- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan.
- Department of Neurology, Imari Arita Kyoritsu Hospital, Arita, Japan.
- Department of Neurosurgery, Imari Arita Kyoritsu Hospital, Arita, Japan.
- Department of Neurospinal Surgery, Shiroishi Kyoritsu Hospital, Shiroishi, Japan.
Correspondence Address:
Tatsuya Tanaka, Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan.
DOI:10.25259/SNI_791_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tatsuya Tanaka1, Hirofumi Goto2, Nobuaki Momozaki3, Eiichiro Honda4. Incidence of radiculopathy following lumboperitoneal shunt placement without fluoroscopy for normal pressure hydrocephalus. 23-Sep-2022;13:437
How to cite this URL: Tatsuya Tanaka1, Hirofumi Goto2, Nobuaki Momozaki3, Eiichiro Honda4. Incidence of radiculopathy following lumboperitoneal shunt placement without fluoroscopy for normal pressure hydrocephalus. 23-Sep-2022;13:437. Available from: https://surgicalneurologyint.com/surgicalint-articles/11881/
Abstract
Background: Spinal catheter insertion in lumboperitoneal shunt (LPS) surgery for normal pressure hydrocephalus (NPH) can result in radiculopathy due to mechanical irritation of the nerve roots of the cauda equina. Here, we analyzed the position of LPS shunts placed without portable fluoroscopy in 72 patients, a subset of whom developed postoperative radiculopathy.
Methods: We retrospectively analyzed how frequently 72 consecutive NPH patients experienced radiculopathy following LPS catheter placement performed without intraoperative fluoroscopy.
Results: The rate of incorrect catheter placement was 15.3% (11/72 cases). We observed that is, downward placement in 6.9% (5/72 cases), hyperflexion in 6.9% (5/72 cases), and subcutaneous migration in 1.4% (1/72 cases) patients. One patient with initial correct LPS placement developed radicular pain 5-day postoperatively attributed to 1-cm of catheter movement; they recovered simply by utilizing oral analgesics for 1-month duration.
Conclusion: LPS insertion without fluoroscopic guidance resulted in a 15.3% risk of spinal catheter displacement. We suggest, therefore, that intraoperative imaging guidance be utilized for the placement of LPS in patients with NPH and/or for other pathology to avoid the 15.3% risk of postoperative radiculopathy.
Keywords: Complication, Fluoroscopic-guided surgery, Lumboperitoneal shunt, Normal pressure hydrocephalus, Radiculopathy, Spinal catheter
INTRODUCTION
Prior reports cited a 5–6% incidence of new postoperative radiculopathy attributed to mechanical irritation of the cauda equina after lumboperitoneal shunt (LPS) placement for patients with normal pressure hydrocephalus (NPH).[
MATERIALS AND METHODS
Clinical and radiographic data
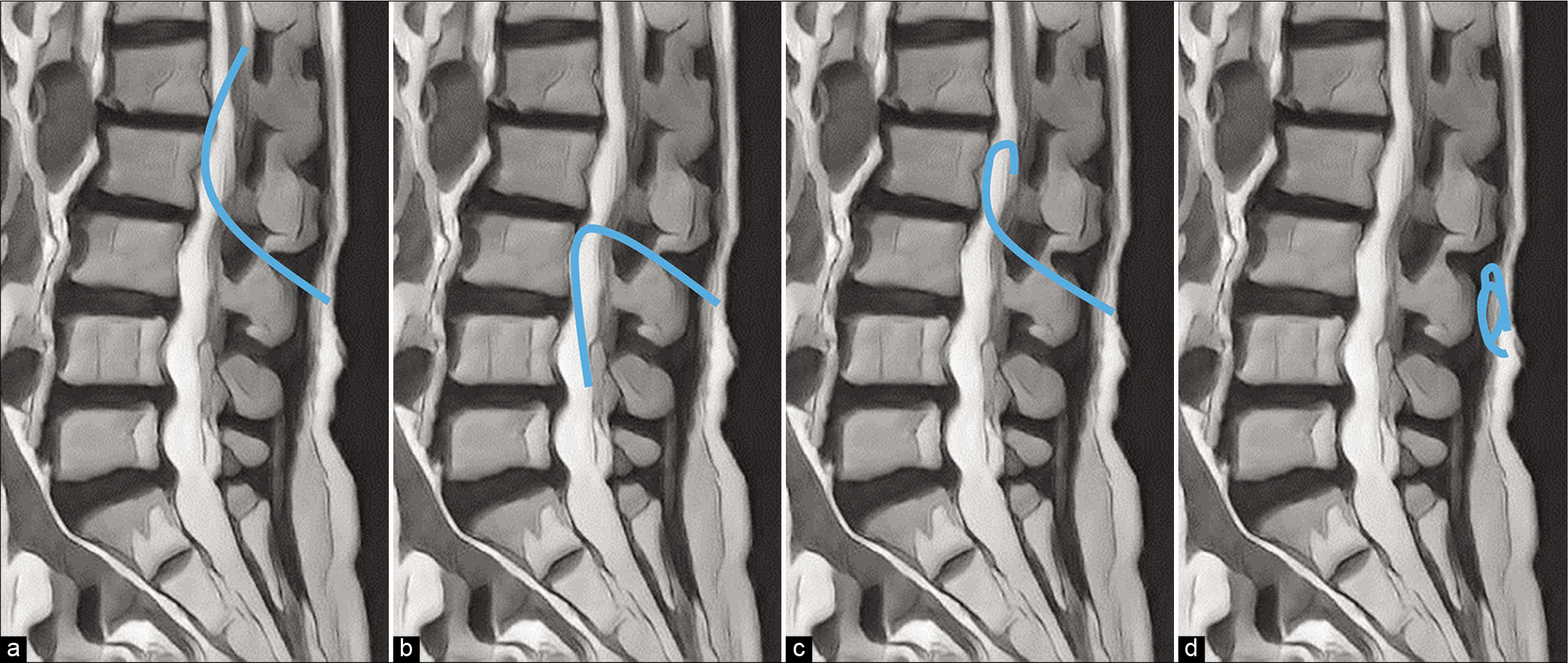
From 2012 to 2016, 72 consecutive patients underwent LPS placement without fluoroscopy for NPH. All patients had an LPS (i.e., pressure programmable valves with anti-siphon devices) placed while in the left lateral decubitus position under general anesthesia. A lumbar catheter was inserted at 13–15 cm from the fascia without fluoroscopy. The valve was initially set at the highest opening pressure. Postprocedural imaging of LPS placement was verified with X-ray or computed tomography imaging and graded into four categories: (1) upward placement (correct placement), (2) downward placement, (3) hyperflexion, and (4) subcutaneous migration [
RESULTS
Postprocedural imaging showed that 11 of 72 (15.3%) patients had spinal catheters incorrectly placed; that is, five with downward placement (6.9%); five with hyperflexion(6.9%); and one with subcutaneous migration (i.e., subsequently required catheter repositioning) (1.4%). Patients with incorrect LPS placement were followed for a minimum of 1 postoperative year, and none had symptoms/ signs related to distal spinal cord damage. One patient with a correctly positioned LPS had radicular pain develop 5-day postoperatively attributed to 1-cm catheter movement; however, no reoperation was required as the patient’s symptoms resolved within 1 postoperative month later on oral analgesics [
Figure 2:
Preoperative spine magnetic resonance imaging (a) showing no spinal canal stenosis. Postoperative spine sagittal computed tomography (CT) (b) shows the correct placement of the spinal catheter (A arrow). Postoperative spine sagittal CT on day 20 (c) shows the catheter moved up 1 cm through the spinal canal (C arrowhead).
DISCUSSION
This study demonstrated that without intraoperative fluoroscopic guidance, LPS insertion can result in a 15.3% incidence of spinal catheter malpositioning. Therefore, intraoperative imaging guidance should likely be utilized for the future placement of LPS in patients with NPH or requiring LPS to address other pathologies. Three additional suggestions for placing LPS under fluoroscopic guidance include; suturing the catheter to the fascia, using a thinner spinal catheter, and avoiding LPS placement in patients with significant spinal stenosis. In SINPHONI trials, after 87 LPS procedures, 6 revisions (7%) were required; just one out of 100 patients treated with ventriculoperitoneal shunt placement required a revision.[
CONCLUSION
LPS insertion without fluoroscopic guidance for NPH resulted in a 15.3% risk of spinal catheter misplacement. Interestingly, radiculopathy developed 5 days after LPS placement due to delayed spinal catheter migration.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
References
1. Aoki N. Lumboperitoneal shunt: Clinical applications, complications, and comparison with ventriculoperitoneal shunt. Neurosurgery. 1990. 26: 998-1003
2. Eisenberg HM, Davidson RI, Shillito J. Lumboperitoneal shunts. Review of 3 cases. J Neurosurg. 1971. 35: 427-31
3. Izutsu N, Hosomi K, Kawamoto S, Khoo HM, Yanagisawa T, Tani N. Lumbar catheter misplacement into the spinal subdural epiarachnoid space causing lumboperitoneal shunt malfunction: Report of two cases. NMC Case Rep J. 2021. 8: 183-7
4. Miyajima M, Kazui H, Mori E, Ishikawa M. One-year outcome in patients with idiopathic normal-pressure hydrocephalus: comparison of lumboperitoneal shunt to ventriculoperitoneal shunt. J Neurosurg. 2016. 125: 1483-92
5. Wang VY, Barbaro NM, Lawton MT, Pitts L, Kunwar S, Parsa AT. Complications of lumboperitoneal shunts. Neurosurgery. 2007. 60: 1045-8