- Department of Neurosurgery, SCB Medical College Hospital, Cuttack, Odisha, India
Correspondence Address:
Soubhagya R. Tripathy
Department of Neurosurgery, SCB Medical College Hospital, Cuttack, Odisha, India
DOI:10.4103/2152-7806.182544
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tripathy SR, Deo RC, Mishra S, Dhir MK, Nath PC, Satapathy MC. Intramedullary spinal cord metastasis arising from papillary thyroid carcinoma: A case report and review of literature. Surg Neurol Int 17-May-2016;7:
How to cite this URL: Tripathy SR, Deo RC, Mishra S, Dhir MK, Nath PC, Satapathy MC. Intramedullary spinal cord metastasis arising from papillary thyroid carcinoma: A case report and review of literature. Surg Neurol Int 17-May-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/intramedullary-spinal-cord-metastasis-arising-from-papillary-thyroid-carcinoma-a-case-report-and-review-of-literature/
Abstract
Background:Intramedullary spinal cord metastases (IMSCM) are typically drop lesions from intracranial metastases and are a rare manifestation of systemic malignancy (8.5% of central nervous system metastases). They arise from primaries such as the lungs, breast, kidney, melanoma, or lymphoma. On the other hand, they arise very rarely from papillary thyroid carcinoma (PTC), even though it is the most common type of primary thyroid malignancy.
Case Description:A 54-year-old male presented with pain in the lower back along with tingling, numbness, and weakness in the bilateral lower limbs. This was associated with urine incontinence for 1½ months. In the previous month, he developed a left-sided solitary thyroid nodule. Fine needle aspiration cytology and ultrasonography were suggestive of metastasis. Furthermore, the thoracolumbar magnetic resonance imaging showed T1-hypo and T2-hyper-intense D11-D12 level intramedullary lesion, with intense enhancement, which was consistent with an intramedullary lesion involving the conus. At surgery, a firm, brownish yellow, friable, vascular tumour was removed en toto. Upon discharge, the patient was neurologically intact except for residual bladder incontinence.
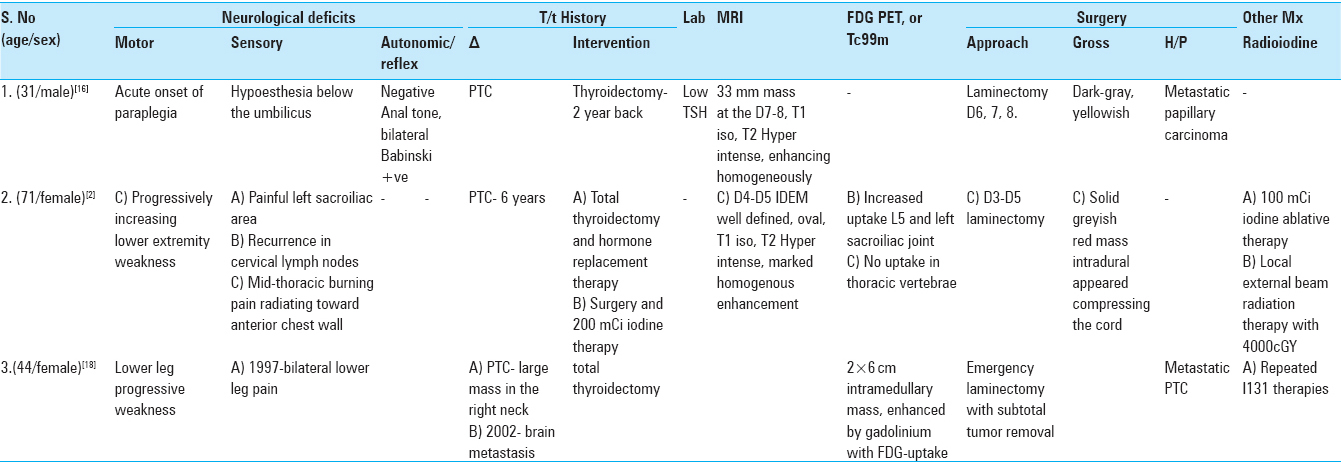
Conclusion:In an extensive literature review (pubmed), IMSCM metastasis from PTC primary is confirmed as a rarity and this may be the fourth documented case. Moreover, this may be the first report of a case of PTC metastatic neurological deterioration “even before the treatment of the primary was undertaken.” Early diagnosis and microsurgical resection can result in improvement of neurological deficits and in the quality of life of patients with IMSCM.
Keywords: Intramedullary spinal cord metastasis, laminectomy, papillary thyroid carcinoma, spinal metastasis, thyroid cancer
INTRODUCTION
Intramedullary spinal cord metastases (IMSCM) represent 8.5% of central nervous system (CNS) metastases. IMSCM affects 0.1–0.4% of all carcinoma patients and comprise 1–3% of all intramedullary spinal cord neoplasms.[
CASE REPORT
A 54-year-old male presented with bilateral low back pain, tingling, numbness, and weakness in both the lower limbs, and incontinence of the bowel and bladder of 2-months duration [
On examination, he had a solitary left-sided thyroid nodule (2 × 2 cm). Motor strength in the lower extremities was 4-/5 on the left and 4/5 on the right (Medical Research Council scale). There was a 20% diminution of all sensation below L1 dermatome and 40% below L3. Perianal sensation was diminished. Plantar reflex was extensor on the left and flexor on the right side.
MR studies
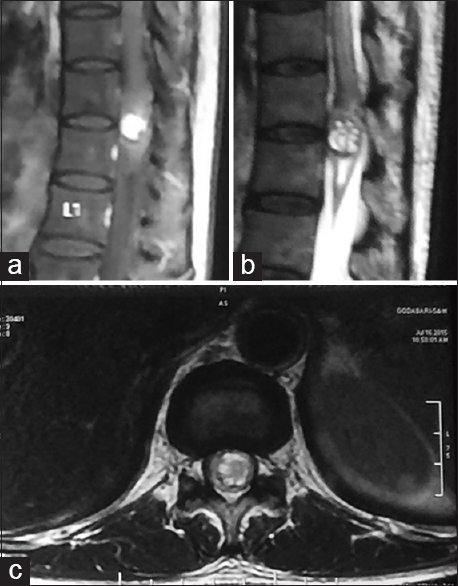
At the D11-12 level, magnetic resonance imaging (MRI) showed an expanded cord with an intramedullary lesion (13 × 11 × 8 mm); the T1 image was hypointense and the T2 study showed it was hyperintense with intense enhancement [
Figure 2
The MRI scan of the thoracic spinal cord: Sagittal (a) T1-weighted contrast image, sagittal (b) T2-weighted image, axial (c) T1-weighted contrast image and axial: Showing a solitary mass in the intramedullary spinal cord at D11-12 level. The lesion showed a heterogeneous enhancement following intravenous gadolinium contrast
Surgical intervention
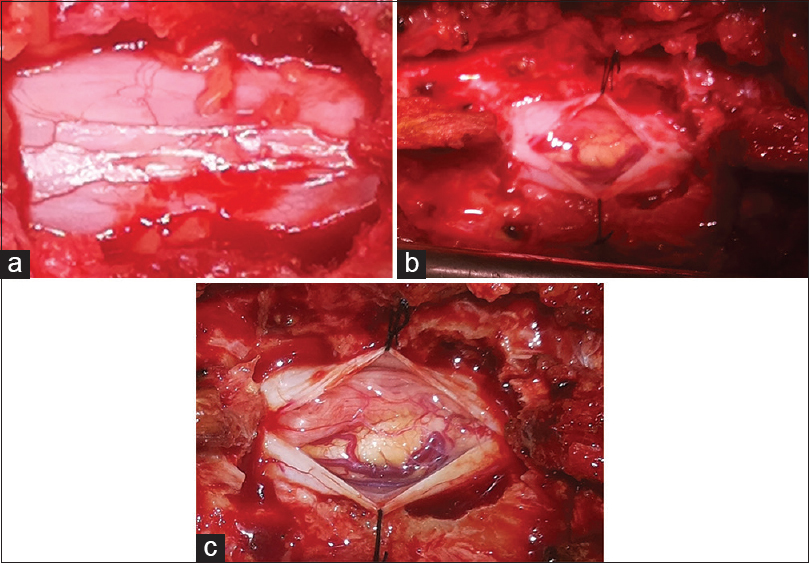
A midline vertical incision was made along the D10-L1 spinous process. D11, D12 laminectomy was performed revealing a tense bluish, intradural mass within the dura in the conus region [
Postoperative neurological status
On postoperative day 3, the patient could walk with minimal support, and could resume his daily activities within a week. However, his bladder incontinence persisted, requiring a perurethral catheter in situ during discharge.
Pathology
H and E (hematoxylin and eosin) staining showed neoplastic tissue composed of sheaths of cells with ovaloid nuclei and without a cytoplasmic border; some had a ground glass appearance and nuclear grooves. In addition, there were many unevenly distributed psammoma bodies between the cells. Immunohistochemically, tumour cells were strongly positive for cytokeratin (CK), CK7, thyroid transcription factor 1 and negative for Novel Aspartic Proteinase of the PepSIN Family type A (NAPSIN-A) and CK20. Pathology confirmed metastatic lesion from PTC.
DISCUSSION
IMSCM are uncommon neoplastic lesions and account for 3–5% cases of myelopathy in patients affected by carcinoma.[
PTC is the most common type of thyroid tumour comprising between 30% and 70% of all thyroid carcinoma cases.[
Pathways for spread
Five routes have been hypothesised for the dissemination of metastatic intradural tumour originating from outside of the CNS: Haematogenous, via the arterial system, via the perineural lymphatics, through the venous plexus, spreading via subarachnoid space, and seeding from the involved osseous structure to the cerebrospinal fluid through the duramater.[
Clinical findings
Weakness and pain present early in comparison to sensory loss, with sphincter disturbance originating last.[
The occurrence of metastatic lesions with hemorrhage arising from a PTC are extremely rare.[
Spinal cord apoplexy
Spinal cord apoplexy is a hemorrhage occurring directly into the spinal cord. It may occur due to traumatism, changes in the coats of the blood vessels, or excessive blood pressure. When its occurrence is recent, it is red or dark in colour, which changes to brown or yellow with age; the tumour in our patient had yellowish-brown discoloration. The clot may later become encapsuled by a fibrous deposit.[
One report describes the case of a thoracic spinal cord lesion proven to be a metastasis from a thyroid primary (PTC).[
Investigations
Gadolinium-enhanced MRI is the imaging modality of choice for spinal tumours, including spinal metastases.[
Treatment
Providing patients with successful palliation and improving their quality of life demands multidisciplinary strategic treatment planning,[
High dose dexamethasone allows for limited and transient neurological improvement In combination with chemotherapy, radiation correlates with an increased duration of survival. Therapeutic irradiation and surgical decompression are the principal and complementary treatment options, respectively Cytoreductive surgery is a major treatment option for lesions early in the course of neurological deficits; however, it has not been found to increase the duration of survival compared to other treatment modalities. In young patients, both PTC and follicular thyroid cancer (FTC) have a more than 97% cure rate if treated appropriately. Indications of surgery include failure of irradiation therapy, unknown diagnosis, pathological fracture dislocation, and rapidly progressing paraplegia[ Postoperatively, most, but not all, patients with thyroid carcinoma need radioactive iodine treatment, except medullary thyroid cancer (MTC) and some small PTC.[
Prognosis
The best predictor of outcome is the site of primary tumour type, with the best prognosis noted in patients with breast or kidney cancer. Life expectancy is often relatively short with median survival ranging from 4 to 15 months in various series.[
CONCLUSION
Metastasis to spinal canal without the primary PTC manifesting itself is not common. In our extensive database search (Pubmed), this was confirmed to be the fourth such report of an IMSCM arising from a PTC. This may also stand out as the first report of a case of PTC metastatic neurological manifestation even before the treatment of the primary was undertaken. Early diagnosis and prompt microsurgical resection results in improvement of neurological deficits as well as the quality of life.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ain KB. Anaplastic thyroid carcinoma: Behavior, biology, and therapeutic approaches. Thyroid. 1998. 8: 715-26
2. AkhavanA , Mehrabaniyan MR, Jarahi M, Navabii H. Intradural extramedullary metastasis from papillary carcinoma of thyroid. BMJ Case Rep. 2012. p. Bcr0220125801-
3. Asadi M, Rokni-Yazdi H, Salehinia F, Allameh FS. Metastatic renal cell carcinoma initially presented with an intramedullary spinal cord lesion: A case report. Cases J. 2009. 2: 7805-
4. Babu M, Gupta R, Kumar A, Gupta M. Spinal intradural metastasis. Jk Science. 2004. 6: 48-50
5. Baudin E, Schlumberger M. New therapeutic approaches for metastatic thyroid carcinoma. Lancet Oncol. 2007. 8: 148-56
6. Bible KC, Suman VJ, Molina JR, Smallridge RC, Maples WJ, Menefee ME. Efficacy of pazopanib in progressive, radioiodine-refractory, metastatic differentiated thyroid cancers: Results of a phase 2 consortium study. Lancet Oncol. 2010. 11: 962-72
7. Cady B, Rossi R. An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery. 1988. 104: 947-53
8. Chamberlain MC, Tredway TL. Adult primary intradural spinal cord tumors: A review. Curr Neurol Neurosci Rep. 2011. 11: 320-8
9. Choi IJ, Chang JC, Kim DW, Choi G. A case report of “spinal cord apoplexy” elicited by metastatic intramedullary thyroid carcinoma. J Korean Neurosurg Soc. 2012. 51: 230-2
10. Costigan DA, Winkelman MD. Intramedullary spinal cord metastasis.A clinicopathological study of 13 cases. J Neurosurg. 1985. 62: 227-33
11. Dunne JW, Harper CG, Pamphlett R. Intramedullary spinal cord metastases: A clinical and pathological study of nine cases.Q J Med. 1986. 61: 1003-20
12. Frey I, Le Breton C, Lefkopoulos A, Perrot N, Khalil A, Chopier J. Intradural extramedullary spinalcanal secondary neoplasms: MR findings in 30 patients. Eur Radiol. 1998. 8: 1187-92
13. Gazzeri R, Galarza M, Faiola A, Gazzeri G. Pure intramedullary spinal cord metastasis secondary to gastric cancer. Neurosurg Rev. 2006. 29: 173-7
14. Goolden AW, Mclaughlin JE, Valentine AR, Pease C. Solitary cerebral metastasis from a papillary carcinoma of the thyroid. Postgrad Med J. 1990. 66: 127-9
15. Grasso G, Meli F, Patti R, Giambartino F, Florena AM, Iacopino DG. Intramedullary spinal cord tumor presenting as the initial manifestation of metastatic colon cancer: Case report and review of the literature. Spinal Cord. 2007. 45: 793-6
16. Honma Y, Kawakita K, Nagao S. Intramedullary spinal cord and brain metastases from thyroid carcinoma detected 11 years after initial diagnosis-case report. Neurol Med Chir (Tokyo). 1996. 36: 593-7
17. Ito K, Miyahara T, Goto T, Horiuchi T, Sakai K, Hongo K. Solitary metastatic cauda equina tumor from breast cancer. Neurol Med Chir (Tokyo). 2010. 50: 417-20
18. Jeon MJ, Kim TY, Han JM, Yim JH, Rhim SC, Kim WB. Intramedullary spinal cord metastasis from papillary thyroid carcinoma.Thyroid. 2011. 21: 1269-71