- Department of Neurosurgery, 7Tir hospital, Iran University of Medical Sciences, Tehran, Iran.
DOI:10.25259/SNI_226_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Arash Fattahi, Seyed Mohammad Reza Mohajeri, Abdolhadi Daneshi, Ardeshir Shahivand. Hyperextension thoracic spine fracture with complete neurological recovery after surgical fixation: A case report. 30-May-2020;11:137
How to cite this URL: Arash Fattahi, Seyed Mohammad Reza Mohajeri, Abdolhadi Daneshi, Ardeshir Shahivand. Hyperextension thoracic spine fracture with complete neurological recovery after surgical fixation: A case report. 30-May-2020;11:137. Available from: https://surgicalneurologyint.com/surgicalint-articles/10065/
Abstract
Background: Hyperextension thoracic spine fractures (HTSFs) typically involve the anterior ligamentous complex of the spine. These patients often present with paraplegia and warrant early surgical reduction/fixation even though few deficits resolve. Here, we present the unusual case of a 40-year-old male whose paraparetic deficit resolved following reduction/fixation of a T7-T8 HTSF.
Case Description: A 40-year-old male presented with a thoracic computed tomography (CT) documented T7- T8 HTSF following a motor vehicle accident. His neurological examination revealed severe paraparesis, but without a sensory level (ASIA motor score 78). The chest CT angiogram scan revealed a hypodensity in the aorta, representing a small traumatic aortic dissection responsible for the patient’s right hemothorax; 450 ml of blood was removed on chest tube placement. He underwent urgent/emergent thoracic spine reduction and fixation at the T7-T8 level. Within 5 postoperative months, he recovered fully neurological function (ASIA motor score 100).
Conclusion: We recommend urgent/emergent surgical reduction/stabilization for patients with thoracic HTSF to decrease offer the potential for neurological recovery and avoid secondary injury due to continued compression.
Keywords: Aortic dissection, Hyperextension thoracic spine fractures, Spinal cord injury, Traction, Trauma
BACKGROUND
Hyperextension thoracic spine fractures (HTSFs) typically involve the anterior spinal ligamentous complex (i.e., AO classification type B3).[
CASE PRESENTATION
A 40-year-old male sustained a motor vehicle accident. The preliminary neurological examination revealed lower extremity paraparesis with sensory preservation and urinary retention; ASIA motor score 78. The chest computed tomography (CT) angiogram revealed a hypodensity in the aorta, representing a small traumatic aortic dissection responsible for the patient’s right hemothorax; 450 ml of blood was removed on chest tube placement. When the thoracic CT also demonstrated a T7-T8 HTSF, he underwent an emergent thoracic spine reduction/fixation procedure. Surgery at the T7 level warranted bilateral laminectomies and resection of the pars interarticularis; pedicle screws were placed bilaterally from T5 to T10, and following displacement/repositioning under direct fluoroscopic guidance, a posterior arthrodesis was performed [
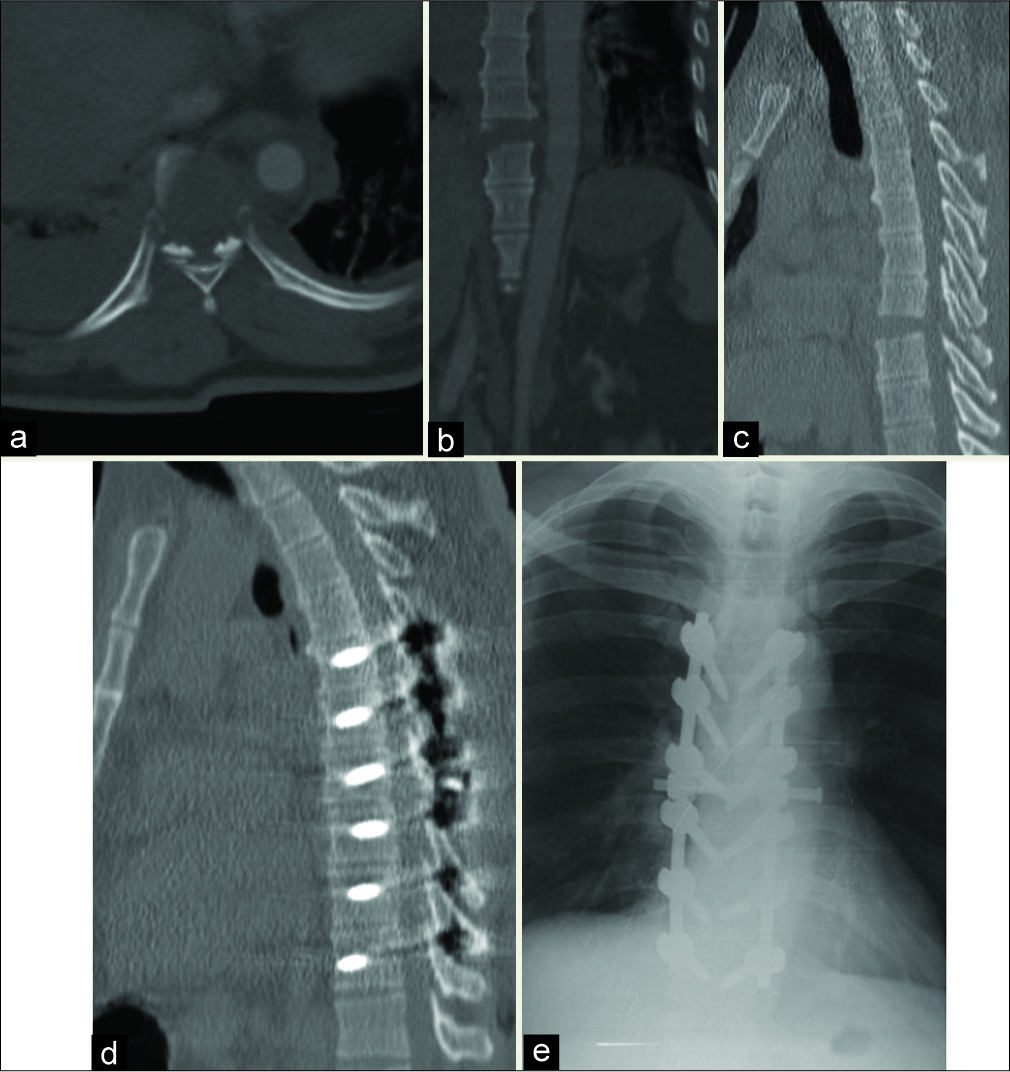
Figure 1:
The computed tomography (CT) scan of the thoracic spine with contrast for detect of vascular injury showed the bilateral head of seventh ribs fracture and right huge hemothorax on an axial view (a). Furthermore, we could see a widening of T7-8 disc space on coronal reconstruction (b) with a small avulsion of the superior endplate of T8. Furthermore, a small hypodensity in the adjacent aorta could be seen that was treated with traumatic aortic dissection diagnosis (b). Sagittal view reconstruction (c) revealed a fracture of the T7 spinous process. Postoperative CT scan in sagittal view (d) and anteroposterior view X-ray (e) showed normal alignment of the previously displaced thoracic spine.
DISCUSSION
HTSFs are rare.[
Spontaneous versus surgical reduction of HTSF
In some cases, external bracing alone may be utilized where there is a spontaneous reduction of the HTSF. Choy et al. utilized complete bed rest for 16 weeks in a patient who demonstrated spontaneous fixation (e.g., the 16-week CT scan confirmed adequate anterior osteophyte bridging).[
Goal of HTSF treatment
One of the surgical goals in treating patients with HTSF is the decompression of neural tissues (i.e., as in our patient undergoing bilateral limited T7 laminectomy with resection of the pars interarticularis) and the provision of simultaneous reduction/stabilization (i.e., to prevent further spinal cord injury). Elgafy et al. and Shin et al., respectively, performed spinal decompressions in their patients utilizing laminectomies with spinous process resections.[
Early reduction/fixation warranted
Patients with HTSF and anterior disk space widening warrant early surgical reduction/fixation to provide immediate stability and to potentiate neurological recovery while avoiding secondary compressive injury. The number of vertebral levels requiring fusion ranges from 2 to 13.[
Residual deficits after surgery for HTSF
Rare patients with significant preoperative neurological deficits attributed to HTSF improve with surgery, while the majority do not.[
Etiology and evidence of aortic dissection with HTSF
Aortic dissection can be attributed to acute widening of the distance between the HTSF endplates (i.e., seen on CT), resulting in a tethering/a stretch injury to the aorta over the posterior vertebral bodies. In our patient, a hypodensity seen in the aorta 3 cm below the fracture was diagnosed as a small traumatic aortic dissection responsible for the patient’s 450 cc hemothorax. In other patients, additional findings may include esophageal and tracheal injuries.
CONCLUSION
In this case, an initially paraparetic patient with sensory preservation attributed to a T7-T8 HTSF urgently (i.e., postadmission day 1) underwent bilateral laminectomies at T7 with bilateral T5-T10 pedicle screw fixation. Within 5 postoperative months, the patient was neurologically intact.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bailey J, Vanderheiden T, Burlew CC, Pinski-Sibbel S, Jordan J, Moore EE. Thoracic hyperextension injury with complete “bony disruption” of the thoracic cage: Case report of a potentially life-threatening injury. World J Emerg Surg. 2012. 7: 14-
2. Burke DC. Hyperextension injuries of the spine. J Bone Joint Surg. 1971. 53: 3-12
3. Choy W, Smith ZA, Viljoen SV, Lindley TE, Dahdaleh NS. Successful treatment of a three-column thoracic extension injury with recumbency. Cureus. 2016. 8: e614-
4. Denis FR, Burkus JK. Shear fracture-dislocations of the thoracic and lumbar spine associated with forceful hyperextension (lumberjack paraplegia). Spine (Phila Pa 1976). 1992. 17: 156-61
5. Elgafy H, Bellabarba C. Three-column ligamentous extension injury of the thoracic spine: A case report and review of the literature. Spine (Phila Pa 1976). 2007. 32: E785-8
6. Shin DE, Nam KS, Yoon HK, Lee JK, Cha YS. A rare hyperextension injury in thoracic spine presenting with delayed paraplegia. Asian Spine J. 2013. 7: 126-