- Department of Neurosurgery, University of Tokyo Hospital, Bunkyo-ku,
- Department of Neurosurgery, Toranomon Hospital, Minato-ku, Tokyo, Japan.
Correspondence Address:
Takayuki Hara
Department of Neurosurgery, Toranomon Hospital, Minato-ku, Tokyo, Japan.
DOI:10.25259/SNI_542_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sukwoo Hong, Takayuki Hara. Hybrid nerve sheath tumor in the orbit: A case report and review of literature. 20-Dec-2019;10:250
How to cite this URL: Sukwoo Hong, Takayuki Hara. Hybrid nerve sheath tumor in the orbit: A case report and review of literature. 20-Dec-2019;10:250. Available from: https://surgicalneurologyint.com/surgicalint-articles/9812/
Abstract
Background: In neurosurgical practice, we rarely encounter hybrid nerve sheath tumors (HNST) in the orbit. We recently had a patient of this rare tumor. We believe that this is the first report where we resected the tumor transcranially.
Case Description: A 54-year-old male presented with the left proptosis and intraconal tumor of 43 mm. We performed fronto-orbital craniotomy to resect the tumor mass. His proptosis completely improved and discharged home with a modified Rankin Scale of 1.
Conclusion: Transcranial resection of orbital HNST was a safe and effective way to treat. Since we do not have much data regarding this rare tumor, we need to accumulate more cases.
Keywords: Exophthalmos, Hybrid peripheral nerve sheath tumor, Pterional
INTRODUCTION
Few case reports have been made regarding the hybrid nerve sheath tumor (HNST) in the orbit. HNST was officially enrolled as a distinct tumor entity relatively recently[
CASE REPORT
History and examination
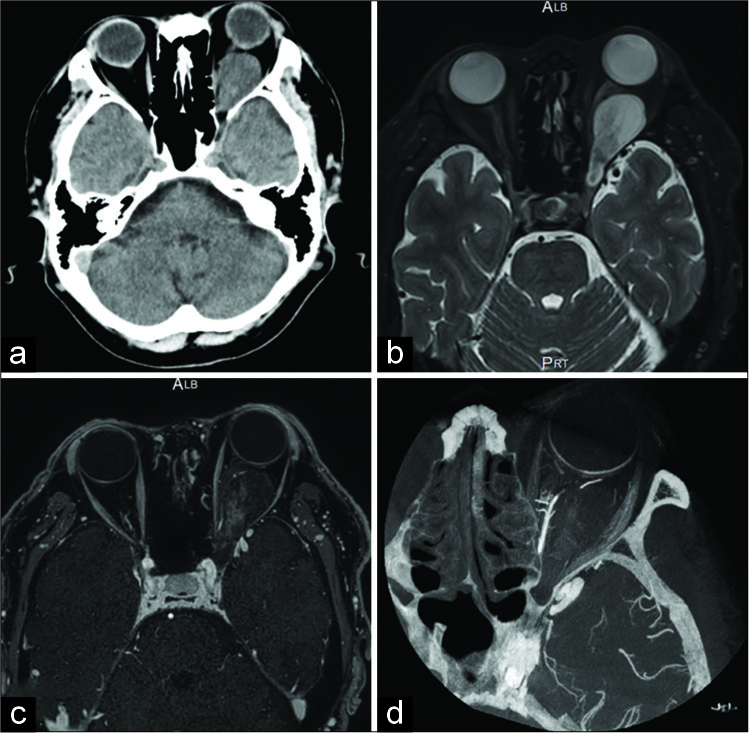
A 54-year-old male had the left proptosis pointed out on his regular health checkup. Subsequent computed tomography showed tumor in the left orbit. He was referred to our hospital for further evaluation. Physical examination was unremarkable except for the left proptosis with normal visual acuity (20/320 oculus dexter and 20/320 oculus sinister) and field. He had no diplopia, nystagmus, or stigmata of neurofibromatosis. Computed tomography showed an apparent proptosis of the left eye [
Figure 1:
Computed tomography showed the left intraconal orbital tumor compressing the globe with resultant exophthalmos (a). T2-weighted magnetic resonance imaging (MRI) showed a hyperintense tumor (b). Gadolinium-enhanced fat suppression T1-weighted MRI showed a heterogeneous enhancement (c). VasoCT showed some feeders from the ophthalmic artery (d).
Operation
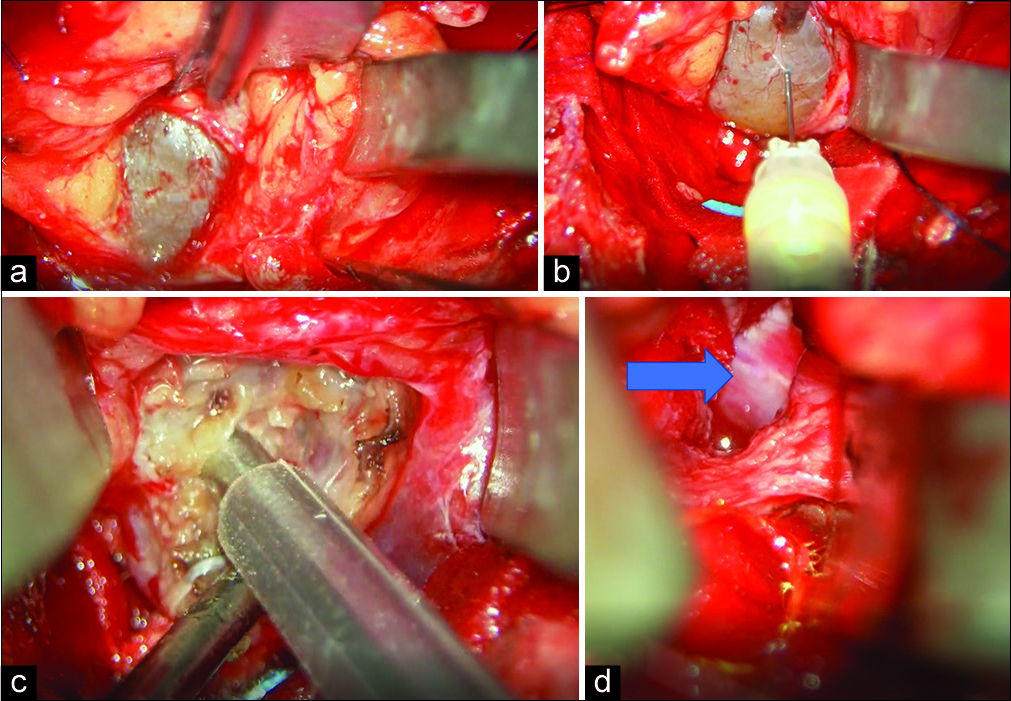
We administered general endotracheal anesthesia and placed lumbar drain. We positioned the patient supine with the head turned 20° to the right and fixed in Mayfield head holder. A curvilinear skin incision was made from just anterior to the tragus to the forehead behind the hairline. Skin flap and the temporalis muscle were reflected in two layers and frontotemporal craniotomy was done. Orbital bar was removed with bone saw lateral to the supraorbital foramen. The greater wing of the sphenoid was rongeured off until temporal dura was exposed. The lesser wing of the sphenoid was rongeured off toward sphenoid ridge until meningo-orbital band was exposed. The superior and lateral wall of the orbit was rongeured off to expose the periorbita. We incised the periorbita in between the superior and lateral rectus muscles and identified the tumor [
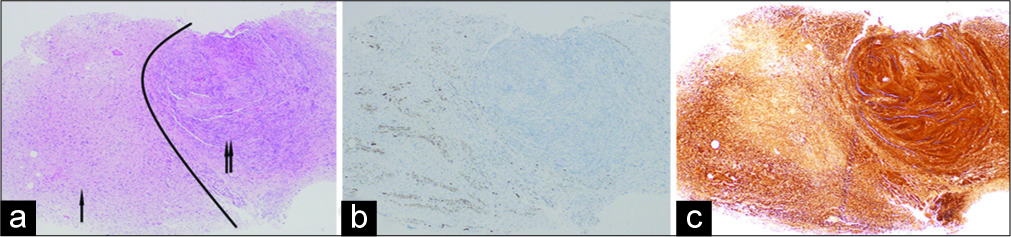
Histopathological findings
Histology showed loosely proliferating spindle tumor cells (neurofibromatosis [NF] component) and nuclear palisading tumor cells (schwannomatous component). No clear border between the two components was observed. On immunohistochemical analysis, S100 protein was slightly and strongly positive in NF and schwannomatous component, respectively. Neurofilament staining showed axonal filament in NF component [
Figure 3:
Hematoxylin and eosin stain showed neurofibromatosis (arrow) and schwannomatous components (double arrow). Arbitrary black line is drawn (a). Neurofilament stain showed positivity in the neurofibromatosis component (b). S100 stain showed strong positivity in the schwannomatous component (c). Original ×40.
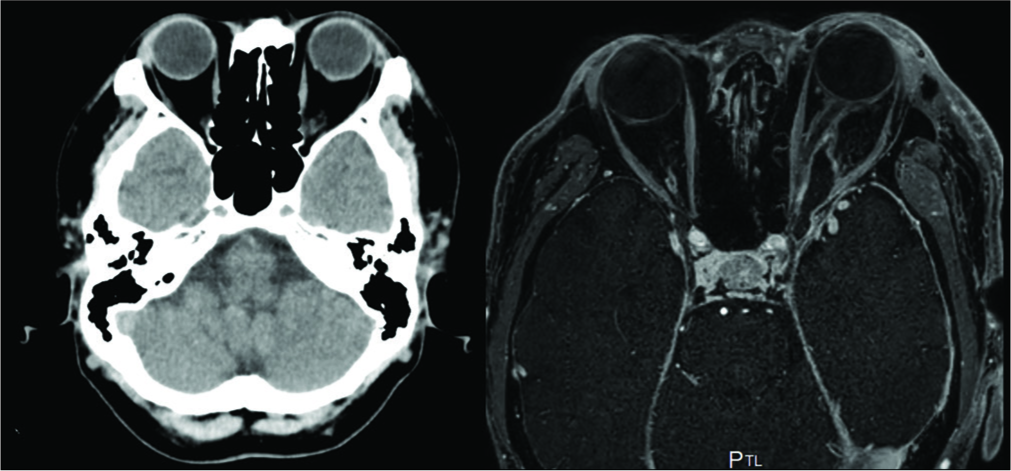
Postoperative course
His postoperative course was uneventful except for abducens nerve palsy and ptosis. The postoperative imaging study showed completely improved proptosis and substantially reduced tumor as well as decompression of the optic nerve [
DISCUSSION
To the best of our knowledge, this is the second report of intraconal orbital HNST. HNST was first described in 1998 and only recently included in the WHO classification in 2013. Due to its rarity, the exact incidence is not known. However, based on the available literature, it is diagnosed most commonly in young adults with no gender predilection.[
HNST from pathological standpoint
HNST is mainly a mixture of two or more out of the following: neurofibroma, perineurioma, and schwannoma.[
HNST from clinical standpoint
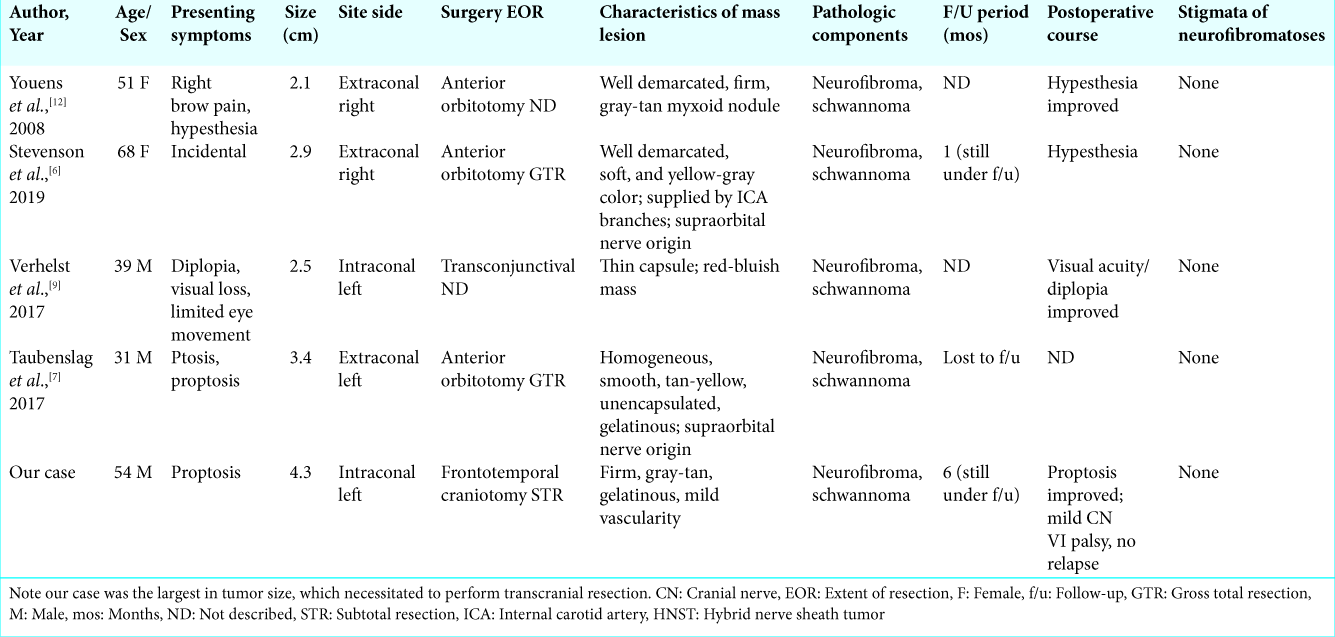
In this paper, we described the intraoperative detail of orbital HNST, which was resected transcranially. All of the previous orbital HNSTs were resected through anterior orbitotomy. However, in our case, the tumor size was the largest of the reported cases [
CONCLUSION
HNST should be included in the differential diagnosis of well-demarcated orbital tumor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Linos K, Stuart L, Goncharuk V, Edgar M. Benign cutaneous biphasic hybrid tumor of perineurioma and cellular neurothekeoma: A case report expanding the clinical and histopathologic features of a recently described entity. Am J Dermatopathol. 2015. 37: 319-22
2. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK.editorsWeltgesundheitsorganisation, International Agency for Research on C. WHO Classification of Tumours of the Central Nervous System. Geneva: World Health Organization; 2016. p.
3. Matter A, Hewer E, Kappeler A, Fleischmann A, Vajtai I. Plexiform hybrid granular cell tumor/perineurioma: A novel variant of benign peripheral nerve sheath tumor with divergent differentiation. Pathol Res Pract. 2012. 208: 310-4
4. Michal M, Kazakov DV, Michal M.editors. Hybrid peripheral nerve sheath tumors: A review. Cesk Patol Spri. 53: 81-8
5. Röhrich M, Koelsche C, Schrimpf D, Capper D, Sahm F, Kratz A. Methylation-based classification of benign and malignant peripheral nerve sheath tumors. Acta Neuropathol. 2016. 131: 877-87
6. Stevenson LJ, McElnea EM, McKelvie PA, Hardy TG. Hybrid neurofibroma/schwannoma of the orbit. Ophthalmic Plast Reconstr Surg. 2019. 35: e49-52
7. Taubenslag KJ, Nickols HH, Chelnis JG, Mawn LA. Hybrid neurofibroma/schwannoma of the supraorbital nerve: Clinicopathologic correlation of a rare tumor. Ophthalmic Plast Reconstr Surg. 2017. 33: S104-6
8. Ud Din N, Ahmad Z, Abdul-Ghafar J, Ahmed R. Hybrid peripheral nerve sheath tumors: Report of five cases and detailed review of literature. BMC Cancer. 2017. 17: 349-
9. Verhelst E, Lauwers N, Siozopoulou V, de Keizer RW, De Groot V. Intraconal hybrid neurofibroma schwannoma of the orbit. Acta Ophthalmol. 2017. 95: S259-
10. Wang L, Wang G, Gao T. Congenital melanocytic nevus with features of hybrid schwannoma/perineurioma. J Cutan Pathol. 2013. 40: 497-502
11. Yamada S, Kitada S, Nabeshima A, Noguchi H, Sasaguri Y, Hisaoka M. Benign cutaneous plexiform hybrid tumor of perineurioma and cellular neurothekeoma arising from the nose. Diagn Pathol. 2013. 8: 165-
12. Youens KE, Woodward J, Wallace D, Cummings TJ. Hybrid neurofibroma-schwannoma of the orbit. Orbit. 2008. 27: 223-5