- Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Fujieda, Japan.
Correspondence Address:
Ryo Kanematsu, Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Fujieda, Japan.
DOI:10.25259/SNI_299_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryo Kanematsu, Junya Hanakita, Toshiyuki Takahashi, Manabu Minami, Sho Nakamura, Shinya Tokunaga, Izumi Suda. Intraoperative complications of vertebral body stenting system. 28-Apr-2023;14:156
How to cite this URL: Ryo Kanematsu, Junya Hanakita, Toshiyuki Takahashi, Manabu Minami, Sho Nakamura, Shinya Tokunaga, Izumi Suda. Intraoperative complications of vertebral body stenting system. 28-Apr-2023;14:156. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12295
Abstract
Background: Vertebral body stenting systems (VBSs) are superior to balloon kyphoplasty for performing vertebral augmentation and height restoration. However, VBS may likely result in more material-related complications that have been under-reported. Here, an 84-year-old female’s vertebral stents “toppled over” before the filling cement was fully applied, thus necessitating an additional posterior fusion.
Case Description: An 84-year-old female presented with low back pain after a fall. Dynamic standing and decubitus X-rays revealed a vertebral compression fracture at T12 resulting in an intravertebral vacuum cleft (i.e., the lowermost level of diffuse idiopathic skeletal hyperostosis). When the VBS was performed, the stents “toppled over” just after removing the balloon catheters; we successfully restored with the cement volume in one stent but not the other, thus warranting an additional posterior fusion to maintain stability.
Conclusion: The proper injection of cement into a VBS requires dual correct stent positioning, and careful control of requisite stent expansion. In an 84-year-old female with a T12 vertebral body fracture and a remarkable vacuum cleft, the VBS procedure resulted in an inadvertent injection into one stent thus warranting a secondary posterior fusion.
Keywords: Material failures, Stent tumbling motion, Stent-related complication, Vertebral body stenting system (VBS)
INTRODUCTION
Vertebral body stenting systems (VBSs) are superior to percutaneous vertebroplasty and balloon kyphoplasty (BKP) for augmenting and restoring vertebral body height following vertebral compression fractures.[
CASE DESCRIPTION
Clinical presentation
An 84-year-old female presented with low back pain. Standing/decubitus dynamic X-rays revealed a vertebral compression fracture at T12 level accompanied by an intravertebral vacuum cleft (i.e., the lower-most level of diffuse idiopathic skeletal hyperostosis [DISH]) [
A VBS was planned to treat the T12 vertebral compression fracture.
Surgery
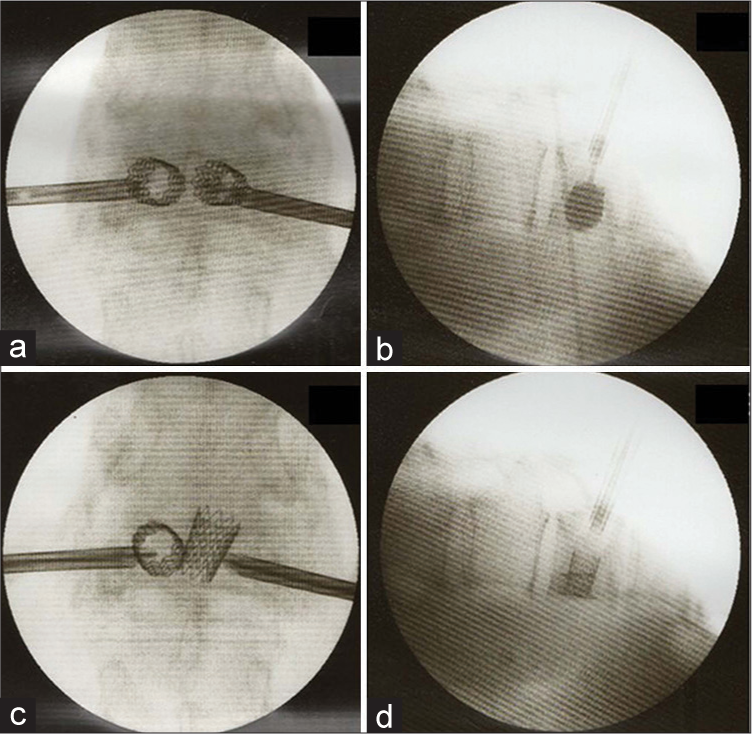
Under fluoroscopic-guidance, the drill and blunt plungers from a vertebral body stent access kit were inserted transpedicularly through working sleeves to create working “channels” for the stents. Inflation catheters were inserted and balloons were expanded until appropriate reduction and/or complete balloon expansion had occurred within the T12 vertebral (i.e., inflation of balloons inside the vertebral body) [
Figure 2:
Balloon was expanded until either appropriate reduction or complete balloon expansion within the vertebral body. The stents were deployed through inflation of the balloon inside the vertebral body, confirming the stability between the endplate and stent (a and b). However, the right side stent toppled over just after removing balloon catheter and it was difficult to inject the cement into the toppled stent (c and d).
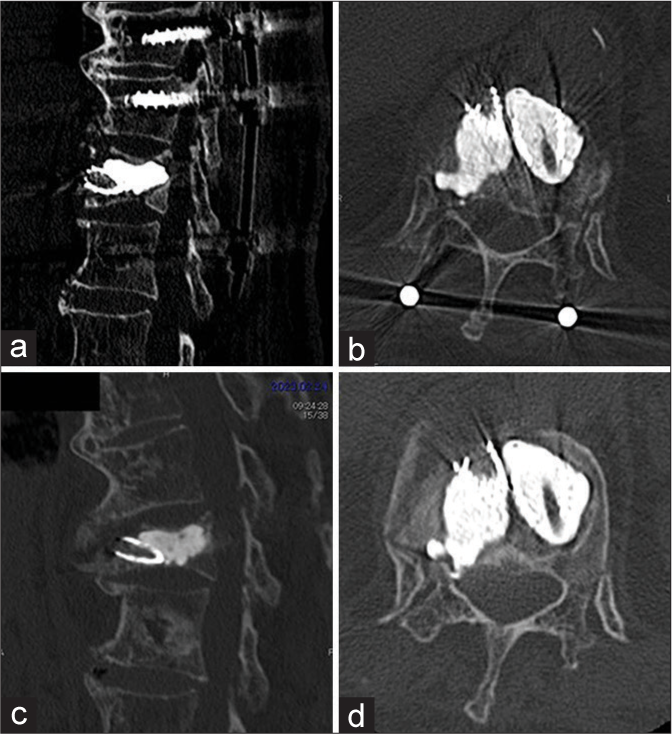
Figure 3:
Vertebral body stenting system and additional posterior fixation was performed at the three levels spanning from Th10 to L1 because the pedicles above Th11 and below L2 were too narrow to insert screws. The stent edge directed toward ventral side (a and b). Bony fusion to Th11 covering beaked stent was achieved and pedicle screws were removed 1 year after operation (c and d).
DISCUSSION
Stent-related complications
VBS is less able to tolerate errors is versus BKP, especially in the presence of an immobile fracture, and/or a sclerotic zone that may contribute to incomplete stent expansion.[
CONCLUSION
For VBS, it is not only critical that stent positioning be correct, but that the stent can tolerate expansion following the injection of cement. In this 84-year-old female with a T12 vertebral body fracture and DISH, the inadvertent “tumbling motion” and failure to fill the right-sided stent (i.e., only adequately filled left stent) required a secondary posterior fusion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Diel P, Röder C, Perler G, Vordemvenne T, Scholz M, Kandziora F. Radiographic and safety details of vertebral body stenting: Results from a multicenter chart review. BMC Musculoskelet Disord. 2013. 14: 233
2. Disch AC, Schmoelz W. Cement augmentation in a thoracolumbar fracture model: Reduction and stability after balloon kyphoplasty versus vertebral body stenting. Spine (Phila Pa 1976). 2014. 39: E1147-53
3. Oswald KA, Kälin J, Tinner C, Deml MC, Bigdon SF, Hoppe S. Anterior thoracolumbar column reconstruction with the vertebral body stent-safety and efficacy. Eur Spine J. 2023. 32: 934-49
4. Rotter R, Martin H, Fuerderer S, Gabl M, Roeder C, Heini P. Vertebral body stenting: A new method for vertebral augmentation versus kyphoplasty. Eur Spine J. 2010. 19: 916-23
5. Werner CM, Osterhoff G, Schlickeiser J, Jenni R, Wanner GA, Ossendorf C. Vertebral body stenting versus kyphoplasty for the treatment of osteoporotic vertebral compression fractures: A randomized trial. J Bone Joint Surg Am. 2013. 95: 577-84