- Department of Radiodiagnosis, J N Medical College, Aligarh, India
- Department of Neurosurgery, J N Medical College, Aligarh, India
Correspondence Address:
Saifullah Khalid
Department of Radiodiagnosis, J N Medical College, Aligarh, India
DOI:10.4103/2152-7806.195232
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Saifullah Khalid, Amber Obaid, Raman M. Sharma, Asad Mahmood, Sabarish Narayanasamy. Intraventricular migration of an isolated fourth ventricular cysticercus following cerebrospinal fluid shunting. 05-Dec-2016;7:
How to cite this URL: Saifullah Khalid, Amber Obaid, Raman M. Sharma, Asad Mahmood, Sabarish Narayanasamy. Intraventricular migration of an isolated fourth ventricular cysticercus following cerebrospinal fluid shunting. 05-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/intraventricular-migration-of-an-isolated-fourth-ventricular-cysticercus-following-cerebrospinal-fluid-shunting/
Abstract
Background:Isolated intraventricular neurocysticercosis (NCC) is less frequently seen and can be missed on plain magnetic resonance imaging (MRI). Three-dimensional constructive interference in steady state (CISS) sequence is an extremely helpful sequence in identifying the lesion but is rarely used routinely.
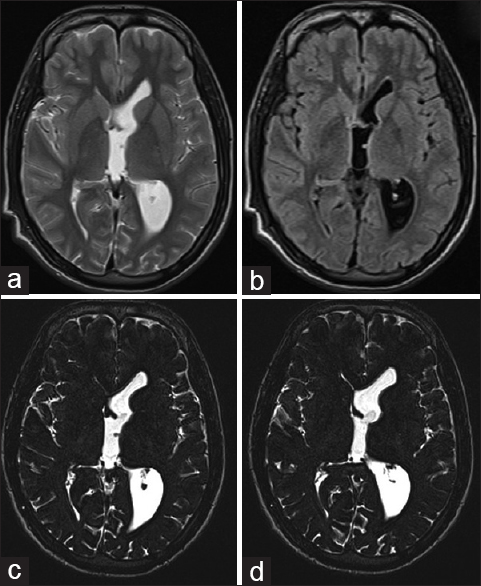
Case Description:Here, we report a case of young male adult who presented with diminution of vision and headache. MRI of the brain revealed hydrocephalus, and on using CISS sequence only, the lesion could be identified in the fourth ventricle. He was treated with medical management, and ventriculoperitoneal shunting of cerebrospinal fluid was done to relieve the hydrocephalus. It resulted in immediate relief with aggravation of headache few days later. Repeat MRI revealed intraventricular migration into the left foramen of monro leading to left lateral ventricle dilatation necessitating endoscopic removal of the lesion.
Conclusion:CISS sequence is definitely the sequence of choice in identifying intraventricular NCC. Ventriculoperitoneal shunting can result in the intraventricular migration of the cyst due to sudden decompression necessitating repeat surgery. Endoscopic removal of NCC has a high success rate with limited complications.
Keywords: CISS sequence, endoscopic, intraventricular, migration, neurocysticercosis, VP shunting
INTRODUCTION
Neurocysticercosis (NCC) is caused by an infection of the central nervous system (CNS) by the larval stage of the pork tapeworm Taenia solium. It is endemic in India and is prevalent in other developing nations, with increasing incidence in developed countries due to globalization.[
CASE REPORT
A 17-year-old male patient presented to the ophthalmology outpatient department with complaints of headache and diminution of vision for the last 20 days. There was no history of fever or trauma. There were no signs of meningeal irritation. The vitals were within normal limit. The clinical evaluation revealed relative afferent pupillary defect in the left eye with evidence of bilateral papilledema on fundoscopy. The patient was advised MRI of the brain to rule out any cerebral pathology. MRI revealed communicating hydrocephalus with no evidence of any space occupying lesion. No lesion could be identified on plain MRI. The MRI was reviewed due to a high index of clinical suspicion, and the possibility of a very tiny nodule in the fourth ventricle was raised, which necessitated further imaging with with constructive interference in steady state (CISS) sequence [
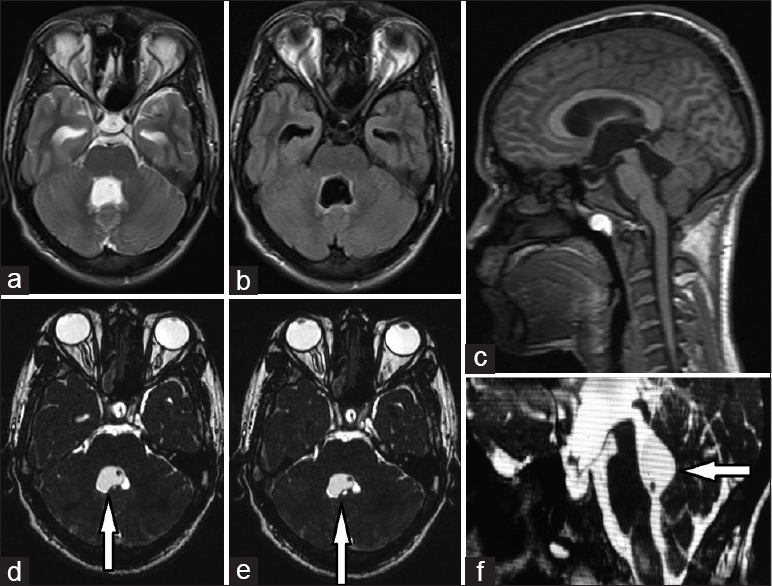
Figure 1
T2-weighted (a), fluid-attenuated inversion recovery (b) axial images, sagittal MP-RAGE (c) shows enlarged fourth ventricle with dilated temporal horns of bilateral lateral ventricle. There is no suspicion of any cystic lesion except for an appreciation of a dot which turns out to be scolex. The cystic lesion with eccentric scolex is easily appreciated on constructive interference in steady state sequence (d, e, f)
DISCUSSION
It is a disease of the young population with equal gender predilection.[
This case is not only important from a diagnostic point of view but from the management perspective as well. While most common presentation is seizures noted in patients suffering from the parenchymal form, 20–30% of the patients can present with raised intracranial pressure and hydrocephalus, which is attributable to the intraventricular form.[
Apuzzo et al.,[
CONCLUSION
Intraventricular NCC could be a cause for unexplained hydrocephalus. MRI with three dimensional-CISS sequence is definitely the imaging of choice in identifying intraventricular NCC. Sudden change of pressure differential by the ventriculoperitoneal shunting could result in intraventricular migration of the cyst. Recurrence of symptoms or headache after shunt surgery in cases of intraventricular NCC should be viewed with suspicion for potential intraventricular migration. Endoscopic removal of NCC has a high success rate with limited complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anandh B, Mohanty A, Sampath S, Praharaj SS, Kolluri S. Endoscopic Approach to Intraventricular Cysticercal Lesions. Minim Invasive Neurosurg. 2001. 44: 194-6
2. Apuzzo ML, Dobkin WR, Zee CS, Chan JC, Giannotta SL, Weiss MH. Surgical considerations in treatment of intraventricular cysticercosis. An analysis of 45 cases. J Neurosurg. 1984. 60: 400-7
3. Araujo ALE, Rodrigues RS, Marchiori E, Pinheiro RA, Flores M, Alves JR. Migrating intraventricular cysticercosis: Magnetic resonance imaging findings. Arq Neuropsiquiatr. 2008. 66: 111-3
4. Citow JS, Johnson JP, McBride DQ, Ammirati M. Imaging features and surgery related outcome in intraventricular neurocysticercosis. Neurosurg Focus. 2002. 12: e6-
5. Garcia HH, Del Brutto OH. Neurocysticercosis: Updated concepts about an old disease. Lancet Neurol. 2005. 4: 653-61
6. Garcia HH, Gonzalez AE, Evans CA, Gilman RH. Taenia solium cysticercosis. Lancet. 2003. 362: 547-56
7. Garcia HH, Gonzalez AE, Tsang VC, Gilman RH. Neurocysticercosis: Some of the essentials. Pract Neurol. 2006. 6: 288-97
8. Goel RK, Ahmad FU, Vellimana AK, Suri A, Chandra PS, Kumar R. Endoscopic management of intraventricular neurocysticercosis. J Clin Neurosci. 2008. 15: 1096-101
9. Govindappa SS, Narayanan JP, Krishnamoorthy VM, Shastry CH, Balasubramaniam A, Krishna SS. Improved detection of intraventricular cysticercal cysts with the use of three-dimensional constructive interference in steady state MR sequences. AJNR Am J Neuroradiol. 2000. 21: 679-84
10. Herrera SR, Chan M, Alaraj AM, Neckrysh S, Lemole MG, Amin-Hanjani S. CT Ventriculography for diagnosis of occult ventricular cysticerci. Surg Neurol Int. 2010. 1: 92-
11. Hingwala D, Chatterjee S, Kesavadas C, Thomas B, Kapilamoorthy TR. Applications of 3D CISS sequence for problem solving in neuroimaging. Indian J Radiol Imaging. 2011. 21: 90-7
12. Husain M, Jha DK, Rastogi M, Husain N, Gupta RK. Neuro-endoscopic management of intraventricular neurocysticercosis (NCC). Acta Neurochir. 2007. 149: 341-6
13. Kotha VK. Migration of intraventricular neurocysticercus after ventriculostomy. Asian J Neurosurg. 2013. 8: 54-6
14. McCormick GF, Zee CS, Heiden J. Cysticercosis cerebri: Review of 127 cases. Arch Neuro. 1982. 39: 534-9
15. Teitelbaum GP, Otto RJ, Lin M, Watanabe AT, Stull MA, Manz HJ. MR imaging of neurocysticercosis. AJR Am J Roentgenol. 1989. 153: 857-66