- Department of Neurosurgery, Hospital Central Sur de Alta Especialidad, Mexico City, Mexico.
- Department of Neurosurgery, Hospital Central Norte, PEMEX, Mexico City, Mexico.
Correspondence Address:
Daniel Alejandro Vega-Moreno
Department of Neurosurgery, Hospital Central Sur de Alta Especialidad, Mexico City, Mexico.
DOI:10.25259/SNI_885_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daniel Alejandro Vega-Moreno1, Antonio Aviles-Aguilar2, Abraham Ibarra de la-Torre1, José Ramón Aguilar-Calderón1, Ulises García-González1, José Omar Santellán-Hernández1, Carlos Betancourt-Quiroz1, Mario Alberto Dueñas-Espinoza1, Ivan Eduardo González-González1, Rodolfo Pedro Molina-Martínez1, Diego Ochoa-Cacique1. Intracranial hypertension syndrome secondary to internal jugular vein thrombosis due to miliary cervical tuberculosis: A case report. 28-Jan-2021;12:32
How to cite this URL: Daniel Alejandro Vega-Moreno1, Antonio Aviles-Aguilar2, Abraham Ibarra de la-Torre1, José Ramón Aguilar-Calderón1, Ulises García-González1, José Omar Santellán-Hernández1, Carlos Betancourt-Quiroz1, Mario Alberto Dueñas-Espinoza1, Ivan Eduardo González-González1, Rodolfo Pedro Molina-Martínez1, Diego Ochoa-Cacique1. Intracranial hypertension syndrome secondary to internal jugular vein thrombosis due to miliary cervical tuberculosis: A case report. 28-Jan-2021;12:32. Available from: https://surgicalneurologyint.com/surgicalint-articles/10551/
Abstract
Background: Thrombosis of the internal jugular vein (IJV) is extremely rare, being central catheterization the most common cause. We present a case of a patient with an unusual appearance of neurological symptoms as a consequence of thrombosis of the IJV secondary to miliary tuberculosis.
Case Description: A 30-year-old woman with disseminated tuberculosis, with multiple lymphadenopathy, axillary, cervical, mesenteric, retroperitoneal, and inguinal, presented with clinical evidence of intracranial hypertension. A diagnostic cerebral angiography was performed, which revealed an occluded left internal jugular and venous stasis in the entire cerebral venous system. The patient was treated with low-molecular-weight heparin, with which she had an adequate evolution.
Conclusion: Tuberculosis is capable of generating a state of hypercoagulability, in addition to a mechanical compression effect due to cervical lymphadenopathy. We report an unusual clinical presentation, with intracranial involvement due to IJV thrombosis secondary to miliary tuberculosis. So far, there are no cases with a similar presentation described above.
Keywords: Internal jugular vein thrombosis, Intracranial hypertension syndrome, Miliary tuberculosis
INTRODUCTION
The first description of an internal jugular vein (IJV) thrombosis was made by Long in 1912, due to a complication of a peritonsillar abscess. Being the iatrogenic the most common causes, by catheterization of IJV and repetitive infections in intravenous drug users.[
To date, very few series have analyzed the form of presentation, morbidity, and mortality of this condition. One of the first series was published by Ascher et al. on 2005 where 60% of the patients had central venous catheterization as a risk factor, 38% had multiple risk factors, 22% some type of coagulopathy, 23% some metastatic neoplasia, and 14% some localized neoplasia.[
We present the case of a patient with an unusual appearance of neurological symptoms associated with increased venous pressure as a consequence of thrombosis of the IJV as well as of the brachiocephalic and left subclavian trunk secondary to miliary tuberculosis.
CASE REPORT
A 30-year-old woman with no history of chronic diseases, no drug use. She went to the emergency department with an acute abdominal pain, an exploratory laparotomy was performed, finding multiple peritoneal adenopathy, with histopathology report of peritoneal tuberculosis. In search of the primary focus, a three-region tomography was performed, in which multiple lymphadenopathies were found: axillary, cervical, mesenteric, retroperitoneal, and inguinal, as shown in [
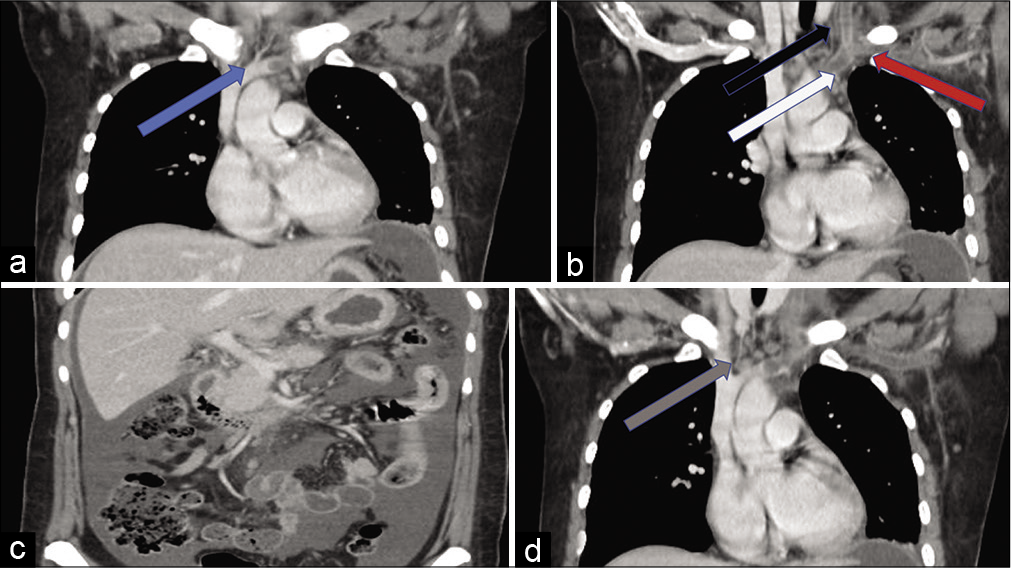
Figure 1:
Contrasted computed tomography in coronal section of cervical and abdominal region. (a) Blue arrow, occlusion of the left innominate vein behind the sternal manubrium. (b) Black arrow, hypodensity of the left internal jugular vein. Red arrow, hypodensity of the left subclavian vein. White arrow, hypodensity of the left innominate vein. (c) Multiple retroperitoneal and mesenteric adenopathy. (d) Gray arrow, perivenous cervical lymphadenopathy.
Four days later, presented with occipital headache predominantly right retroauricular, oppressive, of sudden onset, associated with nausea, vomiting, phosphenes, and tinnitus. One day later, the patient presented numbness in the right arm, pain, and edema. A neck ultrasound was requested, which reported multiple cervical lymphadenopathy and partial occlusion of the left IJV. Physical examination revealed a 15-point Glasgow, bilateral papilledema, with painful ophthalmoplegia. No meningeal signs. Hyperemic right limb with hyperesthesia and edema. In addition to increased thoracic superficial venous circulation.
Given the clinical suspicion of cerebral venous thrombosis due to occlusion of the IJV, a diagnostic cerebral angiography study was performed. With findings of the absence of venous flow in the left internal jugular to the left brachycephalic trunk, dilatation of the left external jugular vein, and increased volume of the right IJV; in addition to slowing in the late venous phase of contrast medium clearance as shown in [
The patient was treated with low-molecular-weight heparin, adjusted to her weight. After the start of treatment, the patient reported an improvement in the headache and clinically edema and pain in the right arm decreased. In the angiographic control [
DISCUSSION
Gbaguidi et al. have of the few series and cases that have analyzed the clinic presentation of IJV thrombosis. A total of 29 patients were analyzed, giving as a result that the edema of the affected limb is the most frequent clinic presentation form, with 65% followed by pain in 51% and 20% collateral superficial venous increase.[
The diagnosis under suspicion of this pathology, even in its classic form of presentation, has been reported in 4 days–3 weeks. In the case of a clinical presentation with brain involvement, the presence of occipital headache with radiation to the neck, as well as an inability to mobility, has been reported as a form of clinical appearance.[
A form of classification has been devised depending on the specific location, divided into groups: Group I with subclavian and axillary involvement, Group II internal jugular only, and Group III a combination of both.[
On the other hand, tuberculosis per se can contribute to these three characteristics previously described by Virchow. Stasis due to the mechanical effect of cervical ganglion masses, vascular injury and its known effect on the tuberculosis bacillus to generate a state of hypercoagulability that seems to develop secondary to the acute phase response.[
A variety of sequelae and complications can occur in patients with localized or disseminated tuberculosis, including parenchymal lesions, mediastinal lesions, vascular lesions, and therefore be occasionally complicated by venous thromboembolism.[
Various mechanisms have been postulated for infections causing deep vein thrombosis. These mechanisms include local invasion of surrounding tissues by infective agent, inflammation, direct endothelial damage, and induction of a transient hypercoagulable state.[
Regarding the management of this pathology, screening to avoid complications is the most important aspect. Once detected antituberculous treatment should be immediately started in addition to anticoagulant therapy. The optimum duration of anticoagulation in IJV thrombosis is not yet standardized.[
In our description, we can say that these factors were present and originated this thrombosis, as dissemination of the bacillus, direct endothelial damage from cervical lymphadenopathies and direct mechanical obstruction.
CONCLUSION
This case illustrates an unusual presentation of a rather rare pathology. Jugular venous obstruction associated to disseminate tuberculosis, in our case, generated a state of intracranial hypertension syndrome due to thrombosis of the left IJV. The neurological symptoms of this patient could have explained mainly by the decreased venous flow at the intracranial level. Fortunately, early detection, due to the neurological component, allowed a definitive diagnosis, avoiding cerebral venous infarcts and possible neurologically sequelae.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ascher E, Salles-Cunha S, Hingorani A. Morbidity and mortality associated with internal jugular vein thromboses. Vasc Endovascular Surg. 2005. 39: 335-9
2. Ball E, Morris-Stiff G, Coxon M, Lewis MH. Internal jugular vein thrombosis in a warfarinised patient: A case report. J Med Case Rep. 2007. 1: 184
3. Das S, Srinivasaraghavan R, Krishnamurthy S, Mahadevan S. Internal jugular vein thrombosis complicating disseminated tuberculosis in a 2-year-old child. BMJ Case Rep. 2014. 2014: bcr2014206861
4. Fiorot JA, Felício AC, Fukujima MM, Rodrigues CA, Morelli VM, Lourenço DM. Tuberculosis: An uncommon cause of cerebral venous thrombosis?. Arq Neuropsiquiatr. 2005. 63: 852-4
5. Gbaguidi X, Janvresse A, Benichou J, Cailleux N, Levesque H, Marie I. Internal jugular vein thrombosis: Outcome and risk factors. QJM. 2011. 104: 209-19
6. Gowrinath K, Nizamiz MI, Kumar BE, Suneetha P, Kishor VH. Unusual complication of cervical tuberculous lymphadenopathy. Indian J Tuberc. 2011. 58: 35-7
7. Hingorani A, Ascher E, Markevich N, Yorkovich W, Schutzer R, Mutyala M. Risk factors for mortality in patients with upper extremity and internal jugular deep venous thrombosis. J Vasc Surg. 2005. 41: 476-8
8. Naithani R, Agrawal N, Choudhary VP. Deep venous thrombosis associated with tuberculosis. Blood Coagul Fibrinolysis. 2007. 18: 377-80
9. Seligsohn U, Lubetsky A. Genetic susceptibility to venous thrombosis. N Engl J Med. 2001. 344: 1222-31