- Department of Neonatology, Fukuoka Children's Hospital, Fukuoka, Japan
- Department of Neurosurgery, Fukuoka Children's Hospital, Fukuoka, Japan
- Department of Clinical Radiology, Fukuoka Children's Hospital, Fukuoka, Japan
- Department of Pediatric Neurology, Fukuoka Children's Hospital, Fukuoka, Japan
Correspondence Address:
Nobuya Murakami
Department of Pediatric Neurology, Fukuoka Children's Hospital, Fukuoka, Japan
DOI:10.4103/sni.sni_139_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoichiro Serita, Takato Morioka, Nobuya Murakami, Nobuko Kawamura, Yasushi Takahata, Ryutaro Kira. Intraventricular hemorrhage possibly extending from an infratentorial subdural hematoma via a perforated suprapineal recessus in a full-term neonate. 01-Nov-2017;8:266
How to cite this URL: Yoichiro Serita, Takato Morioka, Nobuya Murakami, Nobuko Kawamura, Yasushi Takahata, Ryutaro Kira. Intraventricular hemorrhage possibly extending from an infratentorial subdural hematoma via a perforated suprapineal recessus in a full-term neonate. 01-Nov-2017;8:266. Available from: http://surgicalneurologyint.com/surgicalint-articles/intraventricular-hemorrhage-possibly-extending-from-an-infratentorial-subdural-hematoma-via-a-perforated-suprapineal-recessus-in-a-full%e2%80%91term-neonate/
Abstract
Background:Although intraventricular hemorrhage (IVH) is very rarely reported in full-term neonates, it may occur in children with perinatal trauma, asphyxia, and coagulation disorders, and may originate in the choroid plexus and residual subependymal germinal matrix layer.
Case Description:We present the case of a full-term baby with IVH. She had no perinatal problems or coagulation disorders. Sagittal views of neuroimages demonstrated that the IVH possibly extended from a subdural hemorrhage (SDH) in the infratentorial area via a perforated suprapineal recessus. This was barely visible on a conventional axial view of a computed tomographic scan.
Conclusion:When the etiopathogenesis of IVH in a full-term baby with an uncomplicated delivery cannot be clearly defined, multi-directional and multi-modal neuroimaging may be useful.
Keywords: Full-term birth, infratentorial subdural hemorrhage, intraventricular hemorrhage, suprapineal recessus
INTRODUCTION
Intraventricular hemorrhage (IVH) in the subependymal germinal matrix layer is the most common type of neonatal IVH. It is characteristically observed in premature infants,[
Here, we report the case of a full-term baby with IVH, which possibly extend from a subdural hemorrhage (SDH) in the infratentorial area via a perforated suprapineal recessus.
CASE REPORT
A full-term (37 weeks and 4 days) baby girl was born in good general condition by vaginal delivery. Her 22-year-old mother (gravida 1, para 1) experienced an unremarkable pregnancy, apart from testing positive for chlamydia antibody at 28 weeks, for which she received azithromycin. The girl's birth weight was 2862 g, length 48 cm, head circumference 33 cm, and Apgar score 9/10. Thirty minutes after her birth, sporadic ventricular premature contractions were frequently observed. She started breastfeeding 8 hours after birth, and she vomited a couple of times. She developed apneic attacks during the night. Subsequently, generalized seizure was observed in the morning of the next day and she was transferred to our hospital.
On arrival, the girl was not very active. There were no trauma-related lesions, including cephalohematoma, on her outer surface. Her seizure was controlled using intravenous administration of phenobarbital. Peripheral blood count and coagulation tests, including prothrombin time and activated partial thromboplastin time, were within normal limits. Ultrasound imaging of her head showed a high echoic lesion in the lateral ventricles. Axial computed tomographic (CT) images revealed IVH in the bilateral lateral ventricles, the 3rd ventricle and the 4th ventricle. However, SDH with subarachnoid hemorrhage (SAH) was barely visible compared with the IVH [
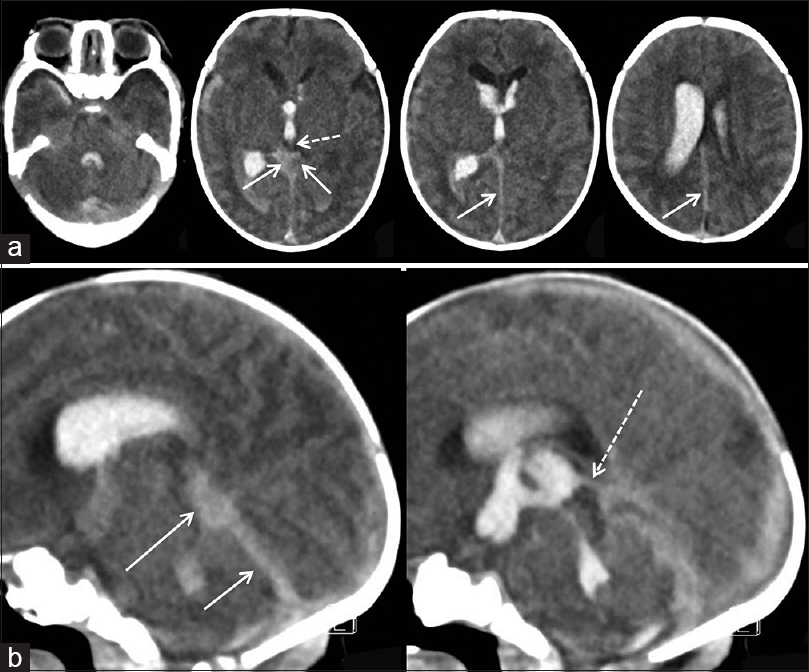
Figure 1
Computed tomographic (CT) scan on day 1 after birth. (a) Axial images revealing intraventricular hemorrhage (IVH) in the lateral ventricles, the 3rd ventricle, and the 4th ventricle. Compared with the IVH, the subdural hemorrhage (SDH) in the infratentorial space and tentorial incisura (white arrows), and the hematoma in the suprapineal recessus (white dotted arrow) are barely visible. (b) Mid-sagittal views. The quadrigeminal cistern in the tentorial incisura (white arrows) is seem to be connected to the IVH in the third ventricle via the suprapineal recessus (white dotted arrow)
Because her fontanel was not tense and general conditions were good, conservative therapy for the intracranial hemorrhage was selected. Although protein C activity was slightly decreased (probably due to her intracranial hemorrhage), protein S activity, antithrombin III, and factor XIII were within normal limits.
Around day 13 after birth, the girl's head circumference had gradually increased in size. On day 18, magnetic resonance (MR) images showed marked enlargement of the entire ventricular system [
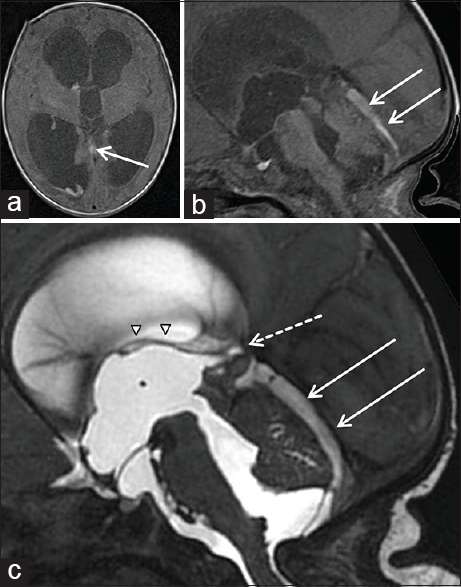
Figure 2
Magnetic resonance (MR) images on day 18 after birth. (a) Axial and (b) sagittal views of T1-weighted images show marked enlargement of the ventricular system. The infratentorial SDH persists (white arrows), while most of the IVH is resolved. (c) Sagittal heavily T2-weighted images show an enlarged suprapineal recessus (white dotted arrow), which appears to extend into the infratentorial SDH (white arrows). Internal cerebral veins (ICVs) are depicted as a linear signal void at the roof of the third ventricle and the suprapineal recessus (white arrow heads)
On Day 19, the girl underwent a ventricle-peritoneal (VP) shunt through the right anterior horn. Her postoperative course was uneventful and her development corresponded to her age.
DISCUSSION
In this full-term baby, without coagulation disorders, both massive IVH and infratentorial SDH was observed at first CT scan. Although most of the IVH was resolved, infratentorial SDH persisted at follow-up MRI. However, the causative bleeding spot of the IVH was not noted. These findings might indicate that the SDH was the primary hemorrhagic site and the IVH was an extension of the infratentorial SDH.
The most common etiology of infratentorial SDH is disruption of the tentorium or falx with tearing of the bridging veins due to mechanical compression and distortion of the head during birth.[
Spontaneous SDH located in the infratentorial region is difficult to see on axial CT scans, since the axial plane is not completely parallel to the tentorium, and it can therefore be overlooked.[
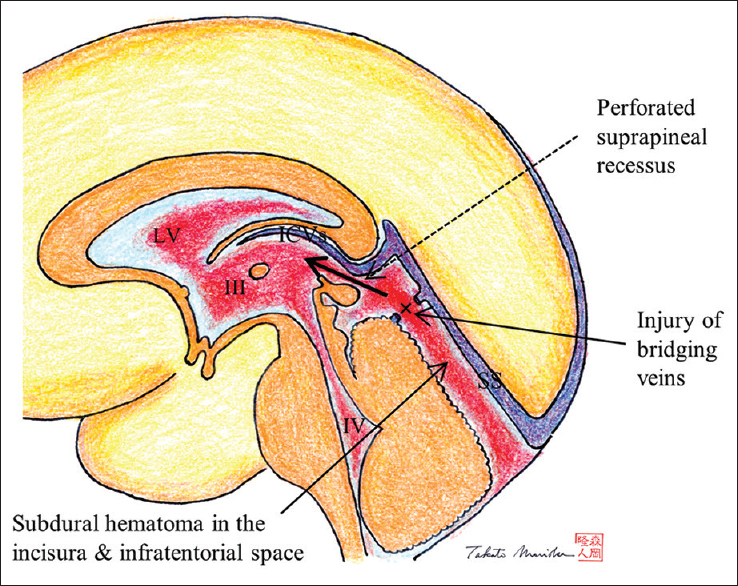
Figure 3
A schematic drawing of our hypothesis concerning the IVH development in this case. Infratentorial SDH, which occurred owing to injury of bridging veins (indicated with x) from the straight sinus (SS) near the suprapineal recessus. The ependyma of the suprapineal recessus was perforated below the entry of ICVs (bold black arrow) and thus IVH (indicated with bold black arrow) developed in the 3rd ventricle (III), the bilateral lateral ventricle (LV), and the 4th ventricle (IV)
The outcome of the infratentorial SDH depends on the parenchymal and brainstem involvement.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahmad K, Zafar Janjua N, Bin Hamza H, Imran Khan M. Spontaneous subdural haemorrhage in new born babies. Lancet. 2004. 363: 2001-2
2. Brouwer AJ, Groenendaal F, Koopman C, Nievelstein R-JA, Han SK, de Vries LS. Intracranila hemorrhage in full-term newborns: A hospital-based cohort study. Neuroradiology. 2010. 52: 567-76
3. Chamnanvanakij S, Rollins N, Perlman JM. Subdural hematoma in term infants. Pediat Neurol. 2002. 26: 301-4
4. Hayashi T, Hashimoto T, Fukuda S, Ohshima Y, Moritaka K. Neonatal subdural hematoma secondary to birth injury. Clinical analysis of 48 survivors. Childs Nerv Syst. 1987. 3: 23-9
5. Ichiyama M, Ohga S, Ochiai M, Fukushima K, Ichimura M, Torio N. Fetal hydrocephalus and neonatal stroke as the first presentation of protein C deficiency. Brain Dev. 2016. 38: 253-6
6. Morioka T, Hashiguchi K, Nagata S, Miyagi Y, Mihara F, Hikino S. Fetal germinal matrix and intraventrucular hemorrhage. Pediatr Neurosurg. 2006. 42: 354-61
7. Perrin RG, Rutka JT, Drake JM, Maltzer H, Hellman J, Jay V. Management and outcome of posterior fossa subdural hematomas in neonates. Neurosurgery. 1997. 40: 1190-200
8. Rhoton AL J.editors. The lateral and third ventricles. RHOTON Cranial anatomy and surgical approaches. Maryland: Lippincott Williams & Wilkins; 2003. p. 235-99
9. Sahriarian S, Akbari P, Amini E, Dalili H, Esmaeilnia Shrivany T, Niknafs N. Intraventricular hemorrhage in a term neonate: Manifestation of protein S deficiency. A case report. Iran J Public Health. 2016. 45: 531-4
10. Szpecht D, Frydryszak D, Miszezyk N, Szymankiewicz M, Gadzinowski J. The incidence of severe intraventricular hemorrhage based on retrospective analysis of 35939 full-term newborns. Report of two cases and review of literature. Childs Nerv Syst. 2016. 32: 2447-51
11. Usul H, Karaarslan G, Cakir E, Kuzeyl K, Mungan I, Baykal S. Conservative management of spontaneous posterior fossa subdural hematoma in a neonate. J Clin Neurosci. 2004. 12: 196-8
12. Whitby EH, Griffiths PD, Rutter S, Smith MF, Springg A, Ohadike P. Frequency and natural history of subdural haemorrhages in babies and relation to obstetric factors. Lancet. 2003. 362: 846-50