- Section of Neurosurgery, Carilion Clinic, Roanoke, Virginia, United States.
- Diagnostic Radiology, Department of Radiology, Carilion Clinic, Roanoke, Virginia, United States.
- Neurointerventional Surgery, Department of Radiology, Carilion Clinic, Roanoke, Virginia, United States.
Correspondence Address:
Joshua A. Cuoco
Section of Neurosurgery, Carilion Clinic, Roanoke, Virginia, United States.
DOI:10.25259/SNI_408_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Joshua A. Cuoco1, Michael J. Benko1, Brendan J. Klein1, David C. Keyes2, Biraj M. Patel3, Mark R. Witcher1. Idiopathic fourth ventricular outlet obstruction misdiagnosed as normal pressure hydrocephalus: A cautionary case. 25-Sep-2020;11:305
How to cite this URL: Joshua A. Cuoco1, Michael J. Benko1, Brendan J. Klein1, David C. Keyes2, Biraj M. Patel3, Mark R. Witcher1. Idiopathic fourth ventricular outlet obstruction misdiagnosed as normal pressure hydrocephalus: A cautionary case. 25-Sep-2020;11:305. Available from: https://surgicalneurologyint.com/surgicalint-articles/10288/
Abstract
Background: Fourth ventricular outlet obstruction is an infrequent but well-established cause of tetraventricular hydrocephalus characterized by marked dilatation of the ventricular system with ballooning of the foramina of Monro, Magendie, and Luschka. Multiple processes including inflammation, infection, hemorrhage, neoplasms, or congenital malformations are known to cause this pathological obstruction. However, true idiopathic fourth ventricular outlet obstruction is a rare phenomenon with only a limited number of cases reported in the literature.
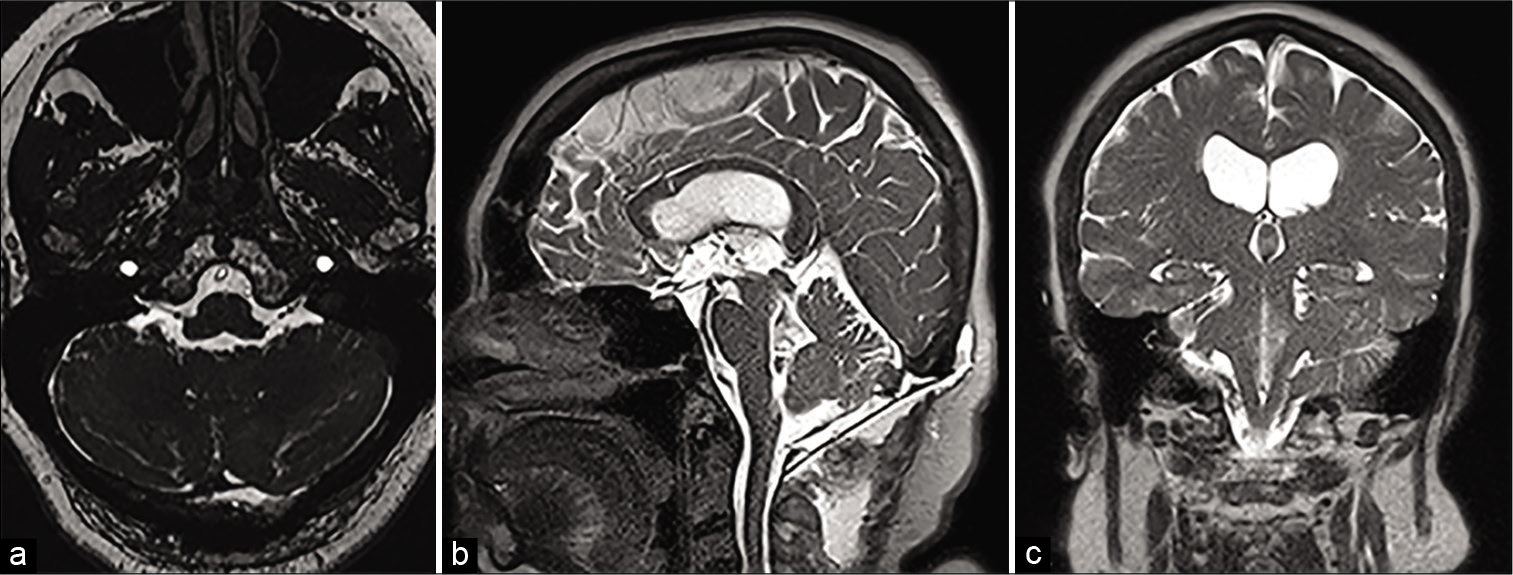
Case Description: A 61-year-old female presented with several months of unsteady gait, intermittent headaches, confusion, and episodes of urinary incontinence. Conventional magnetic resonance imaging demonstrated tetraventricular hydrocephalus without transependymal flow, but with ventral displacement of the brainstem and dorsal displacement of the cerebellum without an obvious obstructive lesion on pre- or post-contrast imaging prompting a diagnosis of normal pressure hydrocephalus. However, constructive interference in steady state (CISS) and half-Fourier acquisition single-shot turbo spin echo (HASTE) sequences followed by fluoroscopic dynamic cisternography suggested encystment of the fourth ventricle with thin margins of arachnoid membrane extending through the foramina of Luschka bilaterally into the pontocerebellar cistern. Operative intervention was pursued with resection of an identified arachnoid web. Postoperative imaging demonstrated marked reduction in the size of ventricular system, especially of the fourth ventricle. The patient’s symptomatology resolved a few days after the procedure.
Conclusion: Here, we describe an idiopathic case initially misdiagnosed as normal pressure hydrocephalus. The present case emphasizes the necessity of CISS sequences and fluoroscopic dynamic cisternography for suspected cases of fourth ventricular outlet obstruction as these diagnostic tests may guide surgical management and lead to superior patient outcomes.
Keywords: Arachnoid web, Endoscopic third ventriculostomy, Fourth ventricular outlet obstruction, Noncommunicating hydrocephalus, Obstructive hydrocephalus, Suboccipital craniectomy
INTRODUCTION
Fourth ventricular outlet obstruction is an infrequent but well-established cause of tetraventricular hydrocephalus characterized by marked dilatation of the ventricular system with ballooning of the foramina of Monro, Magendie, and Luschka. However, the majority of cases result from prior parenchymal insults, including inflammatory, infectious, hemorrhagic, neoplastic, or congenital etiologies.[
CASE REPORT
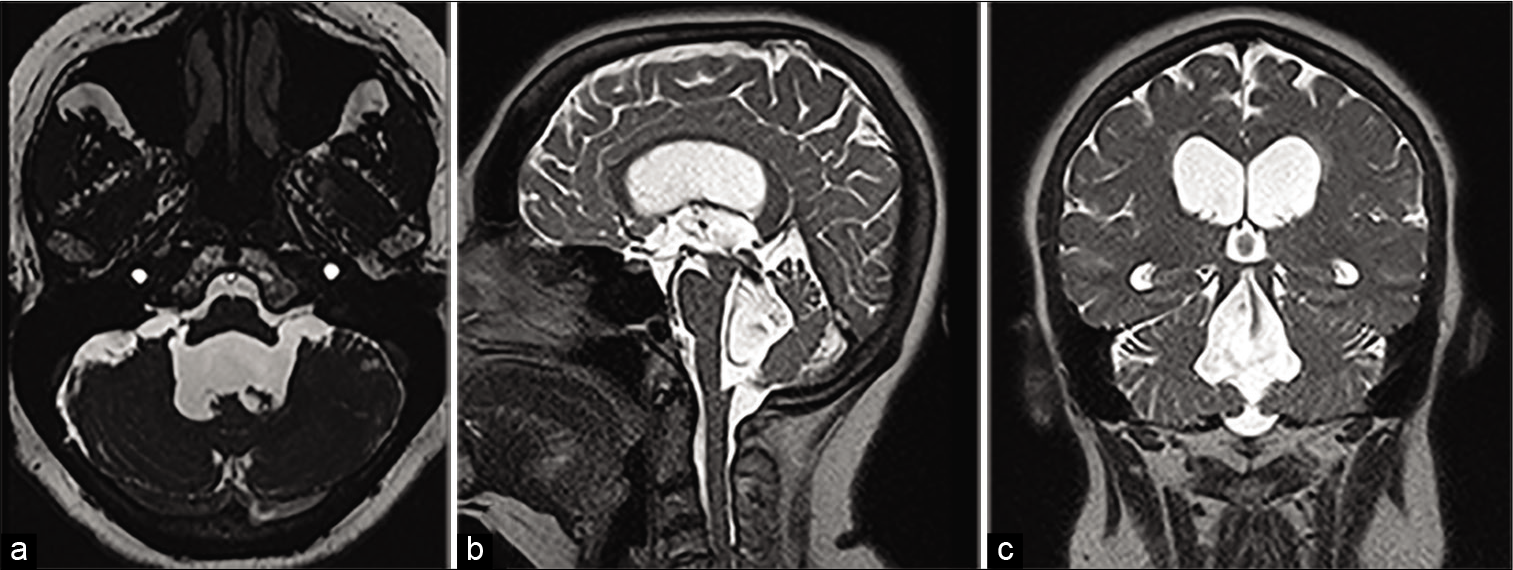
A 61-year-old female presented with several months of unsteady gait, intermittent headaches, confusion, and episodes of urinary incontinence. Her past medical history was unremarkable. Physical examination was notable for impaired tandem gait without focal deficits. Conventional magnetic resonance imaging (MRI) demonstrated tetraventricular hydrocephalus without transependymal flow, but with ventral displacement of the brainstem and dorsal displacement of the cerebellum without an obvious obstructive lesion on pre- or post-contrast imaging. Previous outpatient neurology workup concluded a diagnosis of normal pressure hydrocephalus based on her clinical symptomatology and radiographic findings, which prompted neurosurgical consultation. However, given the degree of fourth ventricular dilatation and subtle displacement of the brainstem and cerebellum, additional imaging sequences were ordered to rule out fourth ventricular outlet obstruction before considering surgical intervention (e.g., ventriculoperitoneal shunting). Constructive interference in steady state (CISS) and half-Fourier acquisition single-shot turbo spin echo (HASTE) MRI sequences suggested encystment of the fourth ventricle with thin margins of arachnoid membrane extending through the foramina of Luschka bilaterally into the pontocerebellar cistern [
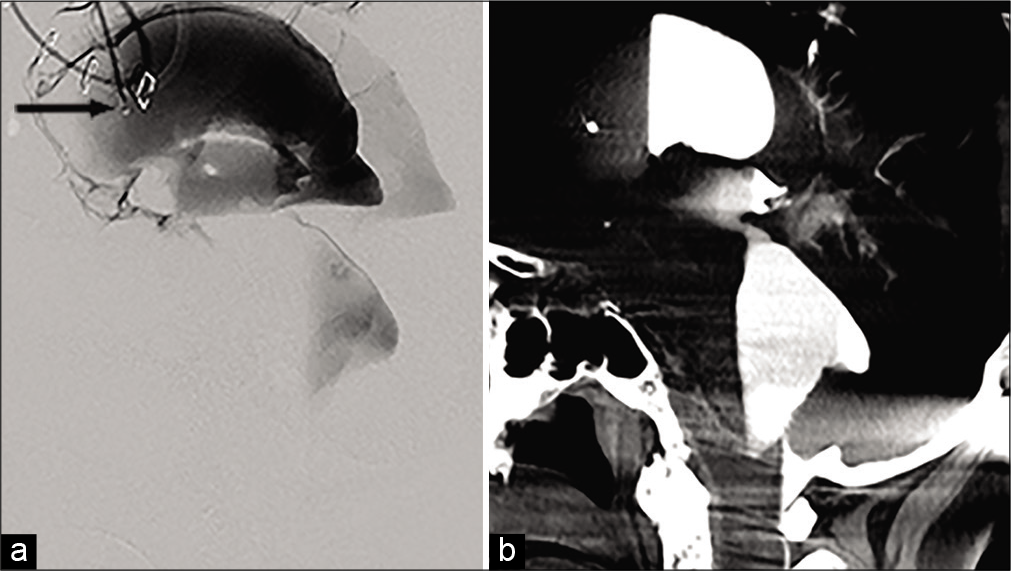
Digital subtraction cisternography demonstrated contrast outflow through the foramina of Monro and cerebral aqueduct; however, there was a paucity of flow through the preponderance of the fourth ventricle with contrast tracking peripherally along the ependymal walls and stopping just past the apertures of the foramina of Magendie and Luschka without extension into the basal cisterns [
Figure 2:
(a and b) Fluoroscopic dynamic cisternography demonstrating dilatation of the lateral and third ventricles with adequate flow through the foramina of Monro and cerebral aqueduct; however, a paucity of outflow is appreciated from the fourth ventricle through either foramina of Luschka or Magendie. The black arrow denotes the tip of the external ventricular drain catheter.
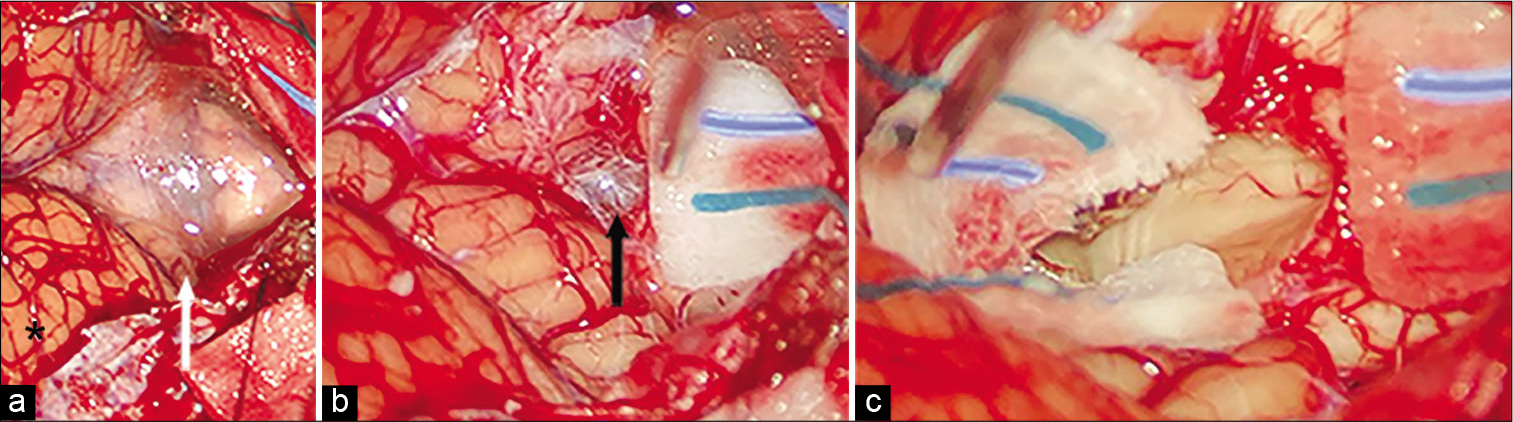
Figure 3:
(a) Initial suboccipital craniectomy exposure of the cerebellar tonsils (black asterisk) and dense, adherent arachnoid within the cistern magna (white arrow). (b) Visualization of a thick, dense, and opaque arachnoid web (black arrow) found to be obstructing the foramen of Magendie. (c) Restoration of normal cerebrospinal fluid flow through a patent foramen of Magendie after circumferential excision of the arachnoid web.
DISCUSSION
Idiopathic fourth ventricular outlet obstruction is an exceedingly rare cause of noncommunicating hydrocephalus.[
On the contrary, balanced ventricular enlargement is typically suggestive of communicating hydrocephalus, as is seen in the setting of adults with normal pressure hydrocephalus. As such, differentiating noncommunicating from communicating hydrocephalus based on imbalanced or balanced ventricular dilatation, respectively, is relatively straightforward. However, fourth ventricular outlet obstruction can also present with balanced tetraventricular hydrocephalus with the impediment of CSF flow at the outlet of the fourth ventricle to the subarachnoid space causing diagnostic difficulties. The present case demonstrated the classic findings seen in the fourth ventricular outlet obstruction including tetraventricular hydrocephalus with ballooning of all foramina, including Magendie and Luschka. Ventral displacement of the brainstem and dorsal displacement of the cerebellum are also classically associated with the diagnosis. Certainly, it is difficult to rule out fourth ventricular outlet obstruction based on conventional MRI sequences. As such, additional MRI sequences, including CISS and HASTE, may be able to confirm suspicion for membranous obstruction. For example, Dincer et al.[
The surgical management of idiopathic fourth ventricular outlet obstruction remains controversial. Numerous approaches have been documented in the literature including suboccipital craniotomy for posterior fossa exploration with excision of the membranous obstruction, endoscopic third ventriculostomy, endoscopic transventricular transaqueductal foraminoplasty of Magendie, and/or Luschka, fourth ventriculocisternostomy and ventriculoperitoneal shunting for functional treatment.[
CONCLUSION
Here, we described a rare case of idiopathic fourth ventricular outlet obstruction diagnosed with fluoroscopic dynamic cisternography and treated successfully with suboccipital craniectomy for microsurgical excision of an encountered arachnoid web. Noncommunicating hydrocephalus attributable to outlet obstruction can be misdiagnosed as communicating hydrocephalus due to conventional MRI, which lacks the sensitivity to identify membranous occlusions. The present case emphasizes the necessity in obtaining CISS sequences and fluoroscopic dynamic cisternography for suspected cases of the fourth ventricular outlet obstruction as the results of such diagnostic tests may guide surgical management strategies and lead to superior patient outcomes.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bai J, Yu Q, Sun X, Xiao H, Wang K, Sun F. Hydrocephalus due to idiopathic fourth ventricle outflow obstruction. J Craniofac Surg. 2019. 30: e397-400
2. Dincer A, Kohan S, Ozek MM. Is all. “communicating” hydrocephalus really communicating? Prospective study on the value of 3D-constructive interference in steady state sequence at 3T. AJNR Am J Neuroradiol. 2009. 30: 1898-906
3. Duran D, Hadzipasic M, Kahle KT. Mystery case: Acute hydrocephalus caused by radiographically occult fourth ventricular outlet obstruction. Neurology. 2017. 88: e36-7
4. Filippi S, Monaco P, Godano U, Calbucci F. Sialorrhea from fourth ventricle hydrocephalus. Case report. J Neurosurg. 1994. 81: 297-8
5. Ishi Y, Asaoka K, Kobayashi H, Motegi H, Sugiyama T, Yokoyama Y. Idiopathic fourth ventricle outlet obstruction successfully treated by endoscopic third ventriculostomy: A case report. Springerplus. 2015. 4: 565
6. Karachi C, Guerinel CL, Brugieres P, Melon E, Decq P. Hydrocephalus due to idiopathic stenosis of the foramina of Magendie and Luschka. Report of three cases. J Neurosurg. 2003. 98: 897-902
7. Longatti P, Fiorindi A, Martinuzzi A, Feletti A. Primary obstruction of the fourth ventricle outlets: Neuroendoscopic approach and anatomic description. Neurosurgery. 2009. 65: 1078-85
8. Mohanty A, Biswas A, Satish S, Vollmer DG. Efficacy of endoscopic third ventriculostomy in fourth ventricular outlet obstruction. Neurosurgery. 2008. 63: 905-13
9. Shimoda Y, Murakami K, Narita N, Tominaga T. Fourth ventricle outlet obstruction with expanding space on the surface of cerebellum. World Neurosurg. 2017. 100: 711.e1-5
10. Suehiro T, Inamura T, Natori Y, Sasaki M, Fukui M. Successful neuroendoscopic third ventriculostomy for hydrocephalus and syringomyelia associated with fourth ventricle outlet obstruction. Case report. J Neurosurg. 2000. 93: 326-9
11. Torres-Corzo J, Sanchez-Rodriguez J, Cervantes D, Vecchia RR, Muruato-Araiza F, Hwang SW. Endoscopic transventricular transaqueductal Magendie and Luschka foraminoplasty for hydrocephalus. Neurosurgery. 2014. 74: 426-35