- Department of Neurosurgery, National Defense Medical College, Tokorozawa, Saitama, Japan
Correspondence Address:
Naoki Otani
Department of Neurosurgery, National Defense Medical College, Tokorozawa, Saitama, Japan
DOI:10.4103/sni.sni_169_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takashi Fujii, Naoki Otani, Satoru Takeuchi, Terushige Toyooka, Kojiro Wada, Kentaro Mori. Horizontal distance of anterior communicating artery aneurysm neck from anterior clinoid process is critically important to predict postoperative complication in clipping via pterional approach. 22-Aug-2017;8:200
How to cite this URL: Takashi Fujii, Naoki Otani, Satoru Takeuchi, Terushige Toyooka, Kojiro Wada, Kentaro Mori. Horizontal distance of anterior communicating artery aneurysm neck from anterior clinoid process is critically important to predict postoperative complication in clipping via pterional approach. 22-Aug-2017;8:200. Available from: http://surgicalneurologyint.com/surgicalint-articles/horizontal-distance-of-anterior-communicating-artery-aneurysm-neck-from-anterior-clinoid-process-is-critically-important-to-predict-postoperative-complication-in-clipping-via-pterional-approach/
Abstract
Background:The difficulty of clipping aneurysm of the anterior communicating artery (AcomA) depends on the size, direction, positional relationship with the parent artery, and height from the anterior frontal base. Cases of clipping unruptured AcomA aneurysm through pterional approach were analyzed to investigate the importance of the horizontal distance from the base of the anterior clinoid process.
Methods:Twenty-six consecutive unruptured AcomA aneurysms were treated by clipping through pterional approach in 10 males and 11 females aged 37–77 years (mean 61.8 years). Size and direction of the aneurysm, and vertical distance from the anterior frontal base and horizontal distance from the base of the anterior clinoid process were measured by preoperative three-dimensional computed tomography angiography (3D-CTA). Correlations with occurrence of clinical complications and computed tomography (CT) abnormalities after operation were investigated.
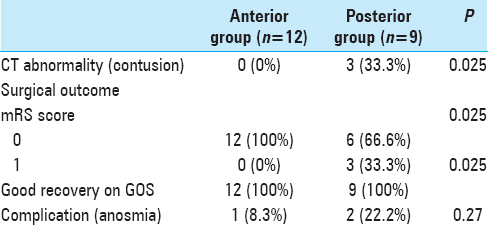
Results:The aneurysms had a mean size of 4.7 mm (range 2.1–8.9 mm). Three patients suffered complications and all had anosmia. Three patients had CT abnormality and all were contusion. The mean horizontal distance from the base of the anterior clinoid process was −4.7 mm (range −12.3–3.5 mm). The patients were divided into the anterior and posterior groups with the boundary set at −5 mm. There were no significant complications between two groups (P = 0.26). There were statistically significant CT abnormalities in posterior group (P = 0.025).
Conclusion:The horizontal distance from the base of the anterior clinoid process is important to predict CT abnormalities and complications in clipping of AcomA aneurysm through pterional approach.
Keywords: Anterior communicating artery aneurysm, clipping, surgical approach, surgical outcome
INTRODUCTION
Clipping of anterior communicating artery (AcomA) aneurysm can be performed through the pterional or interhemispheric approach. The difficulty of clipping AcomA aneurysm depends on the aneurysm size, direction, positional relationship with the parent artery, and height from the anterior frontal base.[
The present study investigated the correlation between horizontal distance from the base of the anterior clinoid process to the neck of the AcomA aneurysm, and the occurrence of complications and abnormality on computed tomography after clipping via the pterional approach.
MATERIALS AND METHODS
This study was approved by the Institutional Review of National Defense Medical College Hospital. Written informed consent was waived because of the retrospective design.
A retrospective analysis was conducted on the clinical and radiological data of AcomA that have been clipped in our institution between 2006 and 2016. The pterional approach was used with relatively small size, low height from the anterior frontal base, and dome projection not posterior. The size was smaller than 10 mm, and the height from anterior frontal base was lower than 13 mm. In other cases, we performed interhemispheric approach. Preoperative head 3D-CTA was performed to measure the aneurysm dome and neck size, distance in the vertical direction from the anterior frontal base to the neck of the aneurysm, and distance in the horizontal direction from the base of the anterior clinoid process to the neck of the aneurysm [
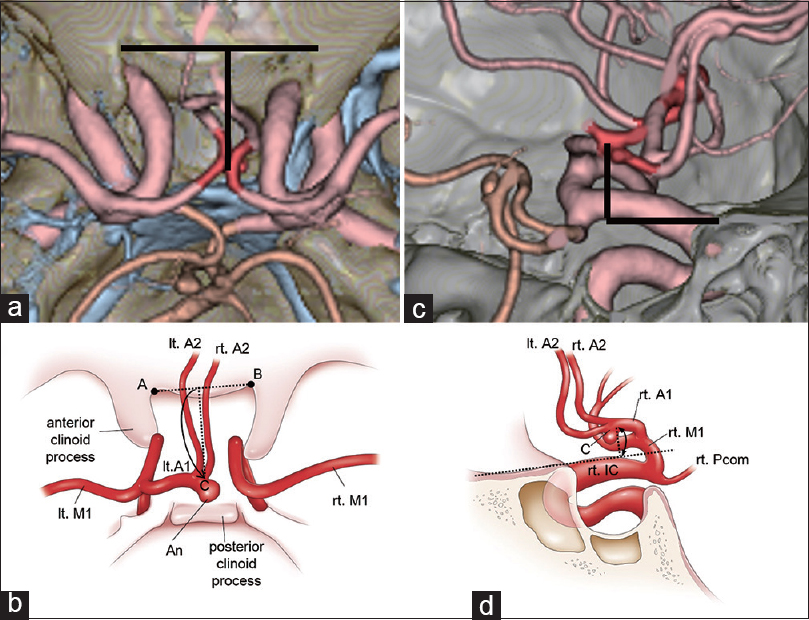
Figure 1
Preoperative CT angiograms (a and c) and the schematic diagrams (b and d) to measure the distance in the horizontal direction from the base of the anterior clinoid process to the neck of the aneurysm (a and b), and the distance in the vertical direction from the anterior frontal base to the neck of the aneurysm (c and d). a = left base of the anterior clinoid process; b = right base of the anterior clinoid process; c and d = aneurysm neck; ACP = anterior clinoid process; PCP = posterior clinoid process
Frontotemporal craniectomy, sphenoid ridge removal, dura arcuate incision, and sylvian fissure opening were performed in nearly all cases. The aneurysm was then identified via the pterional approach and part of the rectal gyrus was partially aspirated if needed. Intraoperative fluorescence angiography with indocyanine green was used to monitor the completeness of clipping.
Comparisons between groups used the student's t-test and Chi-square test with Statcel (OMS Ltd, Tokyo, Japan). Significant difference was defined at the P < 0.05 level.
RESULTS
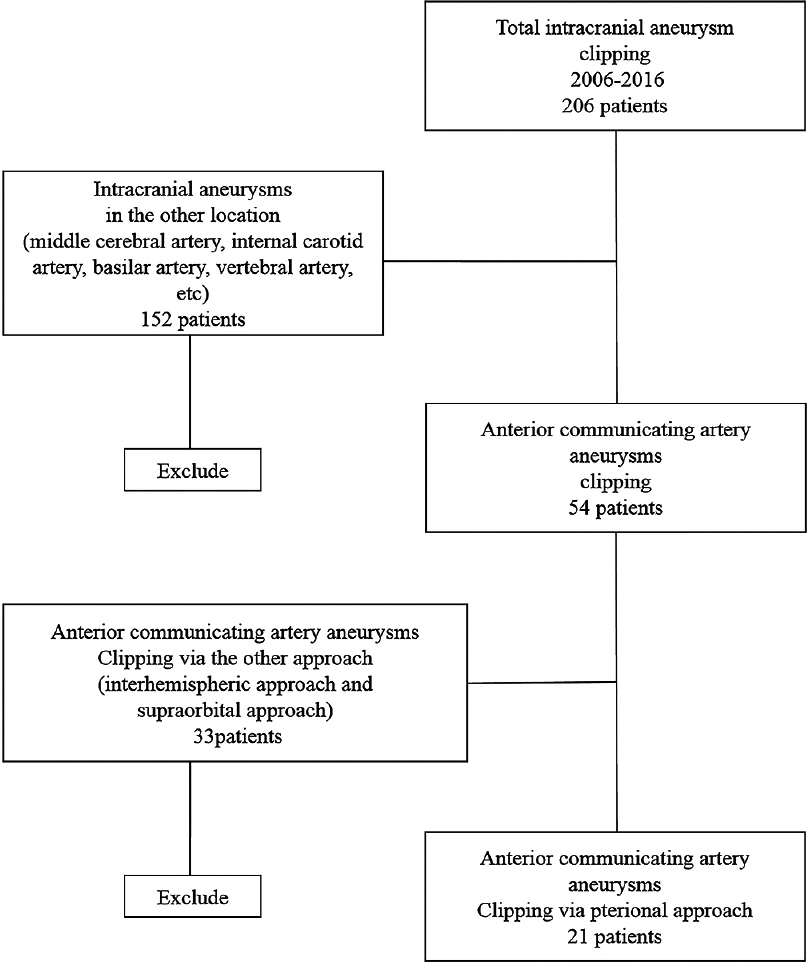
This study reviewed 206 cases of clipping of unruptured aneurysm in our institution between May 2006 and June 2016. A total of 54 (26.2%) cases involved AcomA aneurysm and 152 (73.8%) cases involved other locations. The pterional approach was performed to clip 21 (38.9%) aneurysms, and the interhemispheric approach or supraorbital approach was performed to clip 33 aneurysms (61.1%) [
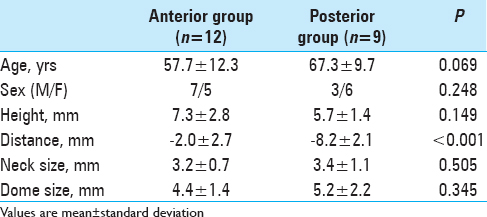
There were no multiple aneurysms. All aneurysms were saccular type. There were 10 males (47.6%) and 11 female patients (52.4%). The mean age was 61.8 years (range 37 to 77 years). The AcomA aneurysms had a mean size of 4.7 mm (range 2.1–8.9 mm) and mean neck size of 3.3 mm (range 1.3–4.7 mm). The mean distance from the base of the anterior clinoid process was −4.7 mm (range −12.3–3.5 mm). The patients were divided into the anterior and posterior groups with the boundary set at −5 mm [
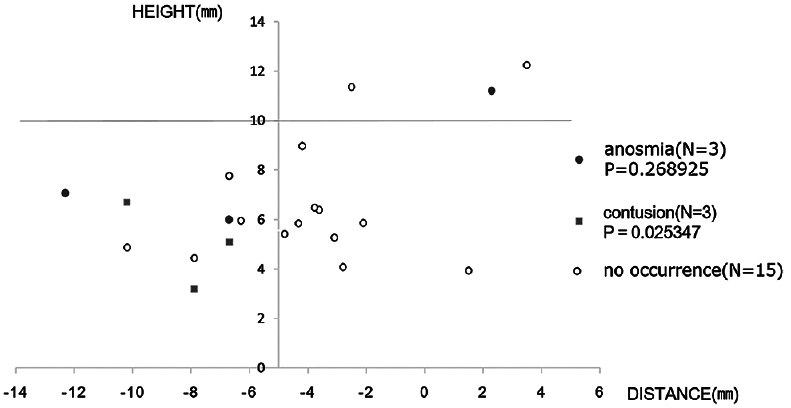
Figure 3
Plot of distance from the anterior frontal base and from the base of the anterior clinoid process. The boundary between the anterior and posterior groups was set at −5 mm from the base of the anterior clinoid process. The posterior group tends to include cases of complications (circles, N = 3) such as anosmia and CT abnormality (squares, N = 3). Open circles show normal cases (N = 15). Height = distance between the aneurysm neck and the anterior frontal base; distance = distance between the aneurysm neck and base of the anterior clinoid process
Three patients (14.3%) suffered complications and all were anosmia. Three patients had CT abnormality (14.3%) and all were frontal base contusion. Two out of three patients with anosmia were included in the posterior group. All 3 patients with contusion were included in the posterior group, with significant difference compared with the anterior group (P = 0.025) [
DISCUSSION
A retrospective was conducted on the clinical and radiological data of AcomA that have been clipped via pterional approach in our institution between 2006 and 2016. The aim of this study is to investigate the importance of the horizontal distance of aneurysmal neck from the base of anterior clinoid process to clip via pterional approach. We evaluate the correlation between the horizontal distance of aneurysmal neck from the base of anterior clinoid process by preoperative 3D-CTA and the neurological findings at the time of discharge and the postoperative CT abnormality. The anterior clinoid process has some variation such as interosseous bridge and caroticoclinoid process foramen. Each size of the anterior clinoid process is also broken. However, we choose the base of the anterior clinoid process as the measuring point because it was not affected by these factors above and can be easily measured by 3D-CTA. The result of this study suggests that clipping of aneurysms located far from base of anterior clinoid process in horizontal distance via pterional approach tend to have complications.
The location of AcomA aneurysm is surrounded with important anatomical structures. In particular, attention is required during surgery to preserve the parent arteries such as the bilateral A1 and A2 and perforators such as the hypothalamic artery and Heubner artery. The difficulty of clipping AcomA aneurysm depends on the aneurysm size, dome projection, height from the anterior frontal base, and relationship with the parent artery.[
Minimum retraction of the frontal lobe and exposure of AcomA complex are required to ensure preservation of the important vessels during clipping via the pterional approach. We need to retract the frontal lobe more if the aneurysm location is high or posterior. However, excessive retraction has been known to cause contusion or anosmia,[
Out study has two limitation. First, our retrospective study has inherent limitations. As with all retrospective studies, our results are susceptible to information bias such as interview is underestimated. Second, because we obtained patients from single center and only included clipping Acom aneurysms via the pterional approach, the number of lesions was relatively small.
The height of the AcomA aneurysm neck has been discussed from the points of difficulty in clipping or choice of approach. The present study has demonstrated that the horizontal neck location is critical to predict the occurrence of postoperative complications in AcomA aneurysm clipping via the pterional approach. The boundary between the anterior and posterior groups was set at −5 mm from the base of the anterior clinoid process. The posterior group tended to develop more complications, and significantly more postoperative head CT abnormalities. Therefore, we suggest that AcomA aneurysm with posterior location should be clipped via the interhemispheric approach, or via the pterional approach with intentionally wide opening of the sylvian fissure.
CONCLUSION
Preoperative measurement of the horizontal distance of AcomA from the base of the anterior clinoid process, as well as aneurysm height, is important in the selection of the optimum approach for clipping.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Funding
This research did not been receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aydin IH, Kadioğlu HH, Tüzün Y, Kayaoğlu CR, Takçi E, Oztürk M. Postoperative anosmia after anterior communicating artery aneurysms surgery by the pterional approach. Minim Invasive Neurosurg. 1996. 39: 71-3
2. Ciołkowski M, Michalik R, Ciszek B. Arteries to the proximal part of the olfactory tract. Folia Morphol (Warsz). 2004. 63: 455-8
3. Dehdashti AR, Chiluwal AK, Regli L. The implication of anterior communicating complex rotation and 3-dimensional comuputerized tomography angiography findings in surgical approach to anterior communicating artery aneurysms. World Neurosurg. 2016. 91: 34-42
4. Fujiwara H, Yasui N, Nathal-Vera E, Suzuki A. Anosmia after anterior communicating artery aneurysm surgery: Comparison between the anterior interhemispheric and basal interhemispheric approaches. Neurosurgery. 1996. 38: 325-8
5. Futami K, Nakada M, Iwato M, Kita D, Miyamori T, Yamaashita J. Simulation of clipping position for cerebral aneurysms using three-dimensional computed tomography angiography. Neurol Med Chir. 2004. 44: 6-12
6. Hayashi N, Sato H, Akioka N, Kurosaki K, Hori S, Endo S. Unilateral anterior interhemispheric approach for anterior communicating artery aneurysms with horizontal head position-technical note. Neurol Med Chir (Tokyo). 1996. 51: 160-3
7. Hino A, Fuse I, Echigo T, Oka H, Iwamoto Y, Fujimoto M. Cipping of upward profecting anterior communicating aneurysms via pterional craniotomy: Approach from the side of A2 of anterior displacement. No Shinkei Geka. 2006. 34: 149-58
8. Izumo T, Matsuo T, Hayashi K, Hiu T, Morofuji Y, Horie N. Surgical treatment for anterior communicating artery aneurysms. Surgery for Cerebral Stroke (Jpn). 2014. 42: 270-7
9. Madfugiri VS, Ambekar S, Pandey P, Guthikonda B, Bollam P, Brown B. The pteriornal and suprablow approaches for aneurysms surgery: A systematic review of intraoperative rupture rates in 9488 aneurysms. World Neurosurg. 2013. 80: 836-44
10. Martin GE, Junqué C, Juncadella M, Gabarrós A, de Miquel MA, Rubio F. Olfactory dysfunction after subarachnoid hemorrhage caused by ruptured aneurysms of the anterior communicating artery. Clinical article. J Neurosurg. 2009. 111: 958-62
11. Park J, Lee SH, Kang DH, Kim JS. Olfactory dysfunction after ipsilateral and contralateral pterional approaches for cerebral aneurysms. Neurosurgery. 2009. 65: 727-32
12. Sekhar LN, Natarajan SK, Britz GW, Ghodke B. Microsugical management of anterior communicating artery aneuryms. Neurosurgery. 2007. 61: 273-90
13. Suzuki J, Yoshimoto T, Mizoi K. Preservation of the olfactory tract in bifrontal craniotomy for anterior communicating artery aneurysms, and the functional prognosis. J Neurosurg. 1981. 54: 342-5
14. Tanaka T, Fuse I, Watanabe K. [Examination of approach side and surgical complication of A-com aneurysm clipping in pterional approach by same operator. Surgery for Cerebral Stroke (Jpn). 2012. 40: 183-7