- Department of Research, Texas Nerve and Paralysis Institute, Houston, Texas, United States.
Correspondence Address:
Rahul Kumar Nath, Department of Research, Texas Nerve and Paralysis Institute, Houston, Texas, United States.
DOI:10.25259/SNI_146_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rahul Kumar Nath, Chandra Somasundaram. Iatrogenic nerve injury and foot drop: Surgical results in 28 patients. 23-Jun-2022;13:274
How to cite this URL: Rahul Kumar Nath, Chandra Somasundaram. Iatrogenic nerve injury and foot drop: Surgical results in 28 patients. 23-Jun-2022;13:274. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11681
Abstract
Background: Most peroneal nerve injuries resulting in foot drop are secondary to trauma or iatrogenic. Foot drop can occur due to potential complications from the hip, lumbosacral spine, and knee surgeries, which are critical to diagnose and manage.
Methods: We reviewed our foot drop patients’ data to determine the incidence and iatrogenic causes of the injury and managed surgically by neurolysis of the peroneal nerve and transfer of functional fascicles of either the superficial peroneal or the tibial nerve to the deep peroneal nerve.
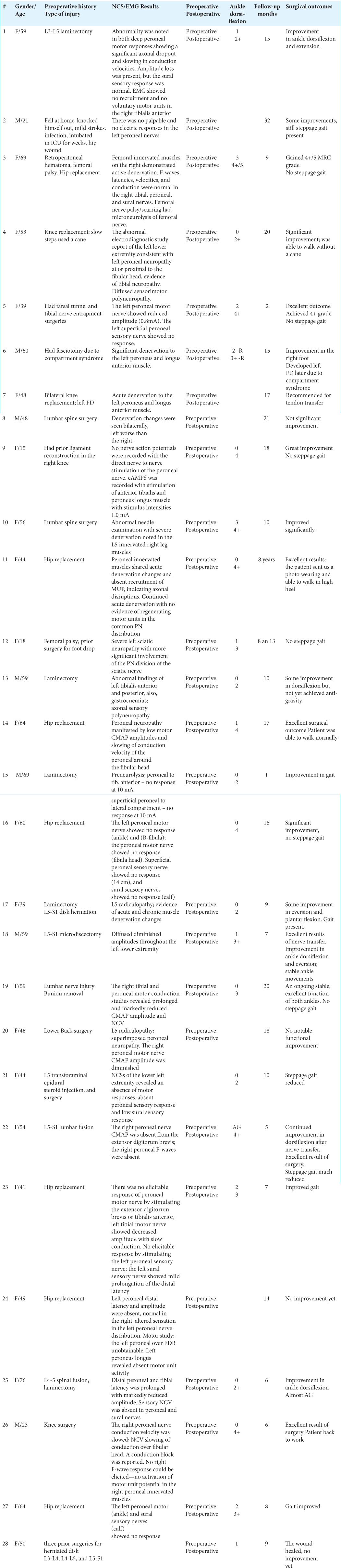
Results: We found 28 iatrogenic foot drop patients who have had surgery and postoperative follow-up evaluations with us. Before the onset of foot drop, all except one (27 of 28) patient have had surgeries in other clinics before presenting to our institution. Foot drop in one patient was due to infection and hip wound after he was intubated and stayed in ICU for 4 weeks. Thirteen of the 28 patients have had lumbosacral (L3-4, L4-L5, and L5-S1) fusion or laminectomy, eight have had hip surgery, and five have had knee surgery. One patient had a fasciotomy due to compartment syndrome and another patient had two previous surgeries for posterior tibial entrapment and tarsal tunnel syndrome at other institutions. NCS and EMG reports showed that these patients had injuries to the peroneal or tibial nerve after their prior surgeries. One patient had a femoral nerve injury. Preoperatively, 10 patients had severe foot drop with muscle weakness and a functional grade of 0/5; 16 patients had grades ranging from 1 to 2/5; and two patients had 3/5. Overall, 23 of the 28 patients (83%) had improvement in their ankle dorsiflexion with anti-gravity and regained a healthier gait after the decompression, neurolysis, and nerve transfer at our clinic.
Conclusion: Twenty-three of the 28 (83%) iatrogenic foot drop patients in this report regained a healthier gait with improved ankle dorsiflexion and anti-gravity after the neurolysis, and nerve transfer of the peroneal or tibial nerve and transfer of functional fascicles of either the superficial peroneal or the tibial nerve to the deep peroneal nerve at our clinic.
Keywords: Decompression, Foot drop, Hip surgery, Iatrogenic nerve injury, Lower back spine surgery, Nerve transfer
INTRODUCTION
Most peroneal nerve injuries resulting in foot drop are secondary to trauma or iatrogenic.[
Neurological deficit in the postsurgical period is under-recognized. Electrophysiological studies help diagnose the type and level of nerve injury.
Our study focuses on the surgical outcomes of iatrogenic foot drop resulting from potential complications of previous surgeries (lower back spine, hip, and knee surgeries) in other institutions before presenting to our clinic.
MATERIALS AND METHODS
We have reviewed our foot drop patients’ data who consulted us over 17 years (07–2004 to current) to determine the iatrogenic causes and incidence of foot drop. EMG and NCS results were used for diagnosing nerve injuries in addition to clinical examinations of the involved foot. We successfully managed foot drop by neurolysis of the peroneal nerve and the nerve transfer[
Surgical procedure
The involved leg was prepared and draped in a sterile fashion. A vertical midline incision was created in the distal posterior thigh, extended laterally along the posterior knee crease at the popliteal fossa, and then curved inferiorly along the course of the peroneal nerve over the fibular neck. The sciatic nerve was identified in the upper incision, which extended 6–8 cm above the popliteal fossa, and the terminal bifurcation of the nerve was traced. The superficial and deep peroneal nerve components were stimulated to identify or confirm conduction through the lateral and anterior muscle compartments. In those patients where the superficial peroneal nerve showed reasonable function, it was selected as the donor for the deep peroneal nerve. A partial transfer of one-third to the motor branch of the peroneal was feasible without clinical loss of eversion, as the superficial peroneal nerve is physically larger than the motor branch to the anterior tibialis muscle by about 3 times.
The motor branch to the anterior tibialis muscle was dissected several centimeters proximally within the common peroneal nerve so that coaptation was easily done without tension. If the lesion affected both superficial and deep branches, the tibial nerve was selected as a donor to the deep peroneal component of the common peroneal nerve or the deep peroneal nerve directly, if possible, by anatomy or by intraneural dissection. The incision created at the posterior knee and thigh allowed visualization of the sciatic bifurcation and dissection of the peroneal component to a distal level as possible to reduce regeneration time. The proximal tibial nerve was gently dissected intraneural to separate component fascicle groups. Typically, two large fascicle groups were then dissected out as suitable in diameter to fill the volume of the anterior and lateral part of the common peroneal nerve constituting the eventual deep peroneal motor branch. If intraneural dissection within the common peroneal nerve to isolate the deep peroneal nerve was feasible, then the tibial fascicle groups were coapted directly to the deep peroneal nerve fibers. Dissection was performed as distally as possible to reduce the length of regeneration to the anterior tibialis muscle. The deep peroneal nerve was sectioned with microsurgical technique and transposed to the area of the tibial nerve. The selected tibial nerve fascicles were then transected and placed in opposition to the peroneal nerve 2–4 cm distal to the bifurcation of the sciatic nerve and proximal to the popliteal crease area.
Approximately 25–30% of the overall volume of the tibial nerve was transferred. Neither the severed distal fascicles of the donor’s nerve nor the transected proximal fibers of the recipient’s deep peroneal nerve were managed specifically after being cut. The transfer site was secured with 9–0 nylon epineural stitches placed in a circumferential fashion around the peroneal-tibial or superficial peroneal-deep peroneal interface. The leg was then placed into a full range of motion to ascertain no tension at the repair site even with the knee was fully extended.
RESULTS
Before the onset of foot drop, all except one (27 of 28) patient have had surgeries in other clinics before presenting to our institution. Foot drop in one patient was due to infection and hip wound after he was intubated and stayed in ICU for weeks. Thirteen of the 28 patients have had lumbosacral (L3-4, L4-L5, and L5-S1) fusion or laminectomy, eight have had hip surgery, and five have had knee surgery. One patient had a fasciotomy due to compartment syndrome, and another patient had two previous surgeries for posterior tibial entrapment and tarsal tunnel syndrome at other institutions. NCS/EMG results showed that all except one patient had reduced peroneal nerve conduction velocity and amplitudes, and an absence or low sensory response of sural nerves. One patient had a femoral nerve injury and scarring and two patients also had tibial nerve injury.
Preoperatively, 10 patients had severe foot drop with muscle weakness and a functional grade of 0/5; 16 patients had grades ranging from 1 to 2/5; and two patients had 3/5 [
Video 1A
Video 1B
Video 2A
Video 2B
Video 2C
DISCUSSION
Iatrogenic nerve injuries can occur during any surgical procedure. Kretschmer et al.[
In addition to peroneal nerve injury, sciatic nerve injuries[
Complete familiarity with the region’s anatomy can significantly reduce the risk of nerve damage.[
CONCLUSION
Twenty-three of the 28 (83%) iatrogenic foot drop patients in this report gained a healthier gait with improved ankle dorsiflexion and anti-gravity after neurolysis of the peroneal nerve and transfer of functional fascicles of either the superficial peroneal or the tibial nerve to the deep peroneal nerve at our clinic.
Videos available on:
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank the patients and their families who participated in this study.
References
1. Antoniadis G, Kretschmer T, Pedro MT, König RW, Heinen CP, Richter HP. Iatrogenic nerve injuries: Prevalence, diagnosis, and treatment. Dtsch Arztebl Int. 2014. 111: 273-9
2. Bakhsh A. Long-term outcome of lumbar disc surgery: An experience from Pakistan. J Neurosurg Spine. 2010. 12: 666-70
3. Bohrer JC, Walters MD, Park A, Polston D, Barber MD. Pelvic nerve injury following gynaecologic surgery: A prospective cohort study. Am J Obstet Gynecol. 2009. 531: e1-7
4. Carolus A, Mesbah D, Brenke C. Focusing on foot drop: Results from a patient survey and clinical examination. Foot (Edinb). 2021. 46: 101693
5. Dellon AL. Postarthroplasty “palsy” and systemic neuropathy: A peripheral-nerve management algorithm. Ann Plast Surg. 2005. 55: 638-42
6. El Mansy Y, Migliorini F, Tingart M, Madarassy G. Minimally versus conventional-invasive transforaminal lumbar interbody fusion in patients with failed back surgery syndrome. Musculoskelet Surg. 2021. 105: 297-302
7. El-Taher M, Sallam A, Saleh M, Metwally A. Foot reanimation using double nerve transfer to deep peroneal nerve: A novel technique for treatment of neurologic foot drop. Foot Ankle Int. 2021. 42: 1011-21
8. Ghobrial GM, Williams KA, Arnold P, Fehlings M, Harrop JS. Iatrogenic neurologic deficit after lumbar spine surgery: A review. Clin Neurol Neurosurg. 2015. 139: 76-80
9. Hans SS, Shepard AD, Reddy P, Rama K, Romano W. Iatrogenic arterial injuries of spine and orthopedic operations. J Vasc Surg. 2011. 53: 407-13
10. Issack PS, Helfet DL. Sciatic nerve injury associated with acetabular fractures. HSS J. 2009. 5: 12-8
11. Kim DH, Murovic JA, Tiel R, Kline DG. Management and outcomes in 353 surgically treated sciatic nerve lesions. J Neurosurg. 2004. 101: 8-17
12. Kretschmer T, Antoniadis G, Braun V, Rath SA, Richter HP. Evaluation of iatrogenic lesions in 722 surgically treated cases of peripheral nerve trauma. J Neurosurg. 2001. 94: 905-12
13. Mont MA, Dellon AL, Chen F, Hungerford MW, Krackow KA, Hungerford DS. The operative treatment of peroneal nerve palsy. J Bone Joint Surg Am. 1996. 78: 863-9
14. Nath RK, Lyons AB, Paizi M. Successful management of foot drop by nerve transfers to the deep peroneal nerve. J Reconstr Microsurg. 2008. 24: 419-27
15. Prasad AR, Steck J, Dellon AL. Zone of traction injury to the common peroneal nerve. Ann Plast Surg. 2007. 59: 302-6
16. Pritchett JW. Lumbar decompression to treat foot drop after hip arthroplasty. Clin Orthop Relat Res. 1994. 303: 173-7
17. Speelziek SJ, Staff NP, Johnson RL, Sierra RJ, Laughlin RS. Clinical spectrum of neuropathy after primary total knee arthroplasty: A series of 54 cases. Muscle Nerve. 2019. 59: 679-82
18. Szwedowski D, Ambroży J, Grabowski R, Dallo I, Mobasheri A. Diagnosis, and treatment of the most common neuropathies following knee injuries and reconstructive surgery a narrative review. Heliyon. 2021. 7: e08032
19. Vecchio M, Santamato A, Geneovese F, Malaguarnera G, Catania VE, Latteri S. Iatrogenic nerve lesion following laparoscopic surgery. A case report. Ann Med Surg (Lond). 2018. 28: 34-7
20. Wiesseman GJ. Tendon transfers for peripheral nerve injuries of the lower extremity. Orthop Clin North Am. 1981. 12: 459-67
21. Yamauchi T, Kim K, Isu T, Iwamoto N, Yamazaki K, Matsumoto J. Undiagnosed peripheral nerve disease in patients with failed lumbar disc surgery. Asian Spine J. 2018. 12: 720-5
22. Zywiel MG, Mont MA, McGrath MS, Ulrich SD, Bonutti PM, Bhave A. Peroneal nerve dysfunction after total knee arthroplasty: characterization and treatment. J Arthroplasty. 2011. 26: 379-85