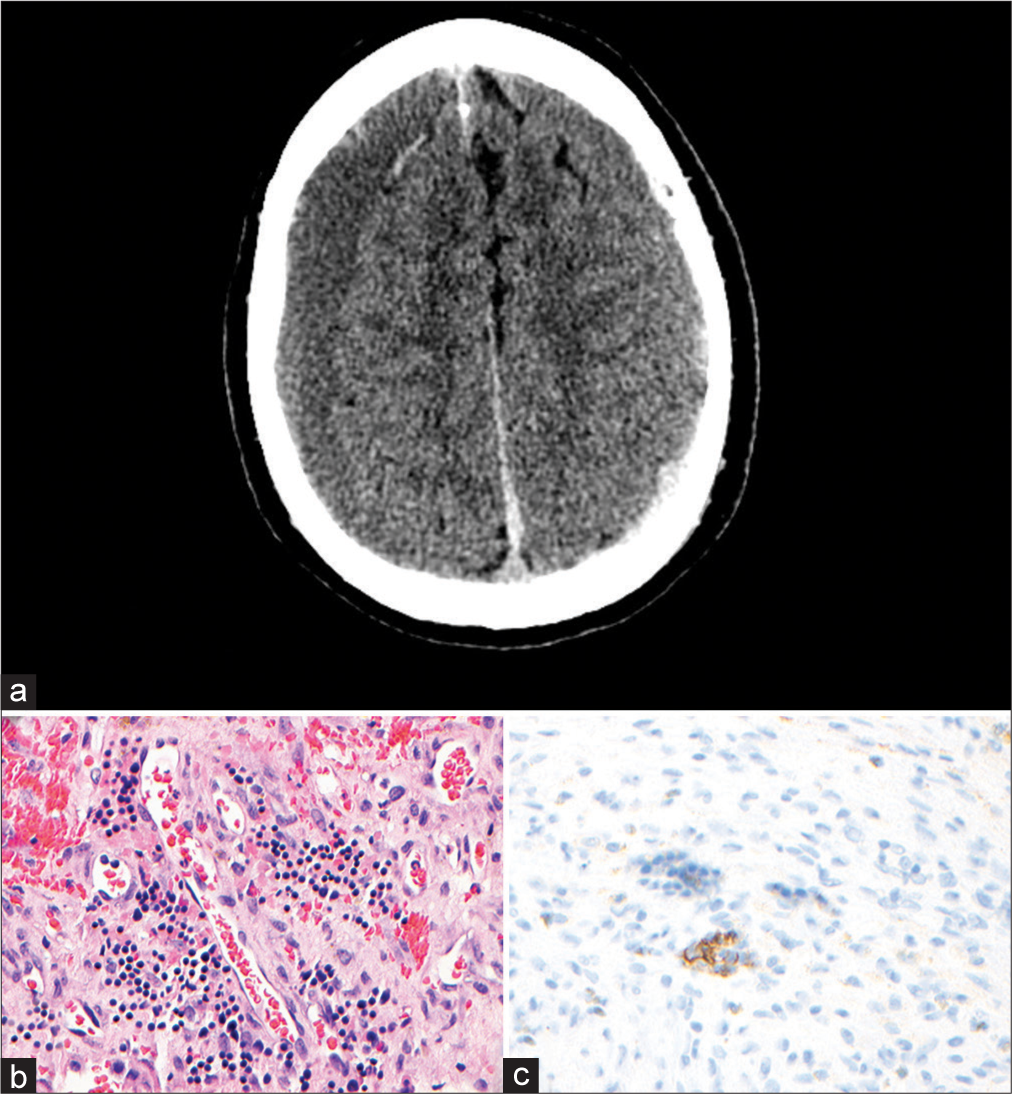
A 66-year-old male with diabetes presented with an 8-week history of chronic occipital headaches and tinnitus. The patient’s primary care physician obtained imaging of the brain which showed bilateral subacute-on-chronic subdural hematomas with 6 mm of the leftward midline shift [
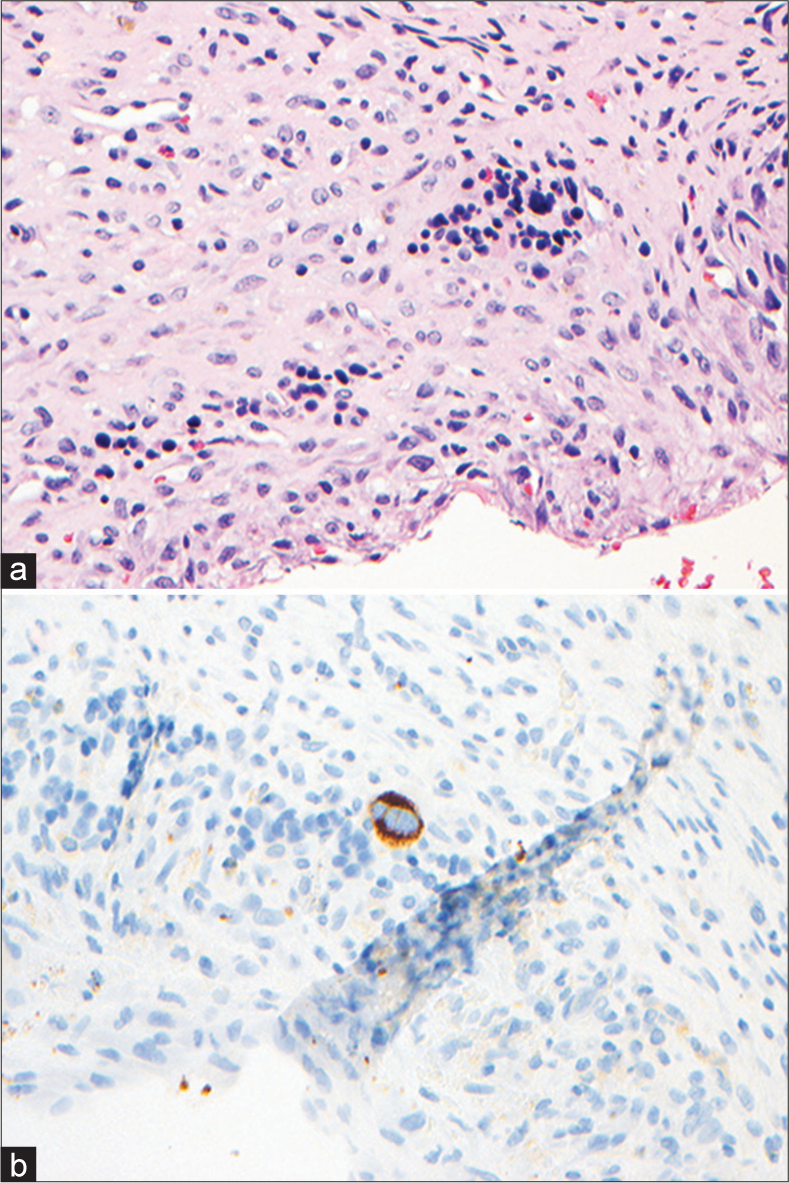
The specimen consisted of fragments of tan-brown, hemorrhagic, soft and membranous tissue measuring 2.7 × 2.0 × 0.4 cm in aggregate grossly consistent with a chronic and organized subdural hematoma. On microscopic examination, there were several erythroid islands noted [
DISCUSSION
These routine subdural hematoma specimens both revealed ectopic clusters of cells that were striking enough to prompt further workup. Both EMH and plasmacytomas are most commonly encountered in the bone or marrow elements, and their presence in the cranium is rare. Below is a brief review of the phenomena of intracranial EMH and intracranial plasmacytomas occurring in chronic subdural hematomas.
Intracranial EMH arising in the dura is very uncommon. It has been described in individuals with chronic anemia, including patients with thalassemia and myeloproliferative neoplasms. [
Several hypotheses have been put forward to explain this phenomenon. In one case, the patient’s subdural hematoma occurred in proximity to a skull fracture and the authors suggested that local extravasation of marrow elements into the hematoma might account for EMH.[
Intracranial solitary extraosseous plasmacytomas (SEP) are very rare. They have occasionally been reported to arise in the dura or brain parenchyma, coming to clinical attention by detection on imaging or by causing mass effect.[
Because SEPs in general present a modest rate of recurrence (25%) and occasionally progress to plasma cell myeloma (15%),[
It is also worth reflecting on whether these foci of EMH and the possible SEP within this patient’s subdural hematoma have a common origin. The formation of a chronic subdural hematoma is driven by inflammation mediated by an array of cytokines.[
CONCLUSION
Intracranial EMH is rare and usually found in individuals with profound and chronic anemia. However, this phenomenon may be more common in chronic subdural hematomas; despite their intracranial location, the cytokine milieu that promotes organization of chronic subdural hematomas may play a role in the establishment of foci of EMH. SEP is exceedingly rare in the cranium; the incidental finding of a minute, clonal plasma cell proliferation in the chronic subdural hematoma of Case 1 is of unknown significance and deserves further study because of the known risk of recurrence and progression in SEP of other sites, ultimately, to plasma cell myeloma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Duerinck J, Van Rompaey K, Moens M, Ampe B, De Smet K, Michotte A. Development of dural plasmacytoma after evacuation of chronic subdural hematoma: Case report. Clin Neurol Neurosurg. 2012. 114: 1322-5
2. Edlmann E, Giorgi-Coll S, Whitfield PC, Carpenter KL, Hutchinson PJ. Pathophysiology of chronic subdural haematoma: Inflammation, angiogenesis and implications for pharmacotherapy. J Neuroinflammation. 2017. 14: 108
3. Eskazan AE, Ar MC, Baslar Z. Intracranial extramedullary hematopoiesis in patients with thalassemia: A case report and review of the literature. Transfusion. 2012. 52: 1715-20
4. Firsching R, Müller W, Thun F, Boop F. Clinical correlates of erythropoiesis in chronic subdural hematoma. Surg Neurol. 1990. 33: 173-7
5. Kuhn E, Dorji T, Rodriguez J, Rosai J. Extramedullary erythropoiesis in chronic subdural hematoma simulating metastatic small round cell tumor. Int J Surg Pathol. 2007. 15: 288-91
6. Li R, Reddy VB, Palmer CA. Extramedullary hematopoiesis: An unusual finding in subdural hematomas. Case Rep Pathol. 2011. 2011: 718585
7. Mehta S, Shapey J, Pohl U, Vindlacheruvu R. Intracranial extramedullary haematopoiesis: A case report. Br J Neurosurg. 2015. 29: 734-6
8. Moens L, Tangye G. Cytokine-mediated regulation of plasma cell generation: IL-21 takes center stage. Front Immunol. 2014. 5: 65
9. Müller W, Zimmermann E, Firsching R. Erythropoiesis in chronic subdural haematomas. Acta Neurochir (Wien). 1988. 93: 137-9
10. Slater JP. Extramedullary hematopoiesis in a subdural hematoma. Case report. J Neurosurg. 1966. 25: 211-4
11. Stanisic M, Aasen AO, Pripp AH, Lindegaard KF, RammPettersen J, Lyngstadaas SP. Local and systemic pro-inflammatory and anti-inflammatory cytokine patterns in patients with chronic subdural hematoma: A prospective study. Inflamm Res. 2012. 61: 845-52
12. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H.editors. WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. Lyon, France: International Agency for Research on Cancer; 2017. p. 241-58
13. Weidenheim KM, Campbell WG, Goldman HW. Atypical monoclonal plasma cell hyperplasia of the central nervous system: Precursor of plasmacytoma with evolutionary considerations. Neurosurgery. 1989. 24: 429-34