- Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Jazan University, Jazan, Saudi Arabia,
- Division of Neurosurgery, Department of Surgery, University of Alberta, Edmonton, Canada.
DOI:10.25259/SNI_355_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yahya H. Khormi, Ryan Chrenek, Tejas Sankar. Intradural synovial cyst of the upper cervical spine: A rare cause of symptomatic cord compression. 11-Jul-2020;11:190
How to cite this URL: Yahya H. Khormi, Ryan Chrenek, Tejas Sankar. Intradural synovial cyst of the upper cervical spine: A rare cause of symptomatic cord compression. 11-Jul-2020;11:190. Available from: https://surgicalneurologyint.com/surgicalint-articles/10132/
Abstract
Background: Synovial cysts are commonly observed soft-tissue masses of the spine, typically extradural and located in the lumbar region. We describe a very rare symptomatic case of a C1-C2 intradural synovial cyst.
Case Description: A 78-year-old female presented with progressive left side weakness, paresthesia, and hyperreflexia. The magnetic resonance imaging revealed a well-circumscribed, subtly enhancing lesion medial to the C1-2 facet, causing cord compression and edema. Using neurophysiological monitoring, surgery included a modified laminectomy of C2 with the removal of the C1 posterior arch. When the dura was opened, a sizable intradural extramedullary lesion was encountered, the cyst was successfully drained and partially resected. The histopathological diagnosis was consistent with a synovial cyst. Postoperatively, the patient’s strength on the left side improved gradually until she was fully ambulatory. Postoperative imaging showed no recurrence at 8 months follow-up.
Conclusion: Synovial cysts should be considered among the differential diagnose of C1-2 cysts. They can occur intradurally and compress the spinal cord resulting in a significant neurological deficit. Cyst excision may be accomplished utilizing a limited laminectomy for cyst identification and drainage, accompanied by partial resection of the cyst wall. Such intervention can lead to good clinical outcomes.
Keywords: Atlantoaxial joint, Cervical cord compression, Intradural cystic lesion, Synovial cyst
BACKGROUND
Juxtafacet cysts are soft-tissue masses that arise from joints in the spine. They include synovial cysts – true cysts with a synovial lining – versus ganglion cysts which are actually pseudocystic histologically.[
CASE DESCRIPTION
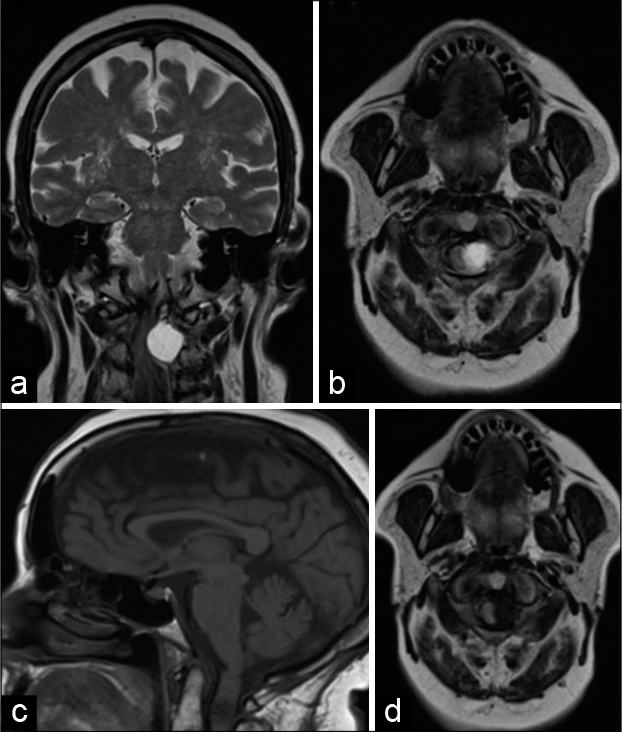
A 78-year-old female presented with the left-sided weakness, paresthesia, and hyperreflexia. The preoperative magnetic resonance imaging (MRI) revealed a well-circumscribed, homogenous, and subtly enhancing dorsolateral intradural lesion with diminished T1 signal and increased T2 signal. It arose from the region of the transverse ligament of the atlas and measuring 1.9 cm × 1.6 cm × 1.9 cm, where it contributed to dorsolateral cord compression. In addition, there was a subtle abnormal T2 increased signal within the cord reflecting edematous change at this level [
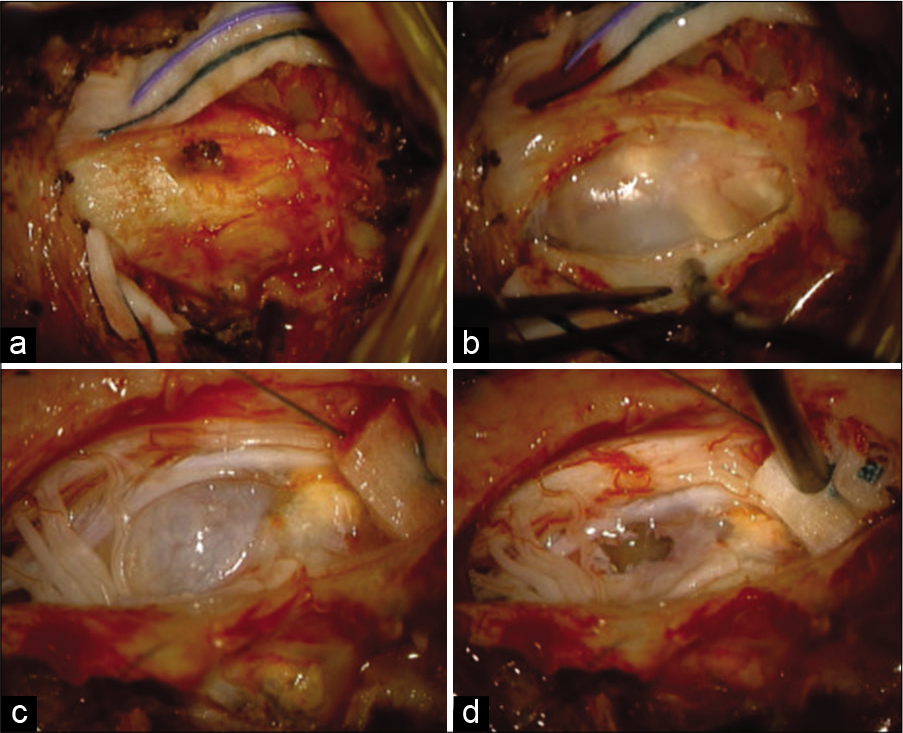
Utilizing intraoperative monitoring, the patient underwent a three-quarter laminectomy of C2, with complete removal of the left hemilamina, half of the right hemilamina, and the posterior arch of C1. Following the decompression, it was noted that the lateral aspect of the thecal sac and the exiting C2 nerve root was slightly thinned, but there was no extradural cyst.
When the dura was opened in a C-shaped fashion deep to several rootlets of the spinal accessory nerve, a sizable intradural extramedullary lesion pushing the spinal cord toward the right was evident. There was a plane between the spinal cord and the cystic lesion facilitating operative dissection. The wall of the cyst was opened and there was efflux of clear fluid with a small amount of calcified material [
Pathology
The analysis included periodic acid–Schiff and Gomori trichrome special stains as well as immunohistochemical markers including AE1/AE3, MIB-1, cluster of differentiation 68, and epithelial membrane antigen. The cyst was partially lined with meningothelial cells; these findings were consistent with a synovial cyst.
Discharge and postoperative course
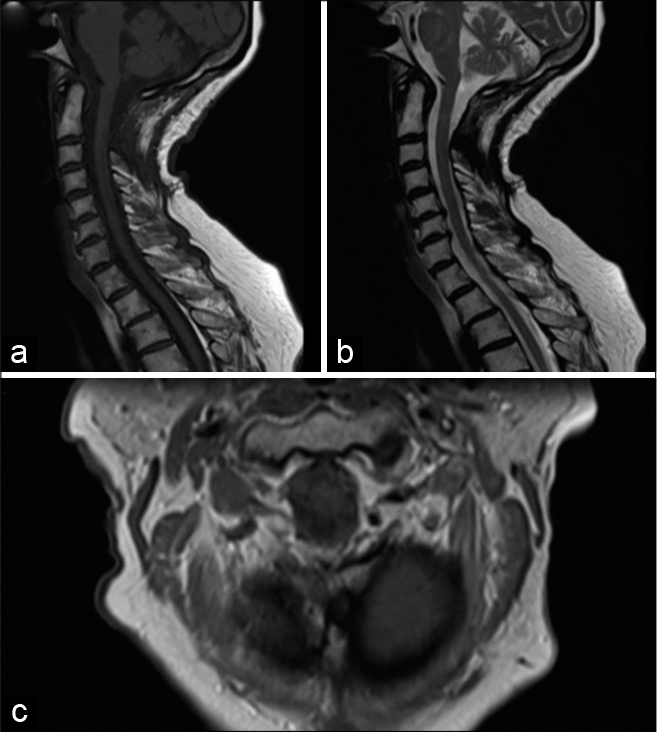
At the time of discharge 4 days later, the patient’s left-sided strength was significantly improved compared to preoperatively. At a 1-month, she was ambulating independently. Postoperative imaging 8 months later (MR) showed no significant residual cyst nor spinal cord compression [
DISCUSSION
There are three case reports of the cervical extradural synovial cyst with small extension intradural.[
The diagnosis of initial MRI was uncertain; however, a ganglion or synovial cyst was considered a possibility. A cystic schwannoma or meningioma was also included in the differential diagnosis.
The age of this patient is in keeping with previously reported cases, which typically occur in those 60 years of age and older.[
CONCLUSION
Synovial cysts should be considered in the differential diagnosis of C1-2 cystic pathology causing spinal cord compression and neurological deficit. Limited laminectomy without fusion, drainage of intradural cyst, and partial resection of the wall can improve neurological function with minimal neurological risk.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akiyama H, Tamaki N, Kondoh T, Nagashima T. Craniocervical junction synovial cyst associated with atlanto-axial dislocation-case report. Neurol Med Chir (Tokyo). 1999. 39: 539-43
2. Boviatsis EJ, Stavrinou LC, Kouyialis AT, Gavra MM, Stavrinou PC, Themistokleous M. Spinal synovial cysts: Pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J. 2008. 17: 831-7
3. Christophis P, Asamoto S, Kuchelmeister K, Schachenmayr W. Juxtafacet cysts, a misleading name for cystic formations of mobile spine (CYFMOS). Eur Spine J. 2007. 16: 1499-505
4. Hartmann S, Tschugg A, Kavakebi P, Thome C. Intradural synovial cyst of the atlantoaxial joint: A case report. Acta Neurochir (Wien). 2016. 158: 1583-6
5. Iwakoshi HY, Niwa M. Two cases of upper cervical intraspinal juxta-facet cysts. Spinal Surg. 2004. 18: 197-202
6. Khan AM, Synnot K, Cammisa FP, Girardi FP. Lumbar synovial cysts of the spine: An evaluation of surgical outcome. J Spinal Disord Tech. 2005. 18: 127-31
7. Morio Y, Yoshioka T, Nagashima H, Hagino H, Teshima R. Intraspinal synovial cyst communicating with the C1-C2 facet joints and subarachnoid space associated with rheumatoid atlantoaxial instability. Spine (Phila Pa 1976). 2003. 28: E492-5