- Department of Neurosurgery, Loghman e Hakim hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- Department of Neurosurgery, Emam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran
Correspondence Address:
Mehrdad H. Bakhtevari
Department of Neurosurgery, Loghman e Hakim hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
DOI:10.4103/sni.sni_162_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Keveh Ebrahimzadeh, Mehrdad H. Bakhtevari, Misagh Shafizad, Omidvar Rezaei. Hydrocephalus as a rare compilation of vertebrobasilar dolichoectasia: A case report and review of the literature. 24-Oct-2017;8:256
How to cite this URL: Keveh Ebrahimzadeh, Mehrdad H. Bakhtevari, Misagh Shafizad, Omidvar Rezaei. Hydrocephalus as a rare compilation of vertebrobasilar dolichoectasia: A case report and review of the literature. 24-Oct-2017;8:256. Available from: http://surgicalneurologyint.com/?post_type=surgicalint_articles&p=8655
Abstract
Background:Vertebrobasilar dolichoectasia (VBD) is a rare disease characterized by significant expansion, elongation, and tortuosity of the vertebrobasilar arteries. Hydrocephalus is a rare compilation of VBD.
Case Description:In this study, we report a 68-year-old male presenting with headache, progressive decreased visual acuity, memory loss, imbalance while walking, and episodes of urinary incontinency. The patient was diagnosed with dolichoectasia of basilar artery causing compression of the third ventricular outflow and thus, presenting with hydrocephalus documented with brain computed tomography scan and brain magnetic resonance imaging. The patient underwent surgical operation and ventriculoperitoneal shunt placement.
Conclusion:In the case of hydrocephalus or normal pressure hydrocephalous, VBD should be considered as a differential diagnosis.
Keywords: Dolichoectasia, hydrocephaly, vertebrobasilar, water hammer, Windkessel
INTRODUCTION
Dolichoectasia is defined as a rare disorder of vascular elongation, widening, and tortuosity, with highly variable neurological symptoms and signs. Its prevalence in the adult population is estimated at 0.06–5.8% and affects most frequently the basilar and vertebral arteries, followed by the internal carotid artery and the middle cerebral artery.[
The main criteria for diagnosis of vertebrobasilar dolichoectasia (VBD) are a basilar artery or vertebral artery diameter >4.5 mm, deviation of more than 10 mm from the shortest expected course, basilar length >29.5 mm, or intracranial vertebral artery length >23.5 mm in magnetic resonance angiography.[
VBD can develop without any clinical symptoms, and most cases are asymptomatic. Symptoms of VBD can be divided into ischemic, hemorrhagic, and mass effect, with ischemic stroke the most common symptom and also the most common cause of VBD-related death.[
The second most common symptom of VBD patients is brainstem and cranial nerve compression which can manifest as weakness, hypertension, cranial nerve palsy, and intracranial pseudospace-occupying lesions.[
CASE REPORT
A 68-year-old male presented with headache and progressive visual loss over 12 months. He also complained of memory loss, gait disturbance, and episodes of urinary incontinency for the past 4 months. The patient's past medical and psychological history were normal. In physical examination, there was a significant decrease in visual acuity of both eyes (able to detect finger count in <1 m distance). Neurological examination revealed bilateral optic atrophy as a sign of increased intracranial pressure (ICP) on fundoscopic ophthalmic examination.
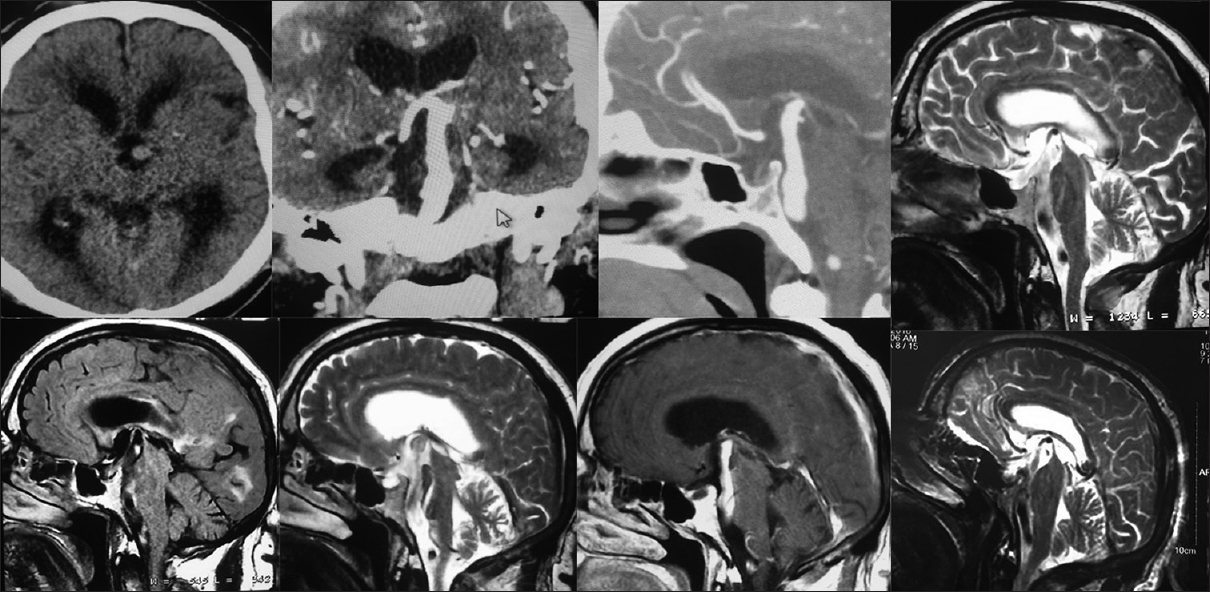
Due to his presentation, brain computed tomography (CT) scan was performed, which showed severe hydrocephalus with periventricular edema. Further evaluation with magnetic resonance imaging (MRI) of the brain demonstrated dilated lateral ventricles and dilated basilar artery, which was extending into the suprasellar cistern compressing floor of the third ventricle.
The patient was diagnosed with dolichoectasia of vertebrobasilar arteries which caused hydrocephalus [
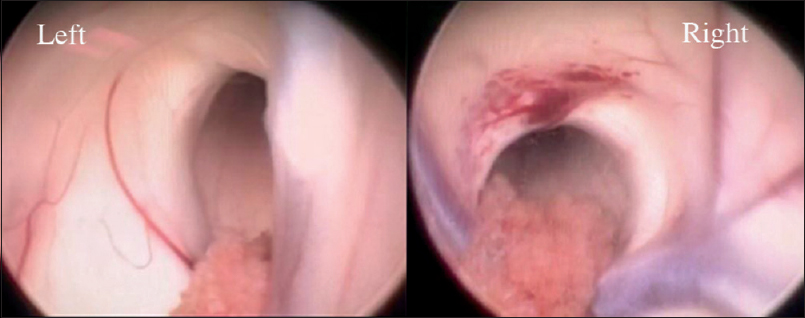
Because of the severe hydrocephalous, we recommended the patient for placement of a ventriculoperitoneal shunt. We avoided endoscopic third ventriculostomy because of the high risk of basilar artery injury. Endoscopic septostomy followed by unilateral ventriculoperitoneal shunting was performed and both Monro foramina and basilar pulsation were seen during endoscopic septostomy [
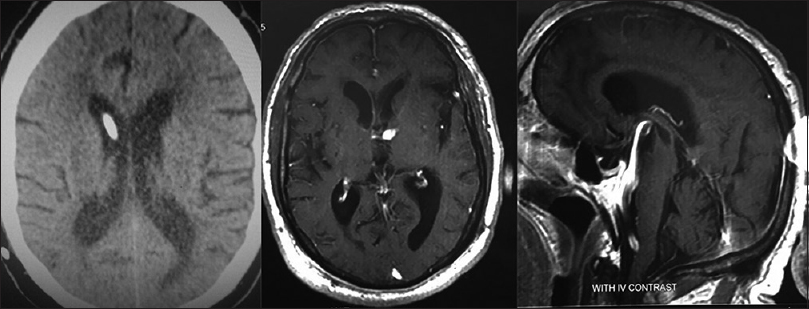
The postoperative period was uneventful, and the patient was discharged from hospital on the fifth postoperative day. Patient's headache resolved during postoperative period, gait imbalance, memory disturbance, and urinary incontinency improved gradually during 6 months. The visual acuity remained unchanged. Follow-up imaging after 6 months revealed relief of the hydrocephalus with normal-sized ventricles [
DISCUSSION
Mechanisms of hydrocephalus
It should be noted that hydrocephalus is a rare compilation of VBD. Estimated 5-year risk of progressive hydrocephalus is 3.3%.[
To confirm a possible water hammer effect causing the dilation of the ventricles, we should have confirmatory imaging such as ventriculogram or MRI Cine study demonstrating CSF flow through the aqueduct. In our case, the relatively rapid clinical course, the loss of visual acuity, and the marked ventriculomegally involving the lateral and third ventricles while sparing the fourth ventricle, all argue in favor of obstructive hydrocephalus produced by compression of the posterior third ventricle and/or aqueduct by the dolichoectatic basilar artery. The rapid resolution of the ventriculomegally with shunting would also be extremely unusual for NPH and supports the diagnosis of obstructive hydrocephalus.
Literature review
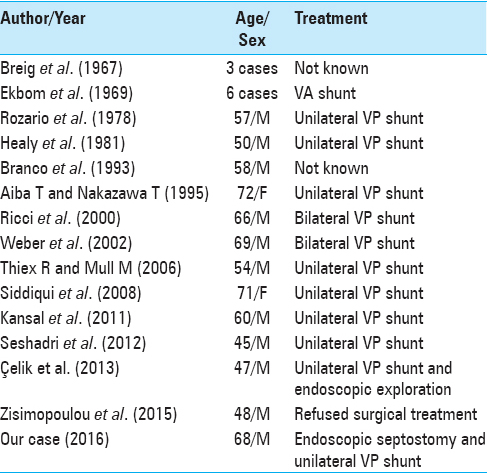
There are few studies which have reported hydrocephalus as a consequence of VBD. In a study of Ikeda et al., 7345 adult subjects were investigated. They found that 96 of them had asymptomatic VBD [
In 1998, Marinescu et al. reported a case in which an aneurysm of the basilar artery was revealed by an ischemic stroke in a 65-year-old man. Hydrocephalus developed during the following months. The MRI studies showed that it could not be explained merely by a permanent compression. However, the patient improved clearly after a ventriculoperitoneal derivation.
Aneurysms of the basilar artery can cause hydrocephalus due to compression of the third ventricle or the Sylvian aqueduct. The observation of a particular case led to discuss another possible mechanism of hydrocephalus. The hydrocephalus could be explained by a “water hammering” effect due to the pulsating blood in the ectatic vessel, which created a CSF outflow impairment through the third ventricle.[
Breig et al.[
In 2008, Siddiqui et al. described a case of a 71-year-old woman presenting with clinical features of raised ICP due to VBD producing obstructive hydrocephalus. The patient underwent emergency ventricular drainage, with resulting decompression of the ventricles and resolution of symptoms.[
In 2011, Kansal et al.[
In a prospective study, Passero et al. investigated 156 patients with VBD for an average follow-up period of 11.7 years. Hydrocephalus occurred in only two cases (1.3%) of VBD. On the contrary, ischemic stroke occurred in 59 cases (37.8%), cranial nerve and brainstem compression occurred in 31 cases (19.9%), and cerebral hemorrhage occurred in 21 cases (13.5%).[
In 2015, Zisimopoulou et al. reported a 48-year old male with a profound dilatation of the ventricular system due to a dolichoectatic basilar artery. They mentioned that the patient suffered from longstanding hydrocephalus and presenile dementia. They suggested that the dilated basilar artery initially caused nonobstructive or obstructive-invisible hydrocephalus under the water hammer effect by impairment of CSF flow. That resulted to the aforementioned symptoms of evolving cognitive impairment and personality changes. Secondarily, as the VBD evolved by direct compression of the third floor ventricle, hydrocephalus worsened.[
According to our literature review, among the reported cases, Ricci et al.[
VBD-induced hydrocephalus is a very rare condition, which is commonly managed with ventriculoperitoneal shunt [
CONCLUSION
In the case of hydrocephalus or NPH, VBD and other vascular malformations should be considered as a differential diagnosis. We proposed that as in the NPH, Windkessel effect could be one of the probable cause of hydrocephalous in vertebrobasilar dolichoectatic-induced hydrocephalous by interfering with normal CSF circulation and pulsation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on: www.surgicalneurologyint.com
References
1. Adams HP, Hachinski VC, Norris JW. Ischemic cerebrovascular disease: Oxford University Press. 2001. p.
2. Breig A, Ekbom K, Greitz T, Kugelberg E. Hydrocephalus due to elongated basilar artery. A new clinicoradiological syndrome. Lancet. 1967. 1: 874-75
3. El-Ghandour NM. Microvascular decompression in the treatment of trigeminal neuralgia caused by vertebrobasilar ectasia. Neurosurgery. 2010. 67: 330-7
4. Flemming KD, Wiebers DO, Brown RD, Link MJ, Huston J, McClelland RL. The natural history of radiographically defined vertebrobasilar nonsaccular intracranial aneurysms. Cerebrovasc Dis. 2005. 20: 270-9
5. Giang DW, Perlin SJ, Monajati A, Kido DJ, Hollander J. Vertebrobasilar dolichoectasia: Assessment using MR. Neuroradiology. 1988. 30: 518-23
6. Huang L, Yu C-Y, Wang B-N, Zhang H-M, Li L-Y, Wang Y. Vertebrobasilar dolichoectasia causing a presentation resembling basilar-type migraine. Clin Neurol Neurosurg. 2013. 115: 784-6
7. Ikeda K, Nakamura Y, Hirayama T, Sekine T, Nagata R, Kano O. Cardiovascular risk and neuroradiological profiles in asymptomatic vertebrobasilar dolichoectasia. Cerebrovasc Dis. 2010. 30: 23-8
8. Kansal R, Mahore A, Dange N, Kukreja S. Dolichoectasia of vertebrobasilar arteries as a cause of hydrocephalus. J Neurosci Rural Pract. 2011. 2: 62-4
9. Lou M, Caplan LR. Vertebrobasilar dilatative arteriopathy (dolichoectasia). Ann N Y Acad Sci. 2010. 1184: 121-33
10. Marinescu M, Remy A, Dufour H, Derome P, Cambon H. [A peculiar mechanism of hydrocephalus: The “water-hammering” effect]. Neurochirurgie. 1998. 44: 117-20
11. Moreira I, Mendonça T, Monteiro JP, Santos E. Hypnic headache and basilar artery dolichoectasia. The Neurologist. 2015. 20: 106-7
12. Nishizaki T, Tamaki N, Takeda N, Shirakuni T, Kondoh T, Matsumoto S. Dolichoectatic basilar artery: A review of 23 cases. Stroke. 1986. 17: 1277-81
13. Passero S, Rossi S, Giannini F, Nuti D. Brain-stem compression in vertebrobasilar dolichoectasia. A multimodal electrophysiological study. Clin Neurophysiol. 2001. 112: 1531-9
14. Passero SG, Rossi S. Natural history of vertebrobasilar dolichoectasia. Neurology. 2008. 70: 66-72
15. Pereira-Filho A, Faria M, Bleil C, Kraemer JL. Brainstem compression syndrome caused by vertebrobasilar dolichoectasia: Microvascular repositioning technique. Arq Neuropsiquiatr. 2008. 66: 408-11
16. Ricci G, Lenzi J, Esposito V. Hydrocephalus caused by dolichoectatic basilar artery. Case report. J Neurosurg Sci. 2000. 44: 155-8
17. Siddiqui A, Chew NS, Miszkiel K. Vertebrobasilar dolichoectasia: A rare cause of obstructive hydrocephalus: Case report. Br J Radiol. 2008. 81: 27603660-
18. Smoker WR, Corbett JJ, Gentry LR, Keyes WD, Price MJ, McKusker S. High-resolution computed tomography of the basilar artery: 2. Vertebrobasilar dolichoectasia: Clinical-pathologic correlation and review. AJNR Am J Neuroradiol. 1986. 7: 61-72
19. Thiex R, Mull M. Basilar megadolicho trunk causing obstructive hydrocephalus at the foramina of Monro. Surg Neurol. 2006. 65: 199-201
20. Ubogu EE, Zaidat OO. Vertebrobasilar dolichoectasia diagnosed by magnetic resonance angiography and risk of stroke and death: A cohort study. J Neurol Neurosurg Psychiatry. 2004. 75: 22-6
21. Weber MA, Steiner T, Fiebach J. [Unusual cause of acute impairment of consciousness. Decompensated hydrocephalus caused by blockage of the foramen Monro due to enlarged basilar artery]. Radiologe. 2002. 42: 833-6
22. Wolters FJ, Rinkel GJ, Vergouwen MD. Clinical course and treatment of vertebrobasilar dolichoectasia: A systematic review of the literature. Neurol Res. 2013. 35: 131-7
23. Yang XS, Li ST, Zhong J, Zhu J, Du Q, Zhou QM. Microvascular decompression on patients with trigeminal neuralgia caused by ectatic vertebrobasilar artery complex: Technique notes. Acta Neurochir. 2012. 154: 793-7
24. Yuan YJ, Xu K, Luo Q, Yu JL. Research progress on vertebrobasilar dolichoectasia. Int J Med Sci. 2014. 11: 1039-48
25. Yuh SJ, Alkherayf F, Lesiuk H. Dolichoectasia of the vertebral basilar and internal carotid arteries: A case report and literature review. Surg Neurol Int. 2013. 4: 153-
26. Zisimopoulou V, Ntouniadaki A, Aggelidakis P, Siatouni A, Gatzonis S, Tavernarakis A. Vertebrobasilar dolichoectasia induced hydrocephalus: The water-hammer effect. Clin Pract. 2015. 5: 749-