- Department of Neurosurgery, Asahikawa Red Cross Hospital, Asahikawa, Hokkaido, Japan.
DOI:10.25259/SNI_693_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Koki Onodera, Kota Kurisu, Seiji Takebayashi, Juro Sakurai, Tohru Kobayashi, Rina Kobayashi, Shuho Goto, Katsumi Takizawa. Intracranial plasmacytoma arising from dura mater secondary to multiple myeloma and presenting with sudden lethal intracerebral hemorrhage: A case report and literature review. 17-Feb-2021;12:55
How to cite this URL: Koki Onodera, Kota Kurisu, Seiji Takebayashi, Juro Sakurai, Tohru Kobayashi, Rina Kobayashi, Shuho Goto, Katsumi Takizawa. Intracranial plasmacytoma arising from dura mater secondary to multiple myeloma and presenting with sudden lethal intracerebral hemorrhage: A case report and literature review. 17-Feb-2021;12:55. Available from: https://surgicalneurologyint.com/surgicalint-articles/10598/
Abstract
Background: Intracranial and central nervous system’s involvement with multiple myeloma (MM) is a clinically rare manifestation. Furthermore, the development of intracranial plasmacytoma without bone involvement is much rarer. Herein, we report the case of massive intracerebral hemorrhage form intracranial plasmacytoma that arose from the dura mater without bone involvement.
Case Description: A 71-year-old woman, who had been diagnosed as MM and treated 2 years prior, developed sudden lethal intracerebral hemorrhage from the intracranial plasmacytoma. Massive hemorrhage was observed after a rapid tumor growth in the middle fossa. Immediate hematoma evacuation and tumor resection allowed the patient to avoid severe neurological deficits and lethal conditions.
Conclusion: A close follow-up by neuroimaging studies is essential in cases of intracranial plasmacytoma in MM patients and early intervention with surgical resection or radiotherapy should be considered.
Keywords: Intracerebral hemorrhage, Intracranial plasmacytoma, Multimodality, Multiple myeloma
INTRODUCTION
Intracranial and central nervous system involvement with multiple myeloma (MM) is a rare clinical presentation, affecting <1% of patients with MM.[
Intracranial involvement without any bone involvement associated with MM is extremely rare.[
Urgent surgical hematoma evacuation and tumor resection allowed the patient to avoid severe neurological deficits and lethal condition. This rare disease manifestation in MM patients is significant and highlights the importance of optimal management of MM with intracranial involvement.
CASE REPORT
A 69-year-old woman was diagnosed with immunoglobulin (Ig) A lambda-type MM and was treated with 8 cycles of chemotherapy bortezomib-dexamethasone (VD) and lenalidomide-bortezomib-dexamethasone (RVD lite) as well as autologous peripheral stem cell transplantation. She underwent complete remission (CR). After 15 months, she presented with neck pain and paralysis in her left arm. Spinal magnetic resonance imaging (MRI) showed extramedullary infiltration in the left C4 and C5 spinous processes and multiple lytic lesions in the upper thoracic vertebra, indicating a recurrence of MM. Systemic treatment was started with daratumumab, bortezomib, and dexamethasone (D-Vd) and focal irradiation (30 Gy/10 Fr) for spinal lesions. During this time, brain MRI was used to screen for intracranial lesions.
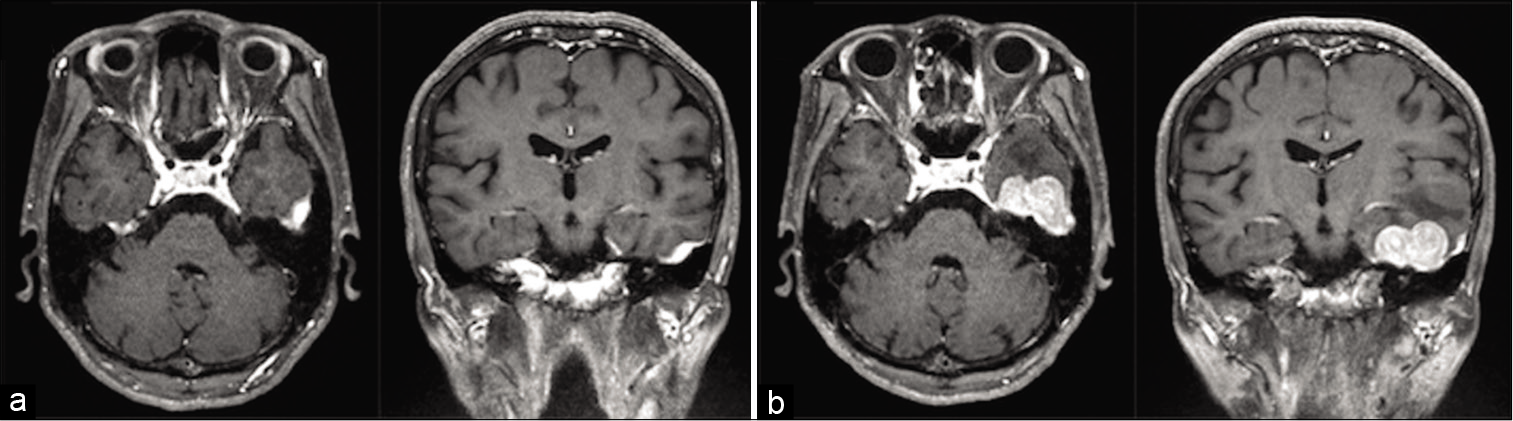
Brain MRI with contrast medium [
Figure 1:
Axial and coronal contrasted T1-weighted magnetic resonance (MR) imaging. (a) MR imaging 3 months before the onset of intracerebral hemorrhage revealed a thickened dural lesion in the left temporal region with homogenous contrast enhancement. No abnormal findings in the contiguous skull base were observed (b) MR imaging 1 week before the onset showed that the extra-axial lesion expanded to 33 × 33 mm mass.
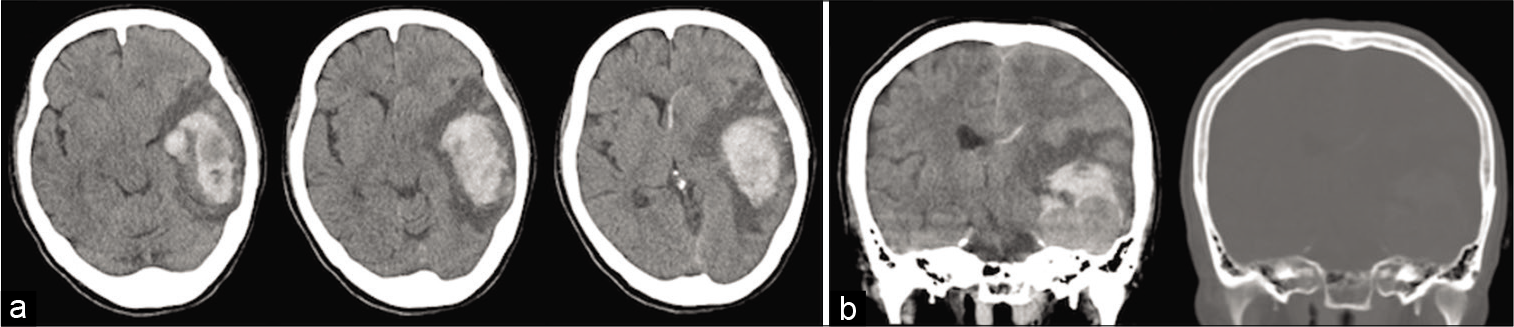
However, a week after MRI, she developed an acute onset of headache followed by disturbance of consciousness and right-sided hemiparesis. She was brought to the emergency room by ambulance. On arrival, she was unable to follow commands and exhibited aphasia and right-handed hemiparesis. A computed tomography (CT) scan [
Figure 2:
Preoperative axial and coronal noncontrasted computed tomographic (CT) scan demonstrating a mass in the left temporal lobe is associated with intraparenchymal hemorrhage extending posteriorly and superiorly. (a) Axial CT images showing a significant mass effect, including the displacement of the left ventricle and midline shift (b) Coronal CT images indicated that the tumor had no adjacent bony lesions.
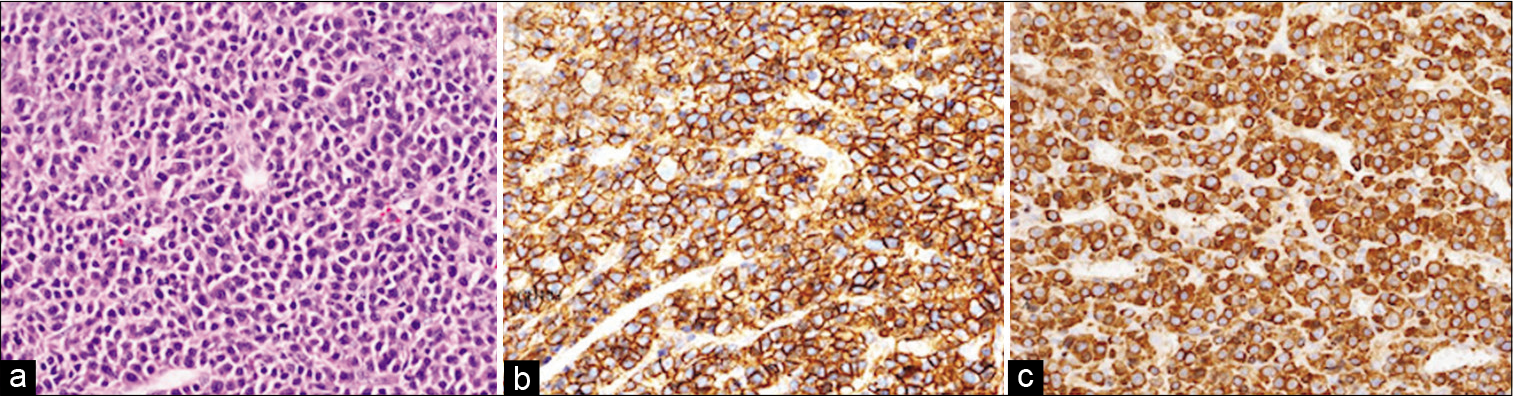
An urgent operation for both the hematoma evacuation and tumor resection was performed. After a temporal craniotomy and dural incision, the intraparenchymal hematoma was promptly evacuated. A reddish rather soft mass was observed directly connected to the hematoma, which arose from the dura mater of the middle fossa. The tumor was detached from the dura mater of the middle fossa followed by gross total removal of the tumor. Since there were no tumor invasion and no connection between the outer layer of the dura mater and adjacent sphenoid bone in the middle fossa, these structures were intentionally preserved. Finally, duroplasty was performed, the bone flap was returned, and the skin was normally closed. The resected tumor was sent for a histological examination. Hematoxylin-eosin staining [
Figure 3:
Histopathological and immunohistochemical examinations of the surgical specimen (a) A histopathologic study with hematoxylin-eosin staining shows diffuse proliferation of plasmacytoid cells, with clumped nuclear chromatin and eccentric cytoplasm (b) Immunohistochemical examination demonstrating the immunostaining of CD138, a marker of plasma cells, indicating the proliferation of CD138-positive cells (c) Immunohistochemical examination revealed that the plasma cells were monoclonal staining with lambda.
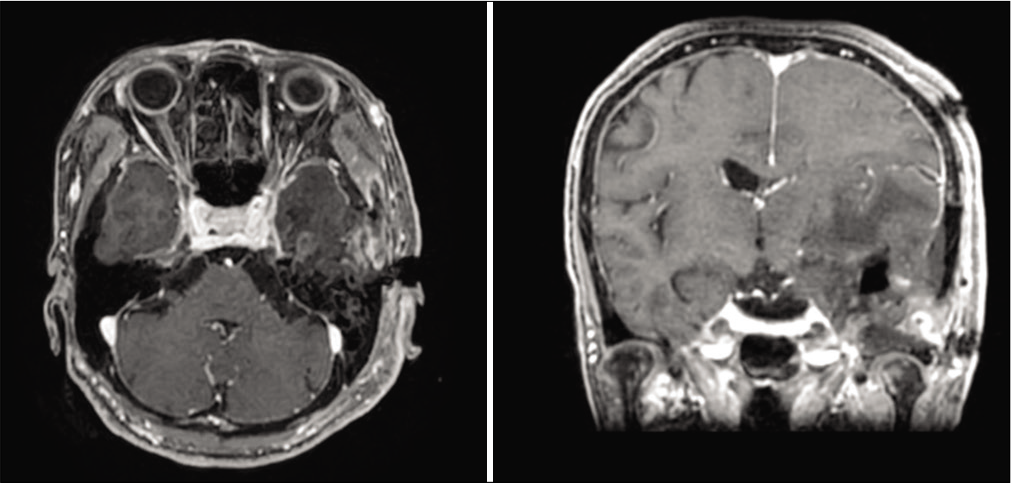
The postoperative course was uneventful and her hemiparesis and aphasia resolved immediately. Postoperative MRI [
DISCUSSION
We here report a case of intracranial MM arising from the dura mater without bone involvement. This rare intracranial mass exhibited rapid growth in a few months, followed by a lethal intracranial hemorrhage from the tumor itself. The urgent operation, hematoma evacuation, and tumor removal allowed the patient to recover from a severe neurological sequela.
Among the intracranial involvement in patients with MM, dural involvement usually occurs due to the direct extension of a plasmacytoma of the skull.[
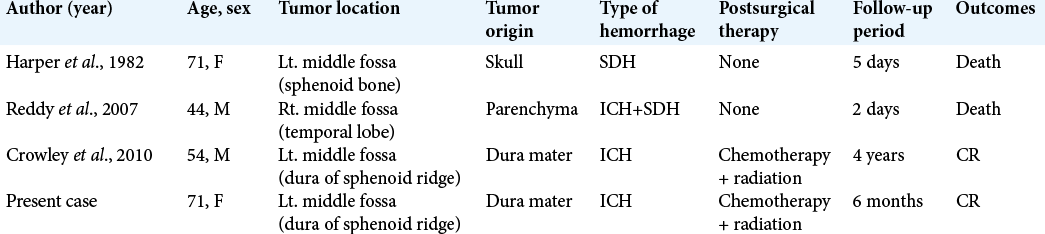
Hemorrhage from intracranial plasmacytoma is a rare and severe presentation. There have only been a few case reports, as summarized in [
The involvement of the central nervous system in MM is lethal, with a survival time of 6 months.[
CONCLUSION
There is currently no established treatment for intracranial MM. At present, tailored combined therapy with chemotherapy, radiotherapy, and surgical resection is chosen as appropriate for each patient. In our case, intracranial plasmacytoma secondary to MM grew rapidly, resulting in severe intracerebral hemorrhage. Since the hemorrhagic manifestation of intracranial plasmacytoma tends to lead to poor prognosis, it is important to recognize the possibility of hemorrhage from tumor in actual clinical settings, as shown in the presented case. Close follow-up by neuroimaging studies and early intervention with surgical resection or radiotherapy is recommended in such case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cerase A, Tarantino A, Gozzetti A, Muccio CF, Gennari P, Monti L. Intracranial involvement in plasmacytomas and multiple myeloma: A pictorial essay. Neuroradiology. 2008. 50: 665-74
2. Chen CI, Masih-Khan E, Jiang H, Rabea A, CsertiGazdewich C, Jimenez-Zepeda VH. Central nervous system involvement with multiple myeloma: Long term survival can be achieved with radiation, intrathecal chemotherapy, and immunomodulatory agents. Br J Haematol. 2013. 162: 483-8
3. Crowley RW, Sansur CA, Sheehan JP, Mandell JW, Kassell NF, Dumont AS. Intracranial plasmacytoma with apoplectic presentation and spontaneous intracerebral hemorrhage: Case report and review of the literature. Clin Neurol Neurosurg. 2010. 112: 172-5
4. Daghighi MH, Poureisa M, Shimia M, Mazaheri-Khamene R, Daghighi S. Extramedullary plasmacytoma presenting as a solitary mass in the intracranial posterior fossa. Iran J Radiol. 2012. 9: 223-6
5. Gangatharan SA, Carney DA, Prince HM, Wolf MM, Januszewicz EH, Ritchie DS. Emergence of central nervous system myeloma in the era of novel agents. Hematol Oncol. 2012. 30: 170-4
6. Harper L, LeBlanc HJ, McDowell JR. Intracranial extension and spontaneous hemorrhage of a sphenoid plasmacytoma. Neurosurgery. 1982. 11: 797-9
7. Lasocki A, Gangatharan S, Gaillard F, Harrison SJ. Intracranial involvement by multiple myeloma. Clin Radiol. 2015. 70: 890-7
8. Lee D, Kalff A, Low M, Gangatharan S, Ho P, Bajel A. Central nervous system multiple myeloma-potential roles for intrathecal therapy and measurement of cerebrospinal fluid light chains. Br J Haematol. 2013. 162: 371-5
9. Liu S, Li X, Li Y, Li D, Wang Y, Tian C. Multiple myeloma with dural mater involvement. Onco Targets Ther. 2019. 12: 3373-5
10. Ma XJ, Li D, Wang L, Hao SY, Zhang LW, Zhang JT. Clinical features, radiological profiles, and surgical outcomes of primary intracranial solitary plasmacytomas: A report of 17 cases and a pooled analysis of individual patient data. J Neurooncol. 2019. 142: 263-72
11. More S, Petrucci MT, Corvatta L, Fazio F, Offidani M, Olivieri A. Monoclonal antibodies: Leading actors in the relapsed/refractory multiple myeloma treatment. Pharmaceuticals (Basel). 2020. 13: E426
12. Prakash A, Korem S, Inkollu S, Lee P. Multiple myeloma relapse as intracranial plasmacytoma: A rare presentation. Cureus. 2020. 12: e8357
13. Reddy N, Karampelas I, Chanan-Khan A, Fenstermaker R, Padmanabhan S. Aggressive relapse of multiple myeloma with intracerebral extension and associated hemorrhage. Leuk Lymphoma. 2007. 48: 1228-30
14. Schwartz TH, Rhiew R, Isaacson SR, Orazi A, Bruce JN. Association between intracranial plasmacytoma and multiple myeloma: Clinicopathological outcome study. Neurosurgery. 2001. 49: 1039-44
15. Silverstein A, Doniger DE. Neurologic complications of myelomatosis. Arch Neurol. 1963. 9: 534-44