- Department of Neurosurgery, Desert Regional Medical Center, Palm Springs, California, United States.
- College of Osteopathic Medicine, William Carey University, Hattiesburg, Mississippi, United States.
Correspondence Address:
Brian Fiani, D.O. Department of Neurosurgery, Desert Regional Medical Center, Palm Springs, California, United States.
DOI:10.25259/SNI_1046_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rebecca Houston1, Brian Fiani1, Brian Musch2, Emilio Tayag1. Holocord spontaneous pneumorrhachis in the setting of refractory emesis. 08-Dec-2021;12:602
How to cite this URL: Rebecca Houston1, Brian Fiani1, Brian Musch2, Emilio Tayag1. Holocord spontaneous pneumorrhachis in the setting of refractory emesis. 08-Dec-2021;12:602. Available from: https://surgicalneurologyint.com/surgicalint-articles/11271/
Abstract
Background: Pneumorrhachis (PNR) is the presence of air within the spinal canal and may be either intramedullary or extramedullary in location. The etiology is most commonly iatrogenic or traumatic in nature. Treatment is dependent on underlying cause and physical exam.
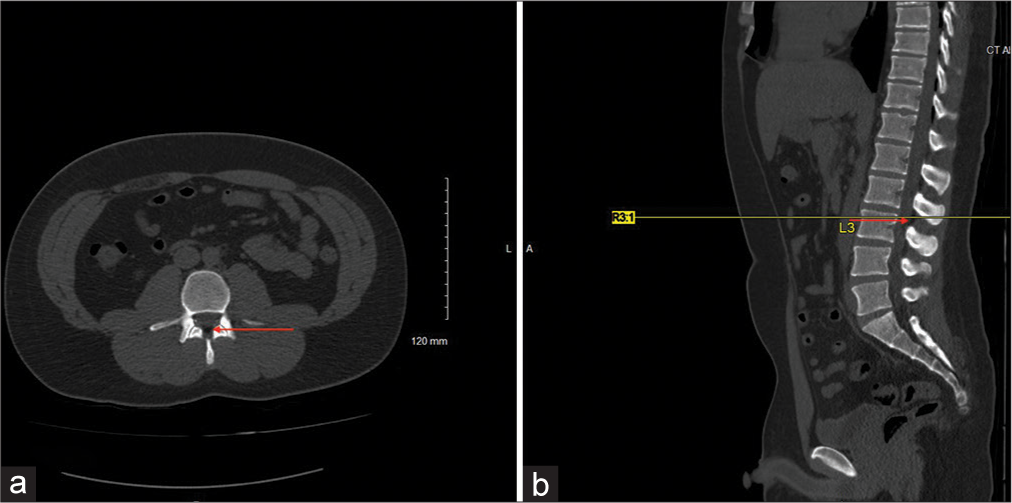
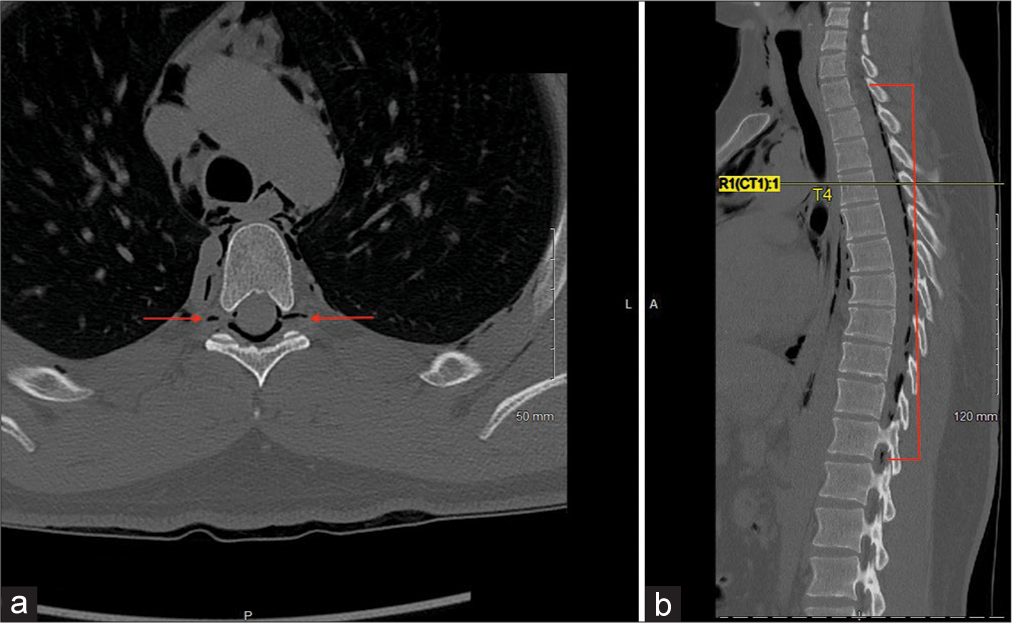
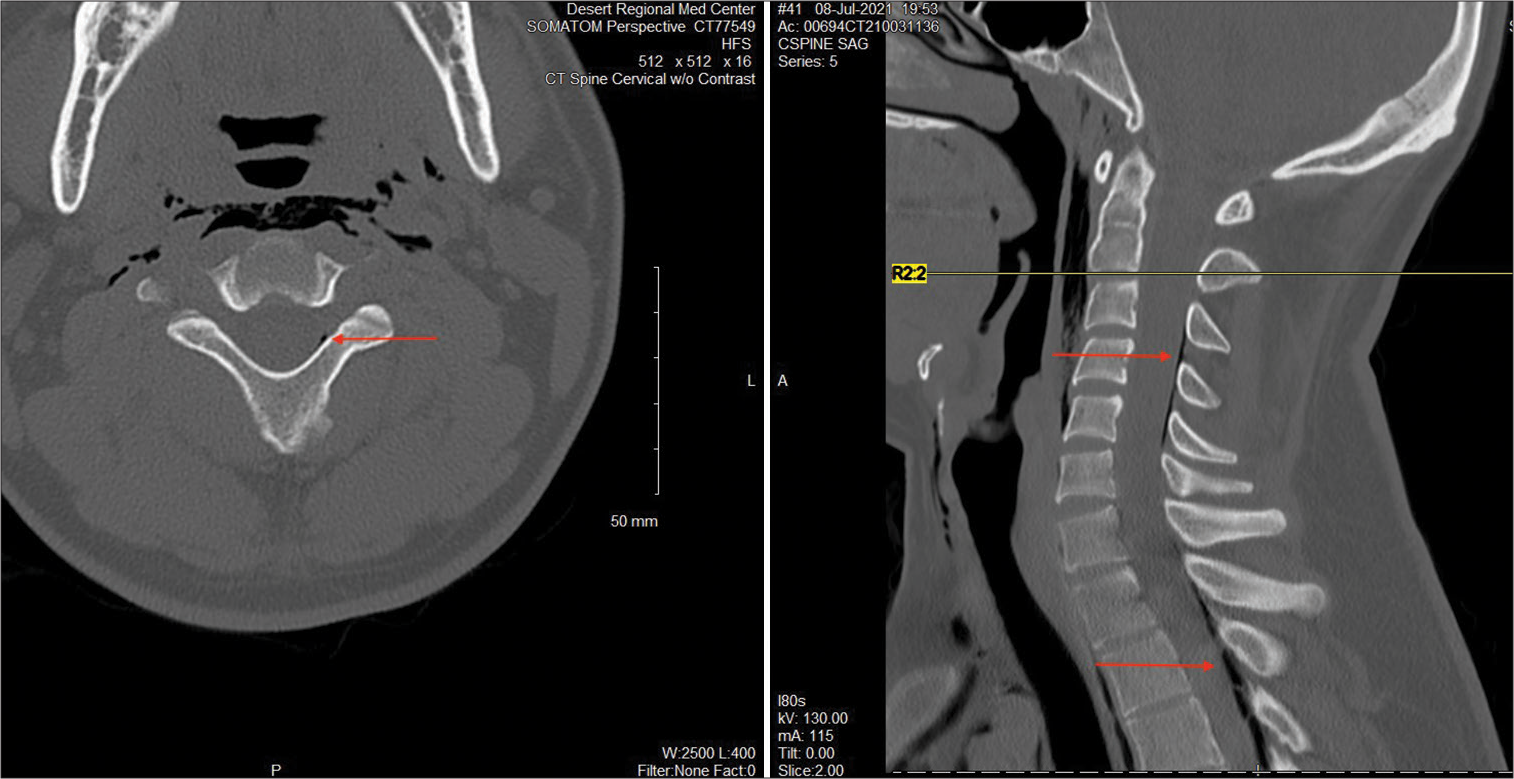
Case Description: Herein, we describe the second case in the literature of spontaneous holocord PNR in a young patient without risk factors. A 22-year-old male with no past medical history presented to the hospital for 2 days of vomiting and cramping in his hands and feet secondary to severe dehydration. He recently started a new job as a manual laborer and had to leave work early 2 days prior due to overexertion working outside in heat ranging from 100 to 120 degrees Fahrenheit. CT abdomen and pelvis demonstrated spontaneous pneumomediastinum and extramedullary PNR extending upward from L3 throughout the thoracic spine to the upper limit of the scan. Subsequent CT cervical and thoracic spine showed the full length of the extradural air from C2-T12 and again at L3.
Conclusion: Spontaneous PNR is an uncommon, typically self-limited condition in which air is introduced into the spinal axis. Anatomic predisposition makes the extradural, dorsal cord in the cervicothoracic region the most common location. Patients are rarely symptomatic, and treatment is supportive in nature once secondary causes with high rates of morbidity and mortality are ruled out.
Keywords: Holocord, Intraspinal air, Pneumomediastinum, Pneumorrhachis
INTRODUCTION
Pneumorrhachis (PNR) is the presence of air within the spinal canal and may be either intramedullary or extramedullary in location. The etiology is most commonly iatrogenic or traumatic in nature, though it is not uncommon for no definitive cause to be identified. Certain acute and chronic conditions predispose patients to the development of PNR including asthma, Valsalva maneuvers such as coughing, emesis and lifting heaving objects, respiratory infections and airway obstruction or perforation.
There is no established definition of spontaneous PNR in the literature. However, classification of pneumomediastinum as spontaneous has historically been defined as the absence of history of trauma and/or iatrogenic cause.[
There are no published statistics in the literature regarding epidemiology of spontaneous PNR as there is no agreed-on definition. Most non-iatrogenic and non-traumatic cases of PNR are asymptomatic. When patients do have symptoms, they are often caused by associated conditions such as pneumomediastinum and subcutaneous emphysema causing chest pain, dyspnea, dysphagia and neck pain.[
CASE DESCRIPTION
A 22-year-old male with no past medical history presented to the hospital for 2 days of vomiting and cramping in his hands and feet secondary to severe dehydration. He recently started a new job as a manual laborer and had to leave work early 2 days prior due to overexertion working outside in heat ranging from 100 to 120 degrees Fahrenheit. CT abdomen and pelvis (later reconstructed into CT lumbar spine) demonstrated spontaneous pneumomediastinum and extramedullary PNR extending upward from L3 throughout the thoracic spine to the upper limit of the scan [
The patient was admitted for completion of gastrografin esophagram which was negative for evidence of esophageal perforation. He was discharged home the day after presentation. At 3-week follow-up, the patient remained without neurological compromise.
DISCUSSION
PNR is a rare phenomenon in which there is air the spinal canal either outside the cord or within the spinal cord itself. Extradural location is most common.[
Notably, in PNR, while air is most commonly located in the posterior spinal canal because of decreased resistance compared to the anterior epidural space which houses a denser vascular network, this patient demonstrated air in the anterior portion of the canal, proximal to the disc space. Air-filled facet cysts have also been proposed as a possible cause of PNR.[
There are no pathognomonic signs or symptoms associated with PNR. There have been cases reported with neurological symptoms in the setting of iatrogenic and traumatic PNR secondary to cord compression. However, in spontaneous PNR, patients are there exists only two cases in the literature in which a patient had signs or symptoms of neurological compromise; in all other cases, patients were either asymptomatic, or complained of symptoms associated with their predisposing condition or those associated with pneumomediastinum, such as chest pain, dyspnea, dysphagia, neck pain, and cough.[
Classification of pneumomediastinum as spontaneous has historically been defined as the absence of history of trauma and/or iatrogenic cause.[
In our review of the literature for cases of truly spontaneous PNR without predisposing acute or chronic conditions (such as acute respiratory illness or asthma), we found that the location of the air most commonly found in the cervicothoracic spine, with the cervical spine, alone as the next most common location The predilection for the cervical spine has an anatomical explanation; there is no fascial barrier between the posterior mediastinum and the cervical epidural space. As such, air can diffuse into the epidural space in this region if it already exists in the posterior mediastinum compartment.[
Treatment for spontaneous, asymptomatic PNR is most commonly geared towards treatment of the underlying condition. In the context of spontaneous pneumomediastinum, this often means supportive care measures such as bed rest, oxygen supplementation, high-flow oxygen therapy, analgesia and in some cases, systemic corticosteroids.[
CONCLUSION
We present a case of spontaneous PNR diagnosed through CT in a patient with no known risk factors. There exist no guidelines for treatment of spontaneous PNR, which is often an incidental finding. As previously mentioned, all except two cases of spontaneous PNR in the literature were asymptomatic. As such, healthcare provider efforts should be directed at ruling out underlying dangerous complications of spontaneous pneumomediastinum and underlying causes of PNR, such as tension pneumomediastinum, pneumopericardium, pneumothorax, tracheal tear and Boerhaave syndrome. If no underlying cause is diagnosed and patient remains asymptomatic, the patient should be monitored under an outpatient status with observation. Serial imaging should be reserved for changes in exam or symptoms that could be related.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alemu BN, Yeheyis ET, Tiruneh AG. Spontaneous primary pneumomediastinum: Is it always benign?. J Med Case Rep. 2021. 15: 157
2. Al-Mufarrej F, Gharagozloo F, Tempesta B, Margolis M. Spontaneous cervicothoracolumbar pneumorrhachis, pneumomediastinum and pneumoperitoneum. Clin Respir J. 2009. 3: 239-43
3. Bally K, Leikin S, Margetis K, Reynolds AS. Extensive pneumorrhachis after spontaneous pneumomediastinum. World Neurosurg. 2020. 142: 392-5
4. Behr G, Mema E, Costa K, Garg A. Proportion and clinical relevance of intraspinal air in patients with pneumomediastinum. AJR Am J Roentgenol. 2018. 211: 321-6
5. Eroglu U, Yakar F, Zaimoglu M, Ozates O, Ozgural O, Ugur HC. Pneumorrhachis. Asian J Neurosurg. 2016. 11: 172-3
6. Heckman AJ, Mohseni M, Villanueva A, Cowart JB, Graham CG. Concurrent spontaneous pneumomediastinum and pneumorrhachis. J Emerg Med. 2018. 54: e117-20
7. Kono T, Kuwashima S, Fujioka M, Kobayashi C, Koike K, Tsuchida M. Epidural air associated with spontaneous pneumomediastinum in children: Uncommon complication?. Pediatr Int. 2007. 49: 923-7
8. Kumaran SP, Gupta K, Singh SS. A rare association of spontaneous pneumorrhachis with spondylolisthesis and lumbosacral vacuum phenomenon: A case report with review of literature. Neurol India. 2011. 59: 120-1
9. Martins L, Dionisio P, Moreira S, Manique A, Correia I, Barbara C. An unusual association in an uncommon disease: Two cases of spontaneous pneumomediastinum associated with pneumorrhachis. Case Rep Pulmonol. 2016. 2016: 5092157
10. Migeot M, Kessler R, Etxeberria Izal A, Rutgers MP, Gille M. Pneumorrhachis associated with a spontaneous pneumomediastinum. Rev Neurol (Paris). 2013. 169: 173-4
11. Oertel MF, Korinth MC, Reinges MH, Krings T, Terbeck S, Gilsbach JM. Pathogenesis, diagnosis and management of pneumorrhachis. Eur Spine J. 2006. 15: 636-43
12. Ramasamy P, Kale SB, Subramaniam S, Giridhar K. Recurrent spontaneous pneumomediastinum with concurrent pneumorrhachis: A rare clinical entity. Ann Thorac Surg. 2018. 105: e155-7
13. Rodrigues J, Costa RM, Magalhaes J, Santos E. Spontaneous pneumomediastinum and pneumorrhachis in a healthy girl. BMJ Case Rep. 2021. 14: e241077
14. Silva JB, Lira J, Ferreira G, Rodrigues J. Pneumorrhachis: A finding in spontaneous pneumomediastinum. An Pediatr (Engl Ed). 2019. 90: 323-4
15. Song KJ, Lee KB. Spontaneous extradural pneumorrhachis causing cervical myelopathy. Spine J. 2009. 9: e16-8
16. Valiyakath D, Al Busaidi T, Al Shamsi S, Al Sawafi Y. Pneumorrhachis with spontaneous pneumomediastinum: Should it raise special concerns?. Oman Med J. 2018. 33: 256-9