- Department of Spinal Disorders, Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, United Kingdom,
- Department of Radiodiagnosis, Institute of Medical Sciences and SUM Hospital, Bhubaneshwar, Odisha,
- Department of Spine Surgery, Apollo Hospital, Mumbai, Maharashtra, India.
Correspondence Address:
Alok Gadkari, Department of Spinal Disorders, Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, United Kingdom.
DOI:10.25259/SNI_398_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Aashish Ghodke1, Sumedha Singh2, Alok Gadkari1, Dheeraj Batheja1, Ram Chaddha3. Isolated costotransverse joint tuberculosis - A rare location for tubercular arthritis. 23-Jun-2022;13:266
How to cite this URL: Aashish Ghodke1, Sumedha Singh2, Alok Gadkari1, Dheeraj Batheja1, Ram Chaddha3. Isolated costotransverse joint tuberculosis - A rare location for tubercular arthritis. 23-Jun-2022;13:266. Available from: https://surgicalneurologyint.com/surgicalint-articles/11673/
Abstract
Background: Posterior element involvement of the spine with tuberculosis (TB) is very uncommon.
Case Description: A 25-year-old immunocompetent female presented with dull mid-back ache and tenderness over the inferior angle of the left scapula and left 7th costovertebral junction. The MRI showed erosion and enhancing soft tissue in the periarticular region of the left 7th costotransverse joint. After the CT-guided biopsy confirmed the diagnosis of TB, she was successfully managed with antitubercular chemotherapy.
Conclusion: In a 25-year-old female, the early diagnosis of atypical TB involving the left T7 costotransverse joint allowed for allowed for its successful treatment/resolution with antitubercular chemotherapy.
Keywords: Atypical TB, Costotransverse joint, Tuberculosis
INTRODUCTION
Spinal tuberculosis (TB) is a commonly encountered extrapulmonary type of TB that generally involves two or more vertebral bodies. Paravertebral soft-tissue shadows are also frequently seen.[
CASE REPORT
Clinical presentation
A 25-year-old female presented with the left dull mid-back pain for 3 months’ duration. The pain was moderate and radiated to the left breast/precordium. The physical examination just revealed focal tenderness over the inferior angle of the left scapula/7th costovertebral junction, without swelling or erythema.
Lab studies
The patient had a raised erythrocyte sedimentation rate of 40 and C-reactive protein of 6. Serological testing for HIV, hepatitis B, and hepatitis C was all negative.
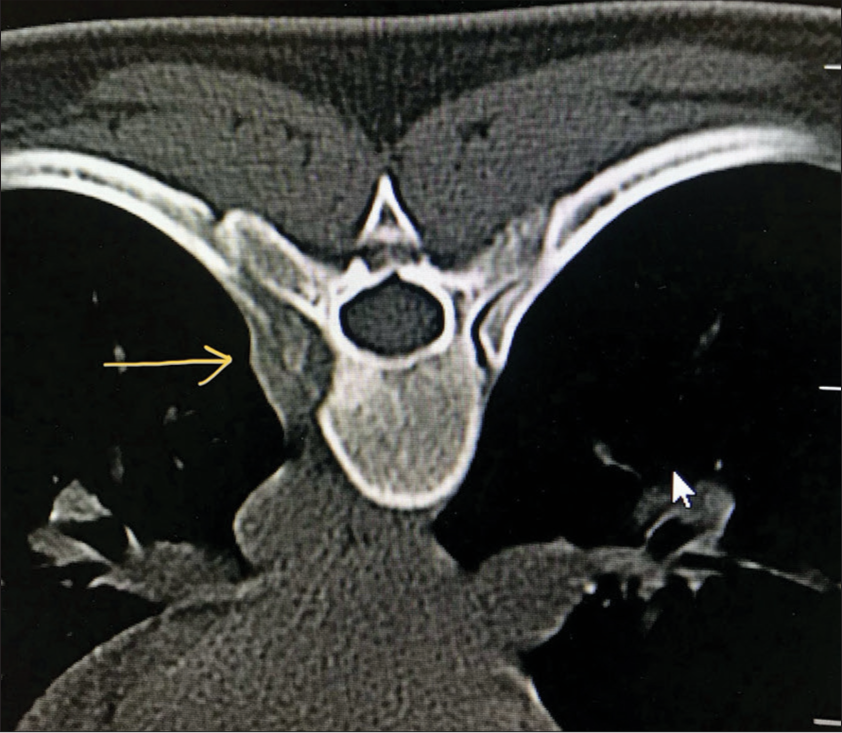
MR/CT evaluations
The anteroposterior X-rays of the thoracic spine showed that the T7 vertebral body was scalloped on the left side, and there erosion of the T7 left pedicle and adjoining rib [
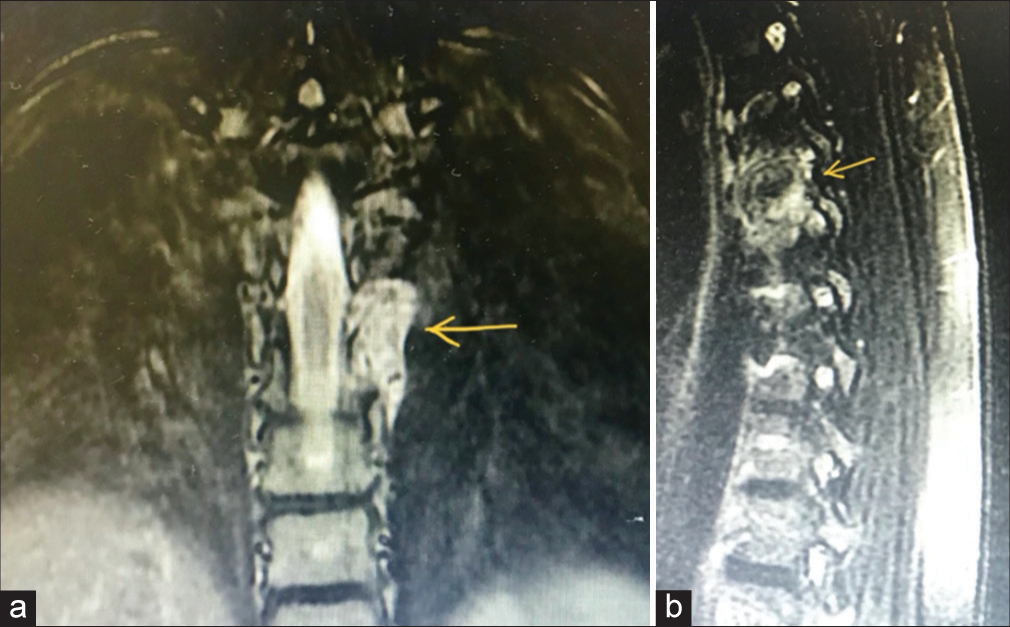
Figure 2:
(a and b) Magnetic resonance imaging showed enhancing periarticular erosive lesions and marrow edema in the posteromedial portion of the left 7th rib, left posterolateral portion of the D7 vertebral body, and lateral portion of the left T7 pedicle, thickening and enhancement of synovium of the 7th costotransverse joint with enhancing soft tissue elevating the overlying pleura, and abutting the descending aorta. a: Yellow arrow shows coronal MRI (T2 )image showing enhancement of the soft tissue. b: Yellow arrow shows saggital MRI (T2)imaging showing periarticular erosive lesions and marrow edema (left T7 pedicle)
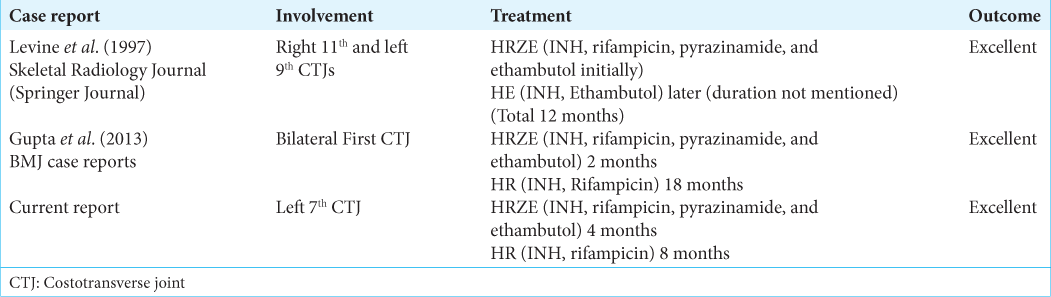
ATT
ATT for the first 4 months included rifampicin, isoniazid, pyrazinamide, and ethambutol (HRZE) (intensive phase). For the next 8 months, the patient received rifampicin and isoniazid (HR) (continuation phase). At follow-up (12 months), the patient showed clinical and radiological signs of healing [
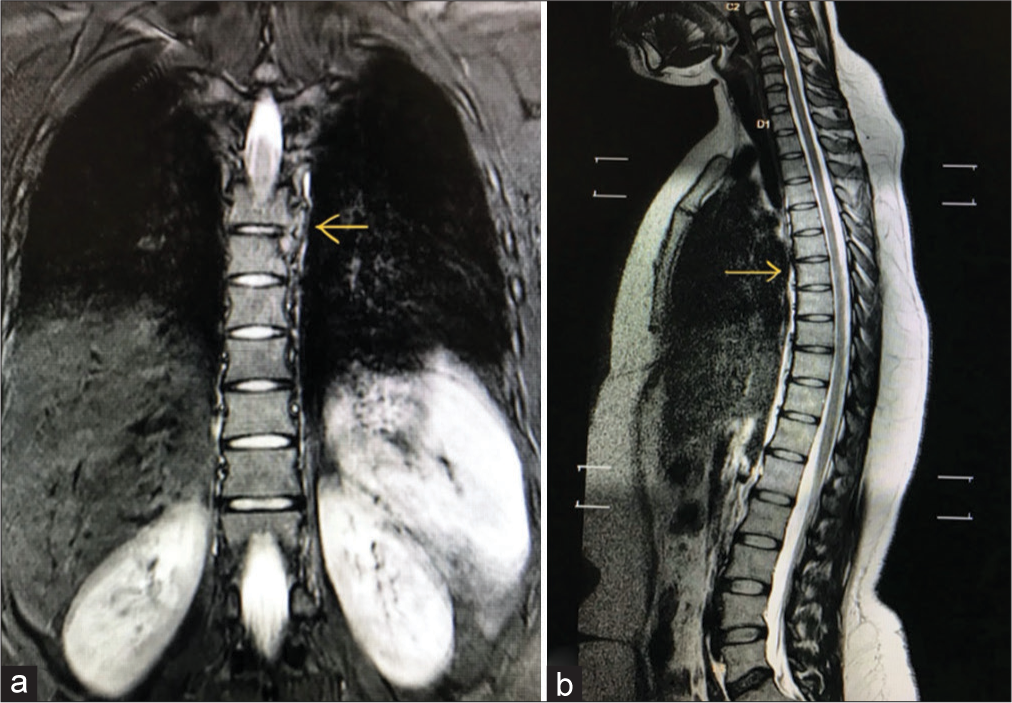
Figure 4:
(a and b) MRI at 12 months follow-up showed complete resolution of the erosive lesions and associated enhancing soft tissue with no residual enhancing lesion or collection. a: Yellow arrow shows coronal MRI (T2) image showing resolution of lesion. b: Yellow arrow shows Sagittal MRI (T2) image showing resolution of lesion.
DISCUSSION
Spinal TB accounts for 1–3% of all TB cases.[
Rare posterior element involvement with TB
Involvement of the posterior elements is generally caused by spread of Mycobacterium from a primary focus through Batson’s venous plexus.[
CONCLUSION
TB can atypically involve the costotransverse joints (i.e., posterior elements). Early diagnosis with MR and CT-guided biopsy for pathological confirmation and subsequent adequate TB treatment should result in good outcomes.[
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Garg RK, Somvanshi DS. Spinal tuberculosis: A review. J Spinal Cord Med. 2011. 34: 440-54
2. Guedes G. Tuberculosis and immunosuppression. J Microbiol Exp. 2018. 6: 145-6
3. Gupta M, Jain VK, Naik AK, Arya RK. Tuberculosis of bilateral first costotransverse joints. BMJ Case Rep. 2013. 2013: bcr2013010490
4. Levine SM, Marianacci EB, Kattapuram SV. Tuberculosis of contralateral costo-transverse joints. Skeletal Radiol. 1997. 26: 741-3
5. Pande KC, Babhulkar SS. Atypical spinal tuberculosis. Clin Orthop Relat Res. 2002. 398: 67-74
6. Tuli SM. General principles of osteoarticular tuberculosis. Clin Orthop Relat Res. 2002. 398: 11-9
7. Yalniz E, Pekindil G, Aktas S. Atypical tuberculosis of the spine. Yonsei Med J. 2000. 41: 657-61
8. Yazdi T, Rahimizadeh A. An illustrative case Isolated posterior spinal arch tuberculosis. World Spinal Column J. 2012. 3: 98-101