- Department of Surgery, Chiang Mai University, Chiang Mai, Thailand,
- School of Medicine, University of Cambridge, Cambridge, United Kingdom.
Correspondence Address:
Jirapong Vongsfak
School of Medicine, University of Cambridge, Cambridge, United Kingdom.
DOI:10.25259/SNI_390_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jirapong Vongsfak1, Chumpon Jetjumnong1, James Cullen2. Image report: Extensive disseminated thoracolumbosacral myxopapillary ependymoma. 18-Sep-2020;11:297
How to cite this URL: Jirapong Vongsfak1, Chumpon Jetjumnong1, James Cullen2. Image report: Extensive disseminated thoracolumbosacral myxopapillary ependymoma. 18-Sep-2020;11:297. Available from: https://surgicalneurologyint.com/surgicalint-articles/10265/
Abstract
Background: Myxopapillary ependymoma occurs more frequently in adults, but is found in the first two decades of life in around 8–20% of patients. Tumors are usually benign with low likelihood for dissemination.
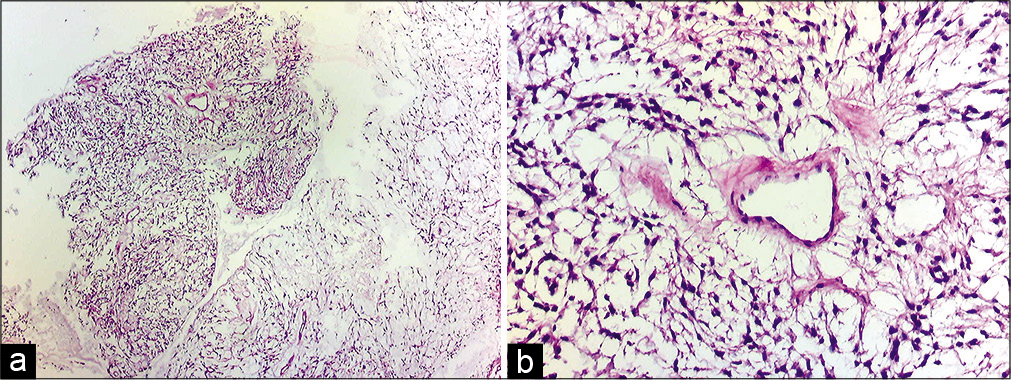
Case Description: We describe a case of a 13-year-old boy who presented with progressive kyphosis and bilateral weakness of the lower limbs. MRI shows a thoracolumbosacral intradural tumor with invasion of sacral neural foramina and dissemination to the cervicothoracic region. The patient received T10-L5 laminectomy with subtotal tumor resection. Pathological examination revealed myxopapillary ependymoma. After surgical resection, the patient underwent physical therapy with whole spinal radiotherapy for disease control.
Conclusion: Spinal myxopapillary ependymomas are usually benign and slow-growing tumors. This case illustrates an extensive and disseminated myxopapillary ependymoma.
Keywords: Disseminated, Invasive, Spinal myxopapillary ependymoma
INTRODUCTION
Intramedullary spinal cord tumors in childhood are rare. They account for only 4–6% of all CNS tumors in this age group. Among the various types of spinal cord tumors, astrocytoma and ependymoma are usually the two most common in childhood. Intramedullary spinal cord tumors in childhood are rare. They account for only 4–6% of all CNS tumors in this age group.[
CASE REPORT
A 13-year-old boy presented in 2018 with progressive kyphosis, without back pain or weakness. The patient visited orthopedic and pediatric doctors and was initially investigated for enthesitis secondary to juvenile idiopathic arthritis. However, serological workup was negative for HLA B27, rheumatoid factor, and ANA.
MRI pelvis in 2019 revealed posterior vertebral scalloping and widening of the neural foramina, which was initially misdiagnosed as dural ectasia. He was, therefore, followed up by pediatric rheumatology as an outpatient.
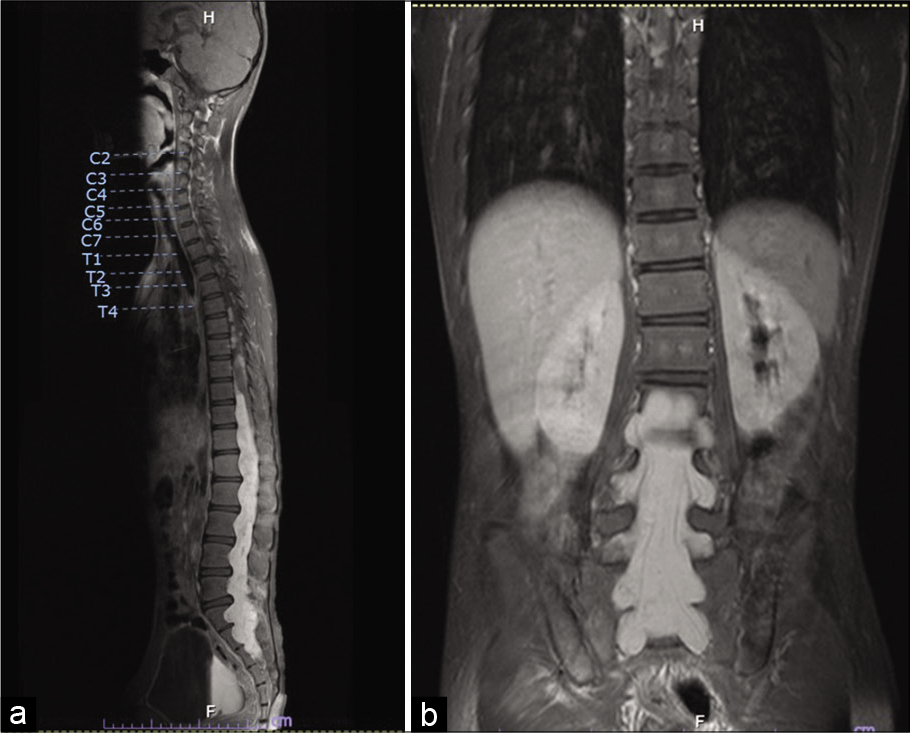
The patient gradually developed bilateral lower limb weakness and urinary incontinence and after two years presented to the neurosurgery outpatient department. Physical examination revealed kyphosis of the thoracolumbar spine. Upper limb power was Grade V throughout. Lower limb power was Grade II proximally (iliopsoas and quadriceps) and Grade I distally (tibialis anterior and extensor hallucis longus). Per rectal examination found loose anal sphincter tone and decreased perianal sensation. MRI whole spine revealed a large, expansile intradural mass that completely occupied the lumbosacral spinal canal. The tumor demonstrated T1WI hypointensity and T2WI hyperintensity as compared to the spinal cord and showed avidly homogenous enhancement postgadolinium contrast, extending from T10 to S3 and causing compression at the lower thoracic cord. The mass was not separate from conus medullaris. In the lumbar region, the mass extended into the neural foramina on both sides from L1-2 to S2-3 and the posterior vertebral bodies showed marked scalloping with mild kyphoscoliosis [
Figure 1:
Preoperative MRI whole spine: (a) a large expansile enhancing intradural mass completely occupying the lumbosacral spinal canal, extending from T10 to S3 level with posterior vertebral scalloping, causing cord compression. (b) This mass in the lumbar region extends into the neural foramina at all levels, with expansion of, and extension out of, the foramina on both sides from L1-2 to S2-3 level.
At follow-up 2 months postdischarge, the patient demonstrated reduced clinical weakness following rehabilitation. Power in the lower limbs was improved to Grade IV both proximally and distally. As of July 2020, the patient is undergoing whole spine radiotherapy for disease control. We plan to perform a lumbar puncture for CSF cytology following radiotherapy to monitor response to treatment.
DISCUSSION
Myxopapillary ependymomas are typically benign and slow-growing tumors. However, despite being low-grade tumors, MPEs have potential for dissemination within the spinal canal.[
The tumor in our report showed extensive thoracolumbar and sacral involvement, with dissemination to the cervicothoracic spinal region. Therefore, the surgical treatment was subtotal tumor resection. After surgical resection, the patient required radiotherapy for disease control.
CONCLUSION
Spinal myxopapillary ependymomas are typically benign, slow-growing tumors. However, this image report shows a case of spinal MPE with extensive and invasive behavior, extending thoracolumbosacrally with perisacral involvement and dissemination to the cervicothoracic spinal region; the patient required multimodality treatment including surgical (subtotal) resection and radiotherapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Dr. Songkiet Suwansirikul (neuropathologist) for pathology figures and reports.
References
1. Abdulaziz M, Mallory GW, Bydon M, de la Garza Ramos R, Ellis JA, Laack NN. Outcomes following myxopapillary ependymoma resection: The importance of capsule integrity. Neurosurg Focus. 2015. 39: E8
2. Fassett DR, Pingree J, Kestle JR. The high incidence of tumor dissemination in myxopapillary ependymoma in pediatric patients. Report of five cases and review of the literature. J Neurosurg. 2005. 102: 59-64
3. Kraetzig T, McLaughlin L, Bilsky MH, Laufer I. Metastases of spinal myxopapillary ependymoma: Unique characteristics and clinical management. J Neurosurg Spine. 2018. 28: 201-8
4. Straus D, Tan LA, Takagi I, O’Toole JE. Disseminated spinal myxopapillary ependymoma in an adult at initial presentation: A case report and review of the literature. Br J Neurosurg. 2014. 28: 691-3
5. Strojnik T, Bujas T, Velnar T. Invasive myxopapillary ependymoma of the lumbar spine: A case report. World J Clin Cases. 2019. 7: 1142-8