- Department of Neurosurgery, SUNY Upstate Medical University, Syracuse, New York, United States.
DOI:10.25259/SNI_96_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Brandon Michael Wilkinson, Michael Galgano. Instrumentation following intradural tumor resection: A case analyses and literature review. 30-May-2020;11:131
How to cite this URL: Brandon Michael Wilkinson, Michael Galgano. Instrumentation following intradural tumor resection: A case analyses and literature review. 30-May-2020;11:131. Available from: https://surgicalneurologyint.com/surgicalint-articles/10058/
Abstract
Background: Resection of intradural spinal tumors typically utilizes a posterior approach and often contributes to significant biomechanical instability and sagittal deformity.
Methods: We searched PubMed for studies regarding pre- and postoperative spine biomechanics/alignment in patients with intradural tumors undergoing posterior decompressions.
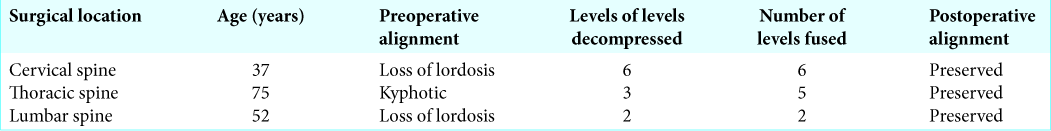
Results: Three patients underwent posterior decompressions with instrumented fusions to preserve good sagittal alignment postoperatively. Variables analyzed in this study included the extent of preoperative and postoperative deformity, the number of surgical levels decompressed and fused, the different frequencies of instability following the resection of cervical versus thoracic versus lumbar lesions, and whether pediatric patients were most likely to develop instability.
Conclusion: Simultaneously performing instrumented fusions following posterior spinal decompressions for tumor removal proved optimal in preventing postoperative spinal deformity. Further, “open” surgical procedures offered more optimal/definitive tumor removal versus minimally invasive approaches, and the greater operative exposure and resultant increased risk for instability were remediated by performing simultaneous fusion.
Keywords: Instrumentation, Intradural, Spine, Tumor
INTRODUCTION
Approximately 45% of spinal canal tumors are intradural; roughly 40% are extramedullary and 5% are intramedullary in location.[
After the resection of intradural tumors, the cervical spine appears to be more vulnerable to instability than the thoracic or lumbar spine (e.g. risk of post laminectomy kyphosis).[
CASE PRESENTATIONS
Case presentation #1
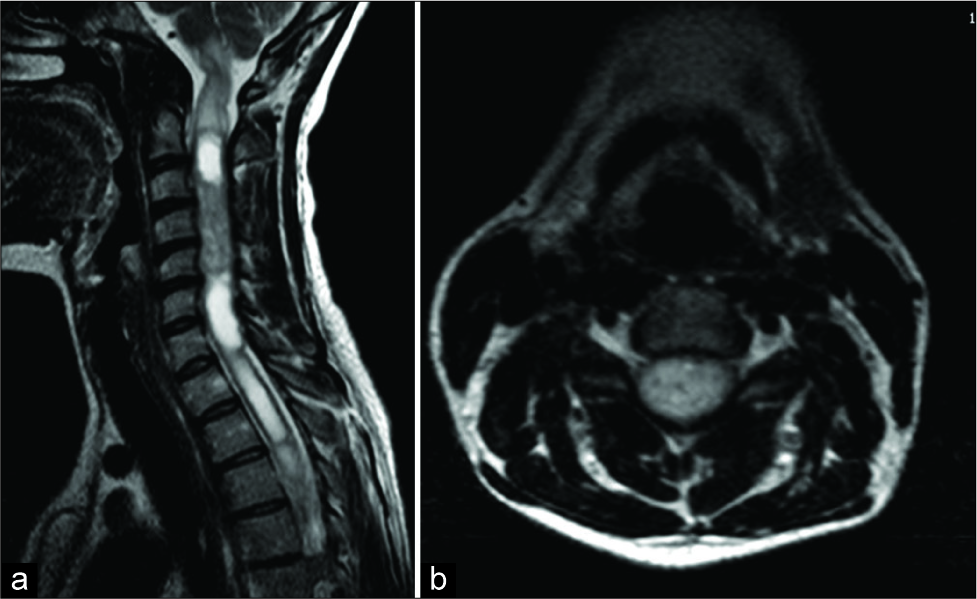
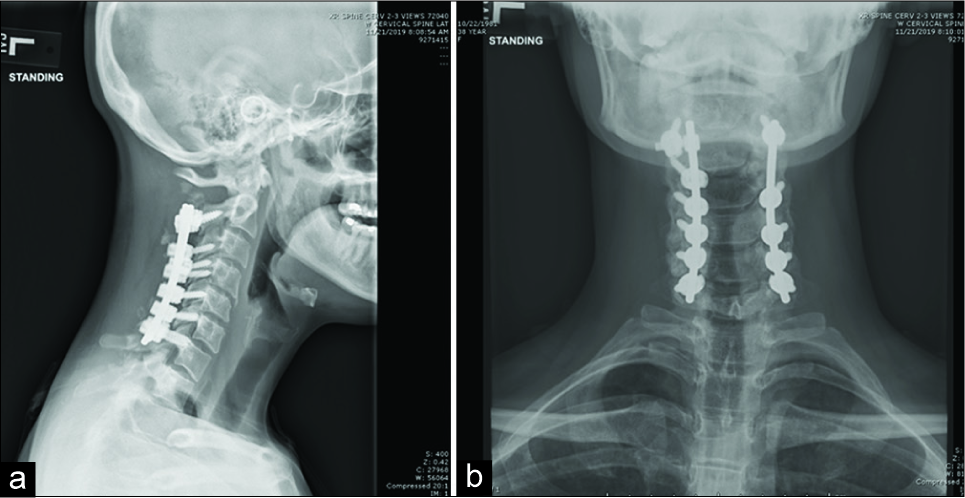
A 37-year-old female presented with 1 year of neck pain and bilateral upper extremity radiculopathy. An MRI revealed an intramedullary lesion extending from C2 to C6 with associated syrinx [
Case presentation #2
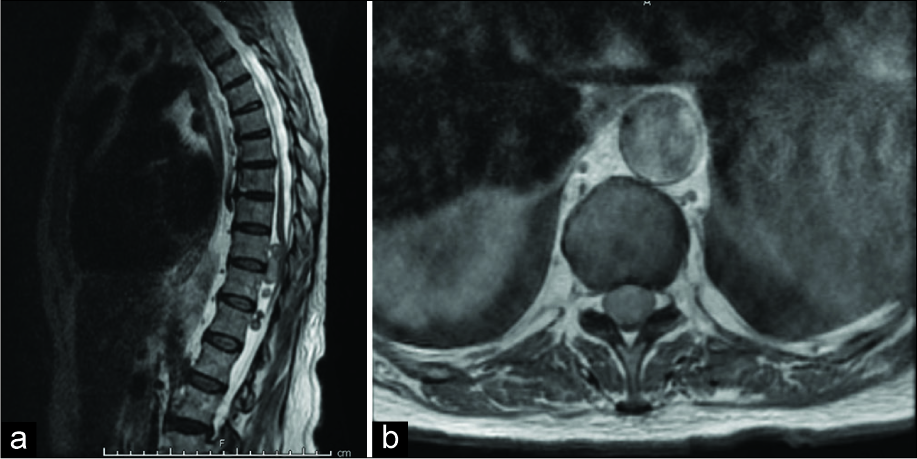
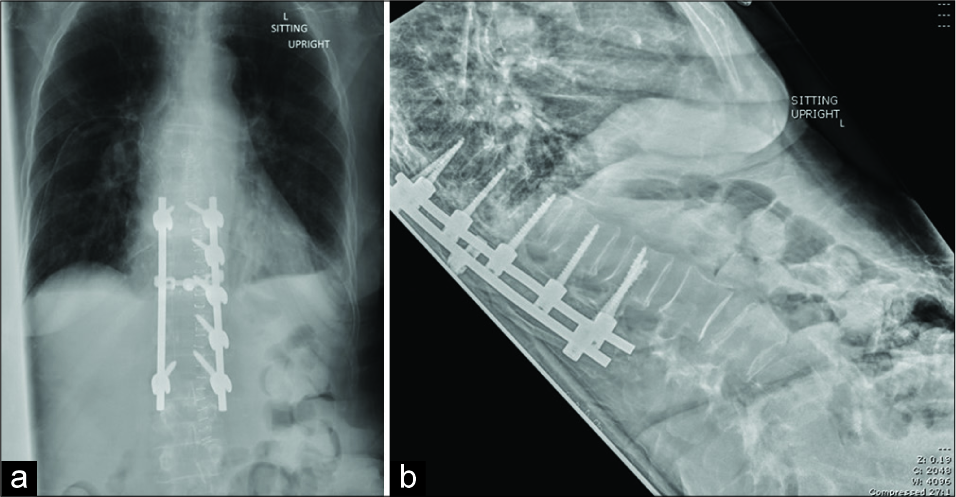
A 75-year-old female presented with several weeks of paresis and urinary incontinence. The MRI revealed five intradural tumors between T10 and T12 [
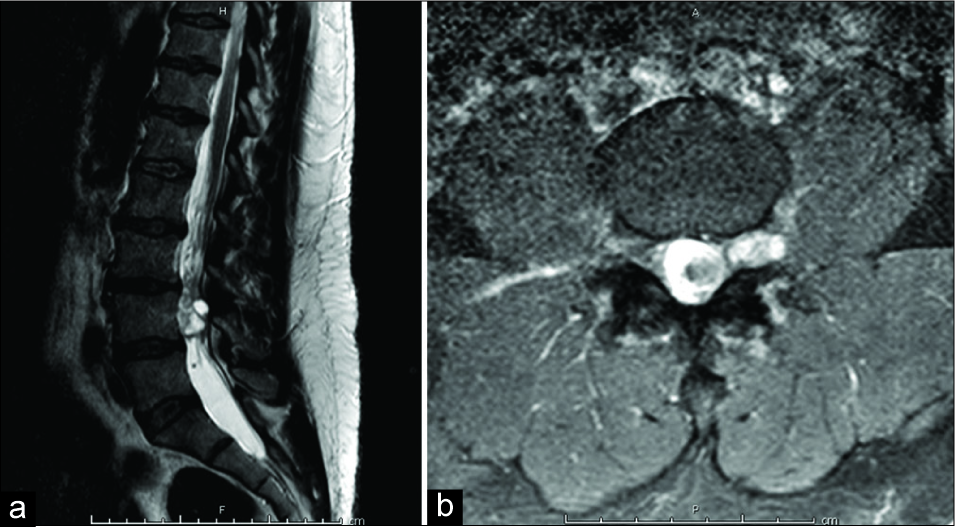
Figure 3:
(a) Sagittal T2 MRI of the thoracic spine showing five intradural extramedullary masses at the levels of T10–T12. (b) Axial T1 MRI with contrast showing uniformly enhancing circumscribed lesion at the level of T10, causing severe mass effect on the spinal cord with near-complete flattening.
Case presentation #3
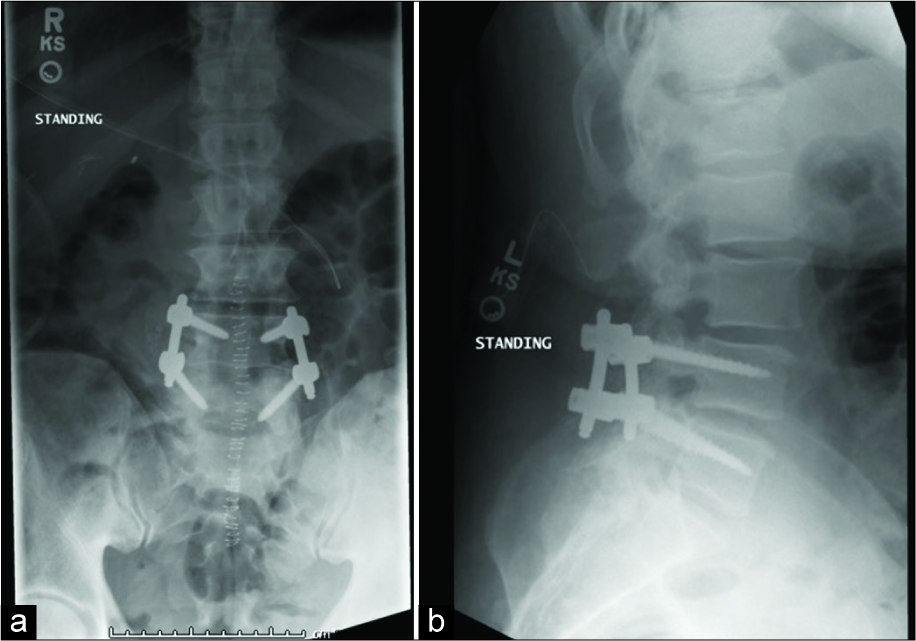
A 52-year-old male presented with a 1-year history of back pain radiating to the posterior thighs and feet. The MRI revealed an intradural extramedullary lesion at the L4 level [
DISCUSSION
When resection of intradural spinal tumors necessitates the significant disruption of posterior column elements, patients may require simultaneous fusion to avoid instability. The cervical spine appears most vulnerable followed by the thoracic and then lumbar spine.[
Preoperative cervical kyphosis increases the risk that after cervical tumor resection, a cervical fusion will be warranted. Fusion should also be considered when C2 posterior elements are disrupted, as this leads to further instability.[
Removal of one-third to half of a facet joint complex, especially in the lumbar spine, does not cause significant instability.[
In our series of cases, “open” surgical approaches offered more optimal tumor removal versus minimally invasive techniques. The increased instability associated with posterior column disruption was mitigated by performing simultaneous instrumented fusions with successful prevention of postoperative spinal deformity.
CONCLUSION
Cervical spine location, pre-operative kyphosis, patient age, and number of levels decompressed appear to be the most significant risk factors for developing post-operative instability. Concomitant instrumented fusion following posterior spinal decompression for intradural tumor removal allows for maximal resection while preventing post-operative spinal deformity.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahmad FU, Frenkel MB, Levi AD. Spinal stability after resection of nerve sheath tumors. J Neurosurg Sci. 2017. 61: 355-64
2. Allen BL, Ferguson RL. The Galveston experience with L-rod instrumentation for adolescent idiopathic scoliosis. Clin Orthop Relat Res. 1988. 229: 59-69
3. Benzel EC. The essentials of spine biomechanics for the general neurosurgeon. Clin Neurosurg. 2003. 50: 86-177
4. Guan Y, Yoganandan N, Pintar FA, Maiman DJ. Effects of total facetectomy on the stability of lumbosacral spine. Biomed Sci Instrum. 2007. 43: 81-5
5. Hersh DS, Iyer RR, Garzon-Muvdi T, Liu A, Jallo GI, Groves ML. Instrumented fusion for spinal deformity after laminectomy or laminoplasty for resection of intramedullary spinal cord tumors in pediatric patients. Neurosurg Focus. 2017. 43: E12-
6. Katsumi Y, Honma T, Nakamura T. Analysis of cervical instability resulting from laminectomies for removal of spinal cord tumor. Spine (Phila Pa 1976). 1989. 14: 1171-6
7. Knafo S, Court C, Parker F. Predicting sagittal deformity after surgery for intramedullary tumors. J Neurosurg Spine. 2014. 21: 342-7
8. Raynor RB, Pugh J, Shapiro I. Cervical facetectomy and its effect on spine strength. J Neurosurg. 1985. 63: 278-82
9. Van Goethem JW, van den Hauwe L, Ozsarlak O, De Schepper AM, Parizel PM. Spinal tumors. Eur J Radiol. 2004. 50: 159-76