Initial experience of subcutaneous nitroglycerin for distal transradial access in neurointerventions
- Department of Neurological Surgery, SUNY Upstate Medical University, Syracuse, New York, United States.
- Department of Neurological Surgery, Ohio State University Hospital, Columbus, Ohio, United States.
- Department of Neurological Surgery, Upstate Medical University Hospital, Syracuse, New York, United States.
Correspondence Address:
Maham Ahmed, SUNY Upstate Medical University, Syracuse, New York, United States.
DOI:10.25259/SNI_711_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Maham Ahmed1, Stephanie Zyck2, Grahame C. Gould3. Initial experience of subcutaneous nitroglycerin for distal transradial access in neurointerventions. 11-Oct-2021;12:513
How to cite this URL: Maham Ahmed1, Stephanie Zyck2, Grahame C. Gould3. Initial experience of subcutaneous nitroglycerin for distal transradial access in neurointerventions. 11-Oct-2021;12:513. Available from: https://surgicalneurologyint.com/surgicalint-articles/11170/
Abstract
Background: Transradial access (TRA) for diagnostic and interventional neuroendovascular procedures has gained significant popularity in recent years due to its improved safety profile and appeal to patients compared with transfemoral access. However, risks of TRA include hand ischemia in cases of poor ulnar collateral circulation and inability to cannulate the radial artery due to its relatively small diameter. By accessing the radial artery distal to the superficial palmar arch where ulnar collateral blood flow arises, in the anatomic snuffbox, the risk of hand ischemia is theoretically eliminated. The use of subcutaneous nitroglycerin and lidocaine to improve rates of success in radial artery access has been reported in the cardiac literature, however, has yet to be described for neurointerventional procedures. We discuss our technique and report our initial experience using subcutaneous nitroglycerin and lidocaine cocktail for access to the distal transradial artery in a variety of neuroendovascular procedures.
Methods: A retrospective review of our institution’s database of neurointerventional and diagnostic procedures performed using dTRA was conducted, and 64 patients were identified between February and December 2020. Patient demographics, clinical data, procedural details, and radiographic information were collected and analyzed.
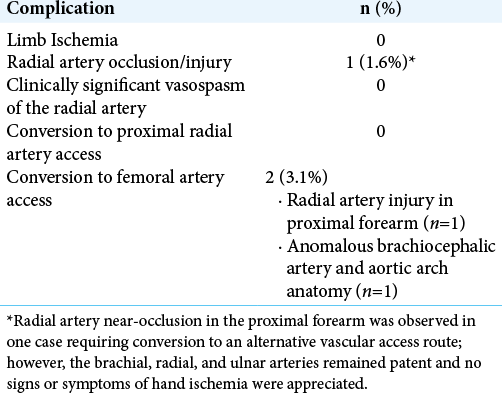
Results: A total of 64 patients underwent neurointerventional procedures using the subcutaneous injection for dTRA access. The procedures performed included diagnostic cerebral angiograms (n = 47), stent and balloon assisted aneurysm coiling (n = 5), flow diversion (n = 2), intra-saccular device placement (n = 1), mechanical thrombectomy (n = 1), tumor embolization (n = 1), middle meningeal artery embolization (n = 2), extracranial carotid stent placement (n = 2), and arteriovenous malformation embolization (n = 3). While no complications of hand ischemia were appreciated, the access site conversion rate was 3.1%; 2 cases required a switch to femoral artery access due to proximal vessel tortuosity and aortic anatomical variations, and not due to access site complication. Furthermore, on repeat angiograms by the same proceduralist, distal TRA (dTRA) was successful in 100% of the cases.
Conclusion: dTRA using subcutaneous nitroglycerin and lidocaine is a safe and effective method for neurointerventional and diagnostic procedures.
Keywords: Anatomic snuffbox access, Aneurysm, Distal transradial access, Neurovascular intervention, Nitroglycerine and lidocaine subcutaneous infusion
INTRODUCTION
Transradial access (TRA) for diagnostic and interventional neuroendovascular procedures has gained significant popularity in recent years due to its improved safety profile and appeal to patients compared with conventional transfemoral access (TFA).[
However, potential issues with TRA include radial artery occlusion and post procedural hand-ischemia due to poor ulnar collateral circulation, as well as ergonomic challenges in use of the left side.[
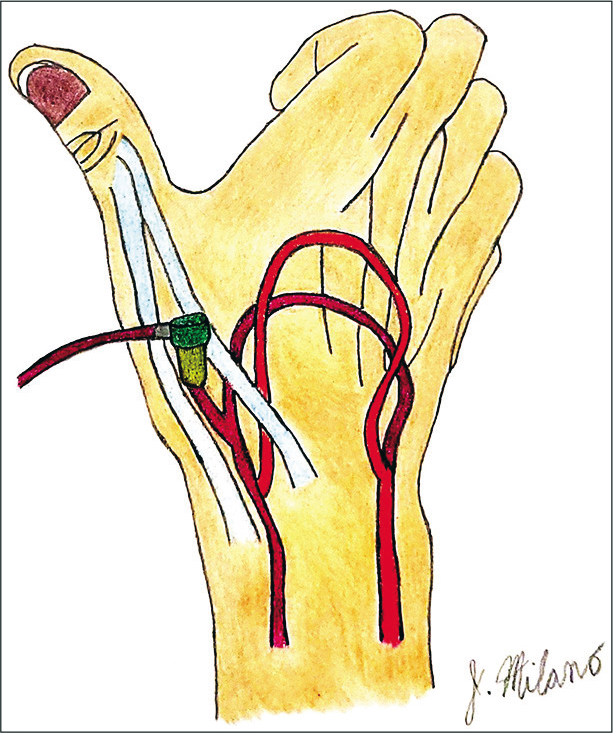
Figure 1:
Distal transradial access is demonstrated in the anatomical snuffbox, formed by the tendons of extensor pollicis longus (medially) and extensor pollicis brevis and abductor pollicis longus(laterally). The deep palmar arch(DPA)[Dark red] and superficial palmar arch (SPA) [Light red] portray an elaborate network of anastomosis, with the DPA providing the distal branch into the anatomical snuffbox. These features account for the patency of proximal vessels for future access and the lack of complication of hand-ischemia.
dTRA has been successfully used for both diagnostic and interventional neuroendovascular procedures. In a series of diagnostic cerebral angiograms by Brunet et al., 100% of the right distal radial arteries were successfully accessed without any complications, although 8.2% of patients had required conversion to standard TRA (1.2%) or TFA (7.0%).[
A retrospective series of neurointerventions utilizing dTRA by Kühn et al. included aneurysm embolization, carotid artery stenting, and arteriovenous fistula embolization. There was a reported 10.4% conversion to TFA due to vascular tortuosity and “limited support of the catheter in the aortic arch.” Radial artery vasospasm was noted and treated successfully with anti-spasmolytics in two cases (4.2%). Nevertheless, there was no report of radial artery occlusion or ischemic episode and the study concluded dTRA to be a safe and effective approach for various neurointerventions.[
One of the most commonly reported reasons for failure of dTRA in neuroendovascular procedures is radial artery vasospasm, for which no standard antispasmodic and/or vasodilator drug protocol currently exists.[
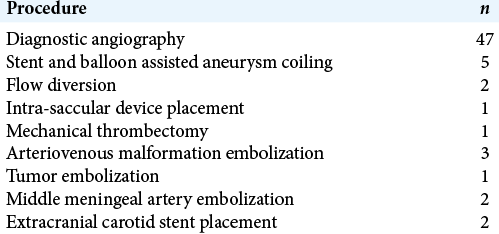
MATERIALS AND METHODS
This study was approved by our hospital institutional review board.
A retrospective review of our institutionns database of neurointerventional and diagnostic procedures performed using dTRA was conducted, and 64 patients were identified between February and December 2020. Patient demographics, clinical data, procedural data, and radiographic information were collected and analyzed. [
RESULTS
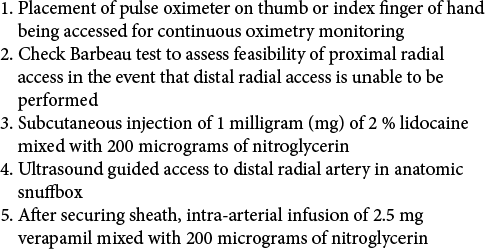
A total of 64 patients were included for analysis. Of those patients, 50% were male and the mean age was 56 years (range 16–81 years). The interventional procedures included mechanical thrombectomy, stenting (extracranial carotid and intracranial), embolization (coil, balloon-assisted coil, liquid embolic, woven endobridge), and flow diversion (Pipeline [Medtronic, Dublin, Ireland]), as listed in [
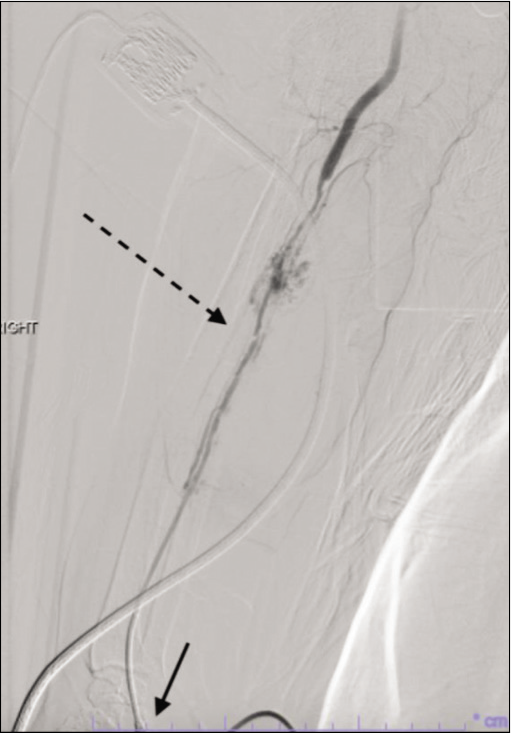
Vascular access through the anatomical snuffbox was successful in 100% of the patients, although two patients (3.1%) required conversion to the transfemoral approach (TFA). Conversion to TFA occurred due to near occlusion of the proximal radial artery in one patient [
Figure 2:
Right radial artery angiography in one case demonstrates near occlusion of the radial artery with a small area of contrast extravasation in the proximal forearm after advancement of a 0.035 inch glidewire (Terumo, Somerset, NJ). The vascular access site is seen distally in the anatomic snuffbox (short solid arrow) and the area of near-occlusion is seen in the proximal forearm (long dashed arrow). The brachial and ulnar arteries remained patent. Radial artery access was aborted and the procedure was completed through a transfemoral route.
DISCUSSION
The limitations of proximal radial artery access for neurointerventional procedures are being improved on by use of the distal radial artery for vascular access. Use of the distal branch in the anatomic snuffbox leads to decreased complication rates and patient satisfaction as compared to traditional TRA and TFA. Nevertheless, guidelines across the nation are in the favor of the traditional access via the proximal forearm and the groin due to the relatively lesser data on the use of dTRA.[
With increasing reports of the use of distal transradial approach, the main reported complication of the occlusion of the radial artery can be countered through pharmacologically preventing arterial vasospasm and increasing vessel diameter. Our case series reports the use of a novel drug cocktail of subcutaneous nitroglycerine and lidocaine at the cannulation site, so as to allow of an enhanced vasodilatory effect on the radial artery, in addition to the intra-arterial infusion of nitroglycerin and verapamil. While subcutaneous infusion of a calcium channel blocker and nitroglycerin has been reported to aide in radial artery vasospasm for various types of procedures; to the best of our knowledge, we are the first to report a standardized protocol for its use in both diagnostic and interventional cerebral angiography in addition to the previously reported intra-arterial antispasmodic infusion.[
Notably, the two cases in our series that required conversion to TFA were due to more proximal anatomic anomalies and not due to the vasospasm of the cannulation site itself. Furthermore, no occlusion was appreciated on repeat angiograms performed by the same proceduralist, and distal radial artery was successfully accessed in 100% of the repeat cases. Thus, subcutaneous nitroglycerin and lidocaine infusion before radial artery cannulation are an easy and effective way to increase the arterial diameter and prevent vasospasm, contributing to our low access-site conversion rate of 3.1% (n = 2), which is on the low end of the range of 0.3–11% reported in the literature (Kühn et al.)
This study is limited by its retrospective nature and relatively small sample size; however, despite those limitations, we believe that this series demonstrate our protocol relatively small sample size contributing trther study may include larger comparative studies with and without the subcutaneous infusion for neurointerventional procedures using dTRA to further strengthen or debunk the current evidence supporting its use.
CONCLUSION
dTRA using subcutaneous nitroglycerin and lidocaine is a safe, easy, and effective method for neurointerventional and diagnostic procedures.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
References
1. Brunet M, Chen S, Sur S, McCarthy DJ, Snelling B, Yavagal DR. Distal transradial access in the anatomical snuffbox for diagnostic cerebral angiography. J Neurointerv Surg. 2019. 11: 710-3
2. Cai G, Huang H, Li F, Shi G, Yu X, Yu L. Distal transradial access: a review of the feasibility and safety in cardiovascular angiography and intervention. BMC Cardiovasc Disord. 2020. 20: 356
3. Curtis E, Fernandez R, Lee A. The effect of vasodilatory medications on radial artery spasm in patients undergoing transradial coronary artery procedures: A systematic review. JBI Database System Rev Implement Rep. 2017. 15: 1952-67
4. Hefnawy E, Alrefaey A. Sonographic evaluation of peri-arterial nitroglycerine for radial artery cannulation in morbidly obese patients: A prospective randomized study. Ain-Shams J Anesthesiol. 2018. 10: 1-5
5. Hoffman H, Jalal MS, Masoud HE, Pons RB, Caamaño IR, Khandelwal P. Distal transradial access for diagnostic cerebral angiography and neurointervention: Systematic review and meta-analysis. AJNR Am J Neuroradiol. 2021. 42: 888-95
6. Koutouzis M, Kontopodis E, Tassopoulos A, Tsiafoutis I, Katsanou K, Rigatou A. Distal versus traditional radial approach for coronary angiography. Cardiovasc Revasc Med. 2019. 20: 678-80
7. Kühn A, de Macedo Rodrigues K, Singh J, Massari F, Puri A. Distal radial access in the anatomical snuffbox for neurointerventions: A feasibility, safety, and proof-of-concept study. J Neurointerv Surg. 2020. 12: 798-801
8. Matsumoto Y, Hokama M, Nagashima H, Orz Y, Toriyama T, Hongo K. Transradial approach for selective cerebral angiography: Technical note. Neurol Res. 2000. 22: 605-8
9. McCarthy D, Chen S, Brunet M, Shah S, Peterson E, Starke R. Distal radial artery access in the anatomical snuffbox for neurointerventions: Case report. World Neurosurg. 2019. 122: 355-9
10. Rajah GB, Lieber B, Kappel AD, Luqman AW. Distal transradial access in the anatomical snuffbox for balloon guide-assisted stentriever mechanical thrombectomy: Technical note and case report. Brain Circ. 2020. 6: 60-4
11. Saito S, Hasegawa H, Ota T, Takino T, Yoshida Y, Ando K. Safety and feasibility of the distal transradial approach: A novel technique for diagnostic cerebral angiography. Interv Neuroradiol. 2020. 26: 713-8
12. Wang Z, Xia J, Wang W, Xua G, Gua J, Wang Y. Transradial versus transfemoral approach for cerebral angiography: A prospective comparison. J Interv Med. 2019. 2: 31-4