- Department of Neurosurgery, King Edward Medical University, Lahore, Mayo Hospital, Lahore, Punjab, Pakistan.
Correspondence Address:
Adnan Qasim, Department of Neurosurgery, King Edward Medical University, Lahore, Mayo Hospital, Lahore - 54000, Punjab, Pakistan
DOI:10.25259/SNI_721_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sundus Ali, Adnan Qasim, Rahmatullah Salah, Muhammad Rizwan Sarwar, Muhammad Usman, Shahzad Shams. Isolated late intradural cauda equina metastasis of renal cell carcinoma. 30-Sep-2021;12:481
How to cite this URL: Sundus Ali, Adnan Qasim, Rahmatullah Salah, Muhammad Rizwan Sarwar, Muhammad Usman, Shahzad Shams. Isolated late intradural cauda equina metastasis of renal cell carcinoma. 30-Sep-2021;12:481. Available from: https://surgicalneurologyint.com/surgicalint-articles/11147/
Abstract
Background: The cauda equina (CE) is the most common site for intradural extramedullary metastasis from systemic malignancies such as lung, breast, and thyroid carcinomas. However, renal cell carcinomas (RCC), with their high metastatic potential, are rarely responsible for CE metastatic lesions. Here, we report an intradural cauda equina mass, as the first and only site of metastasis of a renal cell carcinoma.
Case Description: A 55-year-old female had undergone a left nephrectomy for renal cell carcinoma 8 years ago. She now presented with a unifocal renal cell metastasis to the CE. As such metastases are rare, establishing the correct pathological diagnosis proved to be a challenge.
Conclusion: The cauda equina was the first and only site of an 8-year-delayed metastasis attributed to a renal cell carcinoma.
Keywords: Cauda equina, Intradural, Isolated, Metastasis, Renal cell carcinoma
INTRODUCTION
Renal cell carcinoma (RCC) is known for its high metastatic potential. At the time of diagnosis, 30% of patients with RCC already have metastases, and another 78% of these occur within the first 5 years.[
CLINICAL PRESENTATION
A 55-year-old female had undergone a left-sided nephrectomy 8 years ago for clear/renal-cell carcinoma (RCC). She now presented with a two-month history of gradually progressive low back pain with radiation into the left lower extremity. Her neurological examination only demonstrated a lack of pin appreciation in the left L3 distribution, while all routine laboratory studies were within normal limits.
Radiographic evaluation
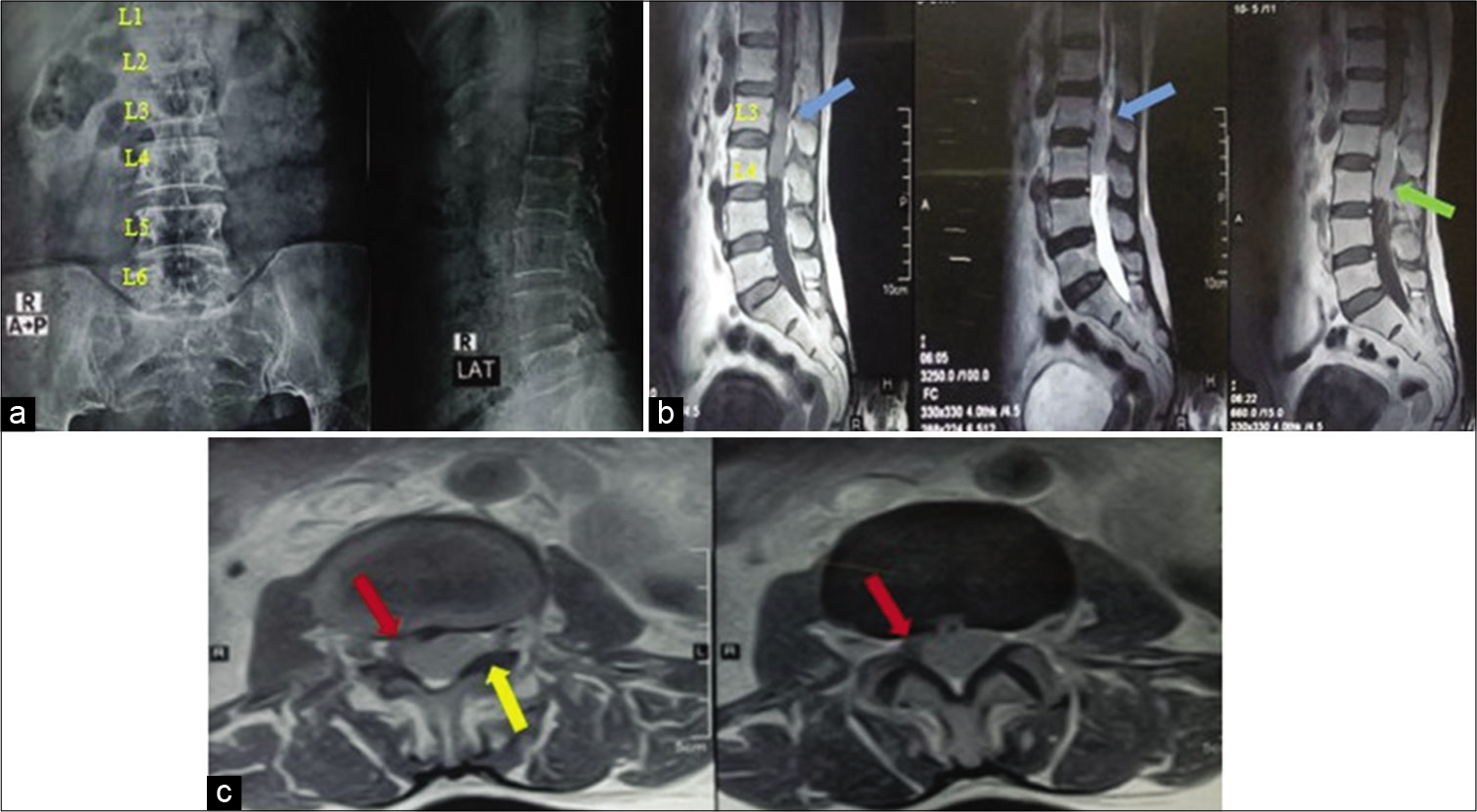
The plain X-rays only showed lumbarization of S1 [
Figure 1:
(a) Plain X-ray Lumbosacral spine showing 6 lumbar vertebrae, to aid in marking level per operatively. (b) Sagittal MRI lumbosacral spine showing rectangular mass at L3-4 level, isointense on T1 and T2, and mild homogenous contrast uptake. (Level counted taking X-ray into consideration). (c) Axial MRI at L4 level, showing well-defined homogenously enhancing mass, extending toward left neural foramina (marked with yellow arrow), displacing the cauda equina to the right side (marked in red).
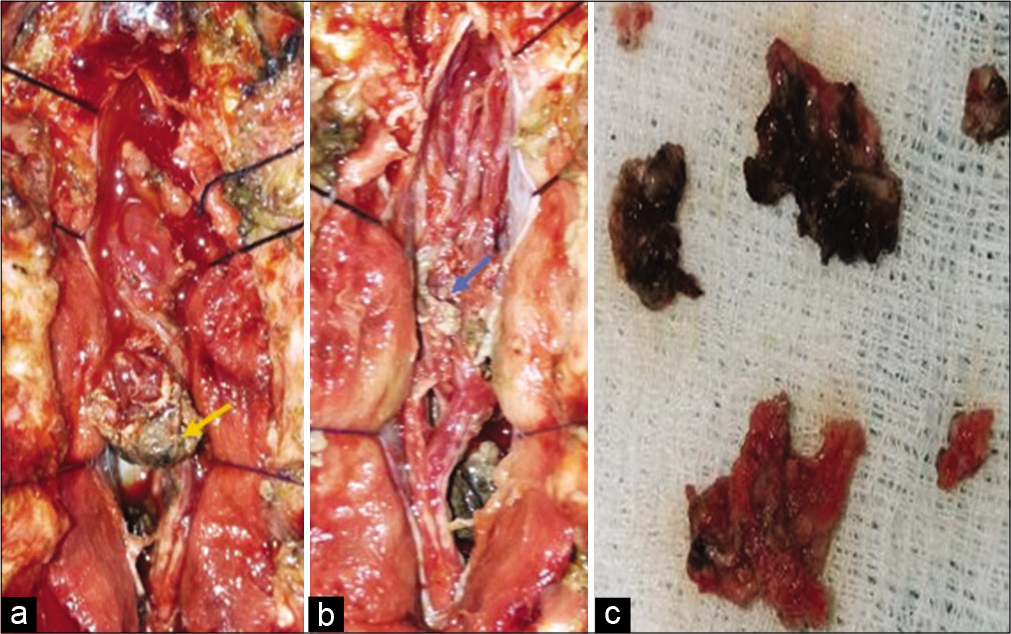
Surgery
Following a L3-L4 laminectomy and midline durotomy, with the opening of the arachnoid membrane, revealed a firm, vascular lesion densely adherent to multiple roots. The caudal pole was readily skeletonized from the cauda equina, but was adherent to the L3 nerve root exiting through the left L3/L4 foramen; it was sacrificed [
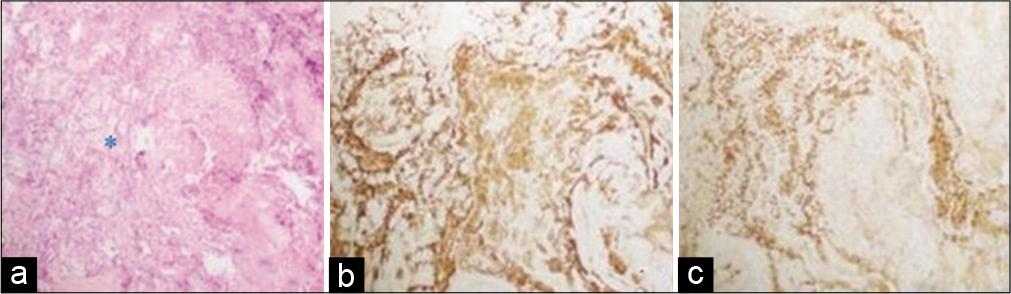
Histology/immunochemistry
The tumor’s histological features were consistent with metastatic renal cell carcinoma, as were the results of immunohistochemical stains (i.e., positive for PAX8 and Cam5.2) [
Figure 3:
(a) Photomicrograph of Hematoxylin and Eosin stain showing polygonal cells with hyperchromatic nuclei, scanty cytoplasm arranged in alveolar pattern (marked with *) typical of clear cell carcinoma, (b) PAX 8 immunostaining showing distinct nuclear reactivity characteristic of renal origin and (c) CAM 5.2 antibody immunostaining for CK8 showing diffuse positivity thus verifying epithelial origin. All images are ×100 original magnification.
DISCUSSION
Cancers that metastasize to the intradural lumbar spine (i.e., breast, lung, thyroid, and gastrointestinal malignancies in decreasing frequency). are rare. The account just for 6% of all spinal metastases,[
Surgery and Histopathological Confirmation of Isolated Metastasis of RCC to CE
Although our provisional diagnosis was for a L3-L4 nerve sheath tumor, intraoperatively, the tumor’s adherence to multiple roots of the CE and lack of a proper capsule was more consistent with a malignant lesion such as RCC.
In addition, histopathology showed the characteristic clear cells arranged in an alveolar pattern classic for RCC while specific immunohistochemical stains (i.e., PAX 8 and CAM 5.) differentiated clear cell/RCC from other organ tumors (i.e, adrenal vs. liver).[
Prognosis and treatment
RCC has a 5-year survival of between 0 and 10%; therefore, aggressive surgical resection is warranted for solitary metastases. Resection of a distant solitary RCC metastasis provides effective local control (i.e., as in this case) and contributes to a 35–50% 5-year survival with adjuvant therapy. Notably, RCC only poorly responds to the typical non-surgical adjuvant therapies (i.e, chemotherapy, hormonal therapy, immunotherapy (8% response rate) and radiotherapy).[
CONCLUSION
The cauda equina (i.e., intradural/extramedullary) is an uncommon site for metastasis of renal cell carcinoma. Therefore, even patients with remote (i.e., 8 years ago in this case) histories of RCC malignancies many years later can present with CE metastases.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
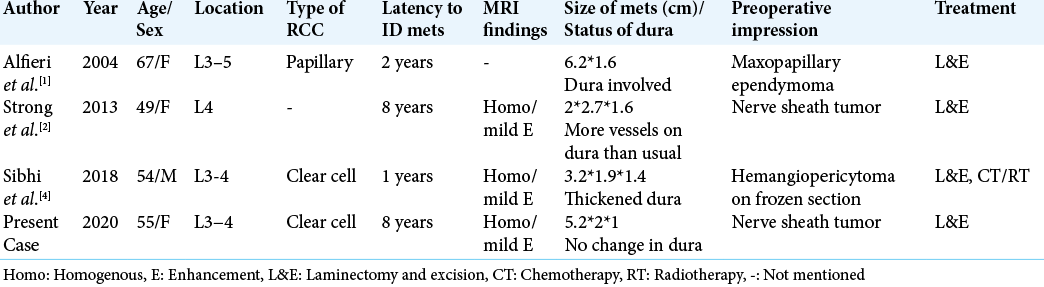
1. Alfieri A, Mazzoleni G, Schwarz A, Campello M, Broger M, Vitale M. Renal cell carcinoma and intradural spinal metastasis with cauda equina infiltration: Case report. Spine (Phila Pa 1976). 2005. 30: 161-3
2. Carminucci A, Hanft S. Intradural extramedullary spinal metastasis of renal cell carcinoma: Illustrative case report and comprehensive review of the literature. Eur Spine J. 2020. 29: 176-82
3. Ganapathy S, Gopal S, Godhani N, Raju A. Isolated cauda equina metastasis from renal cell carcinoma-a rare cause of intradural-extramedullary compression. IP Indian J Neurosci. 2018. 4: 82-5
4. Jost G, Zimmerer S, Frank S, Cordier D, Merlo A. Intradural spinal metastasis of renal cell cancer. Report of a case and review of 26 published cases. Acta Neurochir (Wien). 2009. 151: 815-21
5. Noguchi G, Nakaigawa N, Taguri M, Tsutsumi S, Saito Y, Fukui S. Time-dependent change in relapse sites of renal cell carcinoma after curative surgery. Clin Exp Metastasis. 2018. 35: 69-75
6. Shen SS, Truong LD, Scarpelli M, Lopez-Beltran A. Role of immunohistochemistry in diagnosing renal neoplasms: When is it really useful?. Arch Pathol Lab Med. 2012. 136: 410-7
7. Son HS, Jeon SH, Chang SG. Factors affecting the time to recurrence after radical nephrectomy for localized renal cell carcinoma. Korean J Urol. 2013. 54: 744-9
8. Strong C, Yanamadala V, Khanna A, Walcott BP, Nahed BV, Borges LF. Surgical treatment options and management strategies of metastatic renal cell carcinoma to the lumbar spinal nerve roots. J Clin Neurosci. 2013. 20: 1546-9
9. Tan PH, Cheng L, Rioux-Leclercq N, Merino MJ, Netto G, Reuter VE. Renal tumors: Diagnostic and prognostic biomarkers. Am J Surg Pathol. 2013. 37: 1518-31
10. Thyavihally YB, Mahantshetty U, Chamarajanagar RS, Raibhattanavar SG, Tongaonkar HB. Management of renal cell carcinoma with solitary metastasis. World J Surg Oncol. 2005. 3: 48