- Departments of Neurosurgery, Northeast National Medical Center, Monterrey, Nuevo Leon, Mexico,
- Department of Neurosurgery, Indiana University School of Medicine, Indianapolis, Indiana, United States.
- Anatomic Pathology and Clinical Pathology, Northeast National Medical Center, Monterrey, Nuevo Leon, Mexico,
Correspondence Address:
Jose Javier Cuellar Hernandez
Departments of Neurosurgery, Northeast National Medical Center, Monterrey, Nuevo Leon, Mexico,
DOI:10.25259/SNI_417_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jose Javier Cuellar Hernandez1, Miracle Anokwute2, Silvia Judith Hernandez Martinez3, Jose Ramon Olivas1. Intradural iatrogenic epidermoid cyst at cauda equina: A case report. 18-Sep-2020;11:299
How to cite this URL: Jose Javier Cuellar Hernandez1, Miracle Anokwute2, Silvia Judith Hernandez Martinez3, Jose Ramon Olivas1. Intradural iatrogenic epidermoid cyst at cauda equina: A case report. 18-Sep-2020;11:299. Available from: https://surgicalneurologyint.com/surgicalint-articles/10263/
Abstract
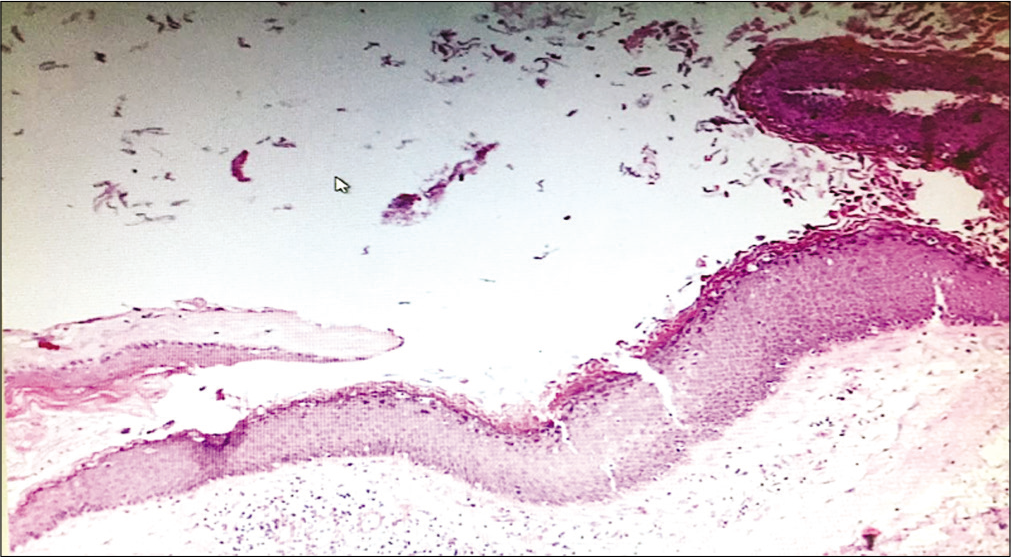
Background: Spinal epidermoid accounts for
Case Description: A 38-year-old female with a history of epidural spinal blocks at L2-3 for two previous pregnancies presented with low back pain, right lower extremity weakness (4/5 level), hyporeflexia, and tingling/ numbness in the right L3-5 distribution. The lumbar MR demonstrated an intradural extramedullary lesion at the L2-L3 level that compressed the cauda equina/nerve roots. MR findings were compatible with an epidermoid cyst, this was histologically confirmed following a microsurgical L2-3 laminectomy for lesion resection. Pathologically, the lesion demonstrated a keratinized stratified squamous epithelium with keratin content without cutaneous attachments, thus confirming the diagnosis of an epidermoid cyst. Postoperatively, her sensory complains improved and her motor strength fully recovered to the 5/5 level.
Conclusion: Patients with spinal epidermoid cysts typically present with underlying spinal dysraphism, but only rarely do iatrogenic cases arise. Here, we presented a patient who developed a spinal lumbar epidermoid cyst in a female patient after undergoing spinal epidural anesthesia during pregnancy. Notably, this was successfully treated a with decompressive laminectomy and microsurgical resection.
Keywords: Cauda equina, Epidermoid cyst, Iatrogenic, Laminotomy, Lumbar puncture
INTRODUCTION
Congenital (e.g., associated with spinal dysraphism) or iatrogenic epidermoid cysts (i.e., also called “pearl tumors”) represent approximately 0.5–1% of all intraspinal tumors.[
During the embryonic period, these lesions “grow” secondary to progressive invagination of epidermal elements into the neural tube.[
The clinical symptoms/signs of these lesions reflect their location. Here, we present a 38-year-old female who developed an epidermoid cyst following two epidural anesthetics utilized for childbirth.
CASE PRESENTATION
A 38-year-old female with a surgical history of two cesarean sections performed with L2-L3 epidural spinal anesthesia presented with 6 months of increasing low back pain and right lower extremity L2-L4 paresthesias/tingling. For several years, she had tried various medications without improvement. She denied any history of trauma, infectious diseases, or surgeries related to her spine.
On physical examination, she had right iliopsoas, quadriceps, dorsiflexion, and plantar flexor weakness (4/5 level), diffuse hyporeflexia, and decreased pin/touch appreciation in the L3-L5 dermatomes. There was no evidence of underlying spinal dysraphism (sacral dimple, tuft of hair, or dermal sinus tract).
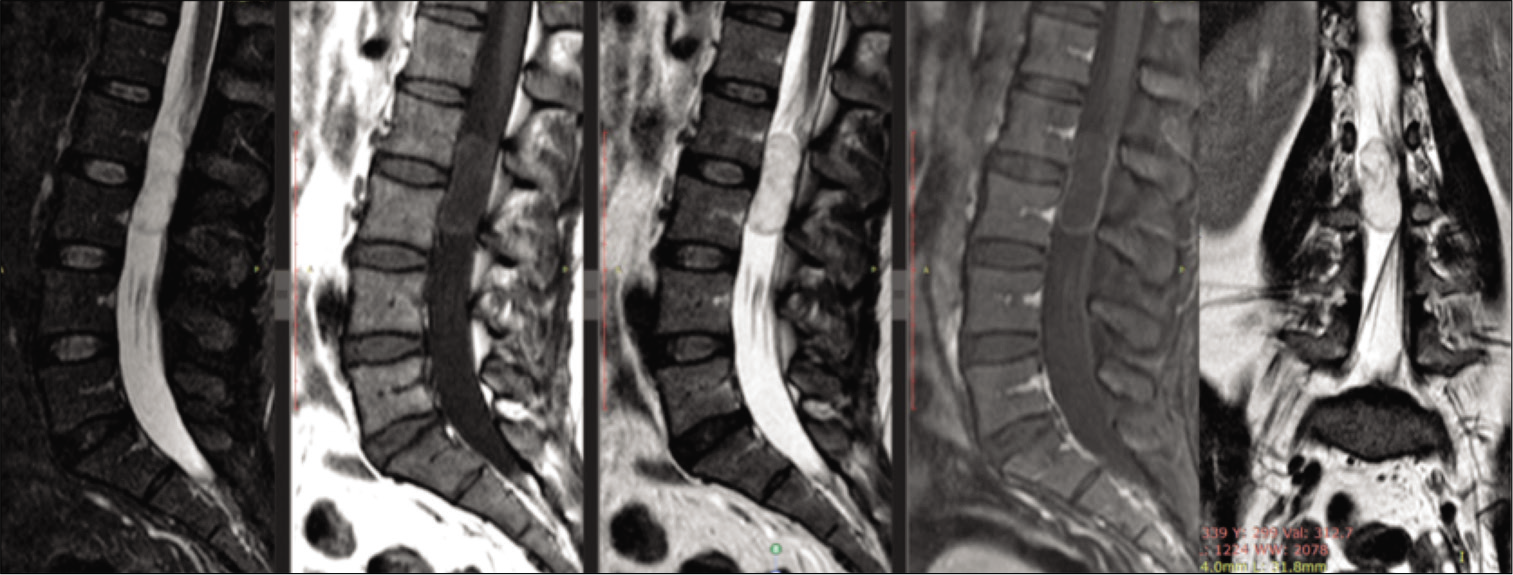
The magnetic resonance imaging of the lumbosacral spine with and without contrast demonstrated a well-circumscribed intradural, extramedullary lesion at the L2-L3 level m (i.e., 3.76 × 1.25 × 1.56 cm) that was slightly hyperintense on T1, hyperintense on the T2 sequence, weighted images, with peripheral enhancement on the contrast study. All findings were consistent with an epidermoid cyst resulting in displacement right to left of the conus/cauda equina [
Figure 1:
Noncontrasted and contrasted preoperative sagittal and coronal magnetic resonance imaging of the lumbar spine demonstrating well-circumscribed intradural, extramedullary lesion at the L2 and L3 level, measuring 3.76 × 1.25 × 1.56 cm, from the right to left that is hyperintense on T2 and STIR but isointense on T1 but with peripheral enhancement on T1 postcontrast. Note the displacement from the right to left the cauda equine nerve roots.
Surgery
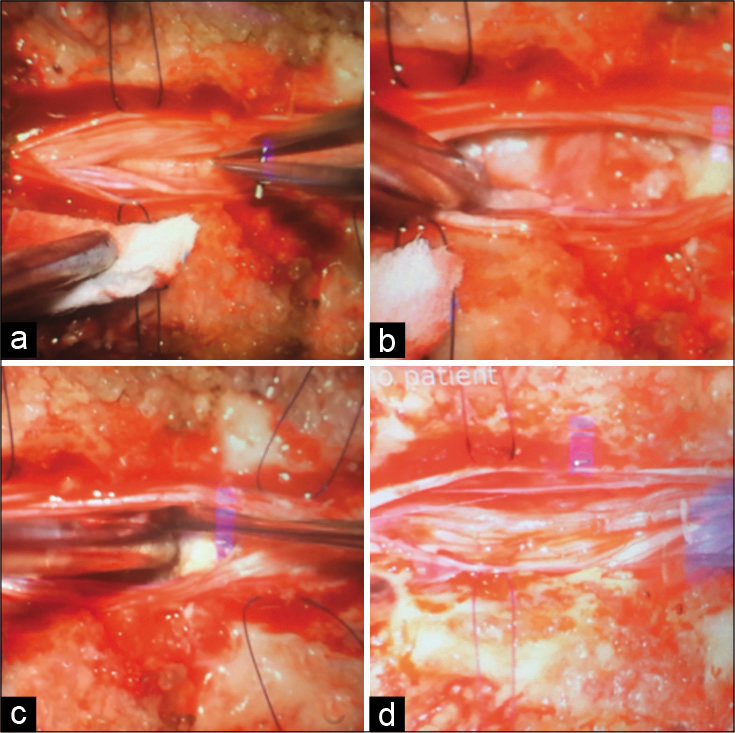
The patient underwent a L2 laminectomy for resection of the epidermoid cyst. This was performed utilizing microscopic visualization, and required a midline durotomy. The lesion was nonvascularized, grayish, pearly, and friable with a well-defined capsule that was not adherent to the surrounding nerve roots of the cauda equina (i.e., more right sided) which was fully resected [
Figure 2:
Microsurgical resection of epidermoid cyst (a) dural opening with displaced nerve roots and capsule of the tumor, (b) approach of the capsular portion and initiation of the debulking, (c) lesion with friable content, poorly vascularized with multiple adhesions to adjacent nerve roots, (d) total resection of the lesion without compromising nerve roots.
DISCUSSION
Congenital (i.e., with spinal dysraphism) and iatrogenic intraspinal epidermoid cysts are quite rare, especially in the lumbar spine.[
Surgery and recurrence rates
Surgical treatment, including gross total excision, is the treatment of choice for patients with persistent/significant neurological deficits.[
Although the epidermoid cysts are benign tumors, local recurrence (reported in up to 10–29% of cases) is reported, especially after subtotal excision because the incomplete excision of basal germinal cells.[
Although recurrent epidermoid cysts develop from 2 to 23 years after the apparent moment of implantation, in our case, the lumbar puncture occurred 9 and 13 years ago.[
CONCLUSION
Spinal epidermoid cyst accounts for <1% of all primary spinal cord tumors. Once identified on MR studies, gross total resection typically results in resolution of prior neurological deficits.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Choremis C, Economos D, Gargoulas A, Papadatos C. Intraspinal epidermoid tumours (cholesteatomas) in patients treated for tuberculous meningitis. Lancet. 1956. 271: 437-9
2. Funao H, Isogai N, Daimon K, Mima Y, Sugiura H, Koyanagi T. A rare case of intradural and extramedullary epidermoid cyst after repetitive epidural anesthesia: Case report and review of the literature. World J Surg Oncol. 2017. 15: 131
3. Gibson T, Norris W. Skin fragments removed by injection needles. Lancet. 1958. 272: 983-5
4. Manno NJ, Uihlein A, Kernohan JW. Intraspinal epidermoids. J Neurosurg. 1962. 19: 754-65
5. Morita M, Miyauchi A, Okuda S, Oda T, Aono H, Iwasaki M. Intraspinal epidermoid tumor of the cauda equina region: Seven cases and a review of the literature. J Spinal Disord Tech. 2012. 25: 292-8
6. Park MH, Cho TG, Moon JG, Kim CH, Lee HK. Iatrogenic intraspinal epidermoid cyst. Korean J Spine. 2014. 11: 195-7
7. Penisson-Besnier I, Guy G, Gandon Y. Intramedullary epidermoid cyst evaluated by computed tomographic scan and magnetic resonance imaging: Case report. Neurosurgery. 1989. 25: 955-9
8. Shin MW, Lee JH, Cho WH, Kim JH. Intradural epidermoid cyst at conus medullaris and cauda equina of the spine. J Korean Soc Radiol. 2012. 66: 113-6
9. Yin H, Zhang D, Wu Z, Zhou W, Xiao J. Surgery and outcomes of six patients with intradural epidermoid cysts in the lumbar spine. World J Surg Oncol. 2014. 12: 50
10. Ziv ET, Gordon McComb J, Krieger MD, Skaggs DL. Iatrogenic intraspinal epidermoid tumor: Two cases and a review of the literature. Spine (Phila Pa 1976). 2004. 29: 15-8