- Department of Neurosurgery, Baylor College of Medicine, One Baylor Plaza, Houston, TX, United States.
- Department of Neurosurgery, Houston Methodist Hospital Neurological Institute, Houston, TX, United States.
Correspondence Address:
Sricharan Gopakumar
Department of Neurosurgery, Baylor College of Medicine, One Baylor Plaza, Houston, TX, United States.
DOI:10.25259/SNI_130_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sricharan Gopakumar, William J. Steele, Matthew Muir, Zain Bhogani, Gavin Britz. Intraspinal mesenchymal chondrosarcoma: An argument for aggressive local resection and adjuvant therapy based on review of the literature. 02-May-2020;:95
How to cite this URL: Sricharan Gopakumar, William J. Steele, Matthew Muir, Zain Bhogani, Gavin Britz. Intraspinal mesenchymal chondrosarcoma: An argument for aggressive local resection and adjuvant therapy based on review of the literature. 02-May-2020;:95. Available from: https://surgicalneurologyint.com/surgicalint-articles/9987/
Abstract
Background: Mesenchymal chondrosarcoma is a rare cartilaginous neoplasm that typically involves the axial skeleton. Despite a well-circumscribed appearance, this tumor has a tendency to recur both locally and with distant metastases.
Case Description: A 17-year-old patient presented with numbness and paresthesias in the lower extremities attributed to a T10-T11 intradural extramedullary mesenchymal chondrosarcoma. The patient was treated with aggressive local resection and adjuvant therapy. Here, this case and present literature are appropriately reviewed.
Conclusion: Although uncommon, intraspinal mesenchymal chondrosarcomas warrant both radical local resection and aggressive adjuvant therapy with chemoradiation to provide the greatest chance of progression-free survival.
Keywords: Adjuvant therapy, Intradural tumor, Intraspinal, Mesenchymal chondrosarcoma
INTRODUCTION
Mesenchymal chondrosarcomas are rare, primary malignant neoplasms of bone and soft tissues that arise from primitive cartilage forming mesenchymal tissue and are capable of distant metastasis.[
Patient case
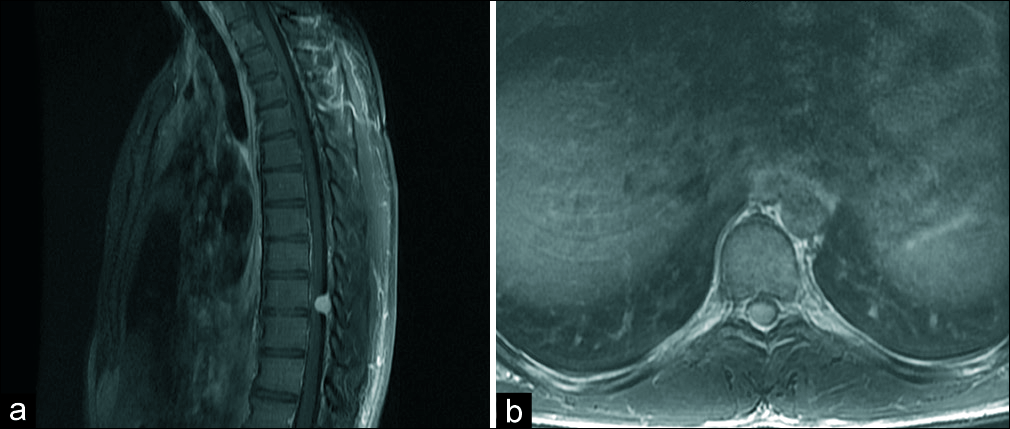
A 17-year-old male presented with a 5-week onset of progressive lower extremity numbness and hyperreflexia attributed to a primary T10-T11 intradural extramedullary mesenchymal chondrosarcoma. Contrast-enhanced T1-weighted magnetic resonance imaging (MRI) of the thoracic spine showed an intradural posterolateral right-sided lesion at the T10-11 level compressing the spinal cord anteriorly [
Due to the high risk of local tumor recurrence, the patient underwent a second operation with further resection of surrounding tissues.[
DISCUSSION
Background
Mesenchymal chondrosarcomas are rare tumors, constituting 25% of all chondrosarcomas in children and adolescents.[
Diagnosis
On MRI imaging, these tumors often have extraosseous extension, lytic lesions, poorly defined periosteal reaction, and mottled calcification.[
Management
Mesenchymal chondrosarcoma is known to have a late recurrence, sometimes even more than 20 years after the primary tumor occurs.[
The use of chemotherapy in the treatment of mesenchymal chondrosarcomas in the literature is controversial.[
CONCLUSION
Intradural extramedullary mesenchymal chondrosarcomas are rare tumors that require prompt diagnosis, aggressive wide surgical excision, and adjuvant radiation and chemotherapy to achieve the best outcomes. Here, a 17-year- old male with a T10-T11 mesenchymal chondrosarcoma underwent a secondary operation with total en bloc resection, including dural removal with patch grafting plus adjuvant chemoradiation to avoid tumor recurrence.
Declaration of patient consent
Patient’s consent not obtained as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bishop MW, Somerville JM, Bahrami A, Kaste SC, Interiano RB, Wu J. Mesenchymal chondrosarcoma in children and young adults: A single institution retrospective review. Sarcoma. 2015. 2015: 608279-
2. Cesari M, Bertoni F, Bacchini P, Mercuri M, Palmerini E, Ferrari S. Mesenchymal chondrosarcoma. An analysis of patients treated at a single institution. Tumori. 2007. 93: 423-7
3. Chan HS, Turner-Gomes SO, Chuang SH, Fitz CR, Daneman A, Martin DJ. A rare cause of spinal cord compression in childhood from intraspinal mesenchymal chondrosarcoma. A report of two cases and review of the literature. Neuroradiology. 1984. 26: 323-7
4. Dabska M, Huvos AG. Mesenchymal chondrosarcoma in the young. Virchows Arch A Pathol Anat Histopathol. 1983. 399: 89-104
5. De Amorim Bernstein K, Liebsch N, Chen YL, Niemierko A, Schwab JH, Raskin K. Clinical outcomes for patients after surgery and radiation therapy for mesenchymal chondrosarcomas. J Surg Oncol. 2016. 114: 982-6
6. Douis H, Saifuddin A. The imaging of cartilaginous bone tumours. II. Chondrosarcoma. Skeletal Radiol. 2013. 42: 611-26
7. Frezza AM, Cesari M, Baumhoer D, Biau D, Bielack S, Campanacci DA. Mesenchymal chondrosarcoma: Prognostic factors and outcome in 113 patients. A European musculoskeletal oncology society study. Eur J Cancer. 2015. 51: 374-81
8. Fu YS, Kay S. A comparative ultrastructural study of mesenchymal chondrosarcoma and myxoid chondrosarcoma. Cancer. 1974. 33: 1531-42
9. Harsh GR, Wilson CB. Central nervous system mesenchymal chondrosarcoma. Case report. J Neurosurg. 1984. 61: 375-81
10. Huvos AG, Rosen G, Dabska M, Marcove RC. Mesenchymal chondrosarcoma. A clinicopathologic analysis of 35 patients with emphasis on treatment. Cancer. 1983. 51: 1230-7
11. Kawaguchi S, Weiss I, Lin PP, Huh WW, Lewis VO. Radiation therapy is associated with fewer recurrences in mesenchymal chondrosarcoma. Clin Orthop Relat Res. 2014. 472: 856-64
12. Lee ST, Lui TN, Tsai MD. Primary intraspinal dura mesenchymal chondrosarcoma. Surg Neurol. 1989. 31: 54-7
13. Lichtenstein L, Bernstein D. Unusual benign and malignant chondroid tumors of bone. A survey of some mesenchymal cartilage tumors and malignant chondroblastic tumors, including a few multicentric ones, as well as many atypical benign chondroblastomas and chondromyxoid fibromas. Cancer. 1959. 12: 1142-57
14. Nakashima Y, Unni KK, Shives TC, Swee RG, Dahlin DC. Mesenchymal chondrosarcoma of bone and soft tissue. A review of 111 cases. Cancer. 1986. 57: 2444-53
15. Obuchowicz AK, Szumera-Ciećkiewicz A, Ptaszyński K, Rutynowska-Pronicka O, Madziara W, Tiszler-Cieślik E. Intraspinal mesenchymal chondrosarcoma in a 14-year-old patient: Diagnostic and therapeutic problems in relation to the review of literature. J Pediatr Hematol Oncol. 2012. 34: e188-92
16. Rushing EJ, Armonda RA, Ansari Q, Mena H. Mesenchymal chondrosarcoma: A clinicopathologic and flow cytometric study of 13 cases presenting in the central nervous system. Cancer. 1996. 77: 1884-91