- Department of Neurosurgery, University of Cincinnati (UC) College of Medicine, Cincinnati, Ohio, USA
- Mayfield Clinic, Cincinnati, Ohio, USA
Correspondence Address:
Yair M. Gozal
Department of Neurosurgery, University of Cincinnati (UC) College of Medicine, Cincinnati, Ohio, USA
Mayfield Clinic, Cincinnati, Ohio, USA
DOI:10.4103/2152-7806.196770
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yair M. Gozal, Kristine Atchley, Bradford A. Curt. Isolated oculomotor nerve palsy after lumbar epidural steroid injection in a diabetic patient. 26-Dec-2016;7:
How to cite this URL: Yair M. Gozal, Kristine Atchley, Bradford A. Curt. Isolated oculomotor nerve palsy after lumbar epidural steroid injection in a diabetic patient. 26-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/isolated-oculomotor-nerve-palsy-after-lumbar-epidural-steroid-injection-in-a-diabetic-patient/
Abstract
Background:In patients with diabetes mellitus, epidural steroid injections (ESI) have been noted to cause significant elevation of blood glucose levels, typically lasting 1–3 days. Here, we describe a previously unreported complication of a diabetic third nerve palsy associated with an ESI.
Case Description:A 66-year-old man with a history of coronary artery disease, hypertension, and insulin-dependent diabetes mellitus presented with low back pain and left lower extremity radiculopathy. The lumbar magnetic resonance imaging (MRI) revealed mild spondylosis, most severe at the L4-5 level, accompanied by a broad based disc protrusion resulting in mild central and moderate biforaminal stenosis. The patient underwent a left-sided L4-L5 transforaminal ESI resulting in transient elevation of his blood glucose levels. On post-procedure day 2, he developed a frontal headache and a complete right third nerve palsy with partial pupillary involvement. The MRI and MR angiography (MRA) of the brain revealed no compressive lesions or oculomotor abnormalities. Ophthalmoplegia and pupillary dysfunction resolved spontaneously over 4 months.
Conclusions:Although rare, a history of a recent ESI should be considered as the etiology of an isolated oculomotor palsy in diabetic patients.
Keywords: Diabetes mellitus, epidural steroid injections, oculomotor nerve palsy, ophthalmoplegia
INTRODUCTION
The use of epidural steroids in diabetic patients is controversial. Multiple studies have demonstrated an association between epidural steroid injections (ESI) and increased insulin-resistance, poor glycemic control, and an elevated risk of infection.[
CASE REPORT
Clinical presentation
A 66-year-old male with a history of coronary artery disease, hypertension, and insulin-dependent diabetes mellitus (DM) presented with 2 months of low back pain, left buttock/leg pain radiating down to the calf, and numbness in the L5 distribution. The lumbar magnetic resonance imaging (MRI) revealed mild L4-5 spondylosis with moderate biforaminal stenosis, accompanied by left L5-S1 lateral recess stenosis.
Epidural steroid injection and post-injection course
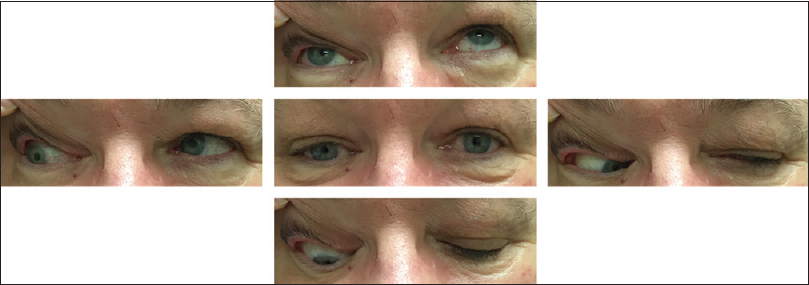
The patient was referred for bilateral selective L4-5 foraminal ESIs utilizing Betamethasone (9 mg per injection) and Bupivacaine under fluoroscopic guidance. There were no immediate post-procedural complications. However, 2 days later, the patient progressively developed a frontal headache, right eye ptosis, and inferolateral displacement of gaze with mild mydriasis of the the right pupil (4 mm OD vs. 2 mm OS), consistent with a right third nerve palsy with partial pupillary involvement [
Figure 1
Photographs demonstrating ophthalmoplegia secondary to the right third nerve palsy with involvement of the pupil. The center panel demonstrates the extent of ptosis at rest and characteristic “down and out” position of the eye. Remaining images demonstrate eye position during voluntary gaze in each direction relative to the center panel
Figure 2
Post-procedure average recorded blood glucose (mg/dL) over 1 month after epidural steroid injection (ESI). Each point represents the average blood glucose obtained from the patient's personal glucometer calculated in 3-day bins. Initial value (day 0) reflects the blood glucose level recorded at the treatment center immediately before ESI
DISCUSSION
Diabetes-associated oculomotor palsy affects ~0.5% of all diabetic patients and accounts for 11–42% of all third nerve palsies.[
Multiple studies have documented elevated mean blood glucose concentrations and insulin resistance lasting between 1–7 days following epidural steroids in diabetic patients.[
DM affects more than a quarter of Americans over the age of 65 and is disproportionally common in patients with spinal stenosis.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Even JL, Crosby CG, Song Y, McGirt MJ, Devin CJ. Effects of epidural steroid injections on blood glucose levels in patients with diabetes mellitus. Spine. 2012. 37: E46-50
2. Goldstein JE, Cogan DG. Diabetic ophthalmoplegia with special reference to the pupil. Arch Ophthalmol. 1960. 64: 592-600
3. Greco D, Gambina F, Maggio F. Ophthalmoplegia in diabetes mellitus: A retrospective study. Acta Diabetol. 2009. 46: 23-6
4. Green WR, Hackett ER, Schlezinger NS. Neuro-Ophthalmologic Evaluation of Oculomotor Nerve Paralysis. Arch Ophthalmol. 1964. 72: 154-67
5. Jacobson DM. Pupil involvement in patients with diabetes-associated oculomotor nerve palsy. Arch Ophthalmol. 1998. 116: 723-727
6. Keane JR. Third nerve palsy: Analysis of 1400 personally-examined inpatients. Can J Neurol Sci. 2010. 37: 662-70
7. Kwan ES, Laucella M, Hedges TR, Wolpert SM. A cliniconeuroradiologic approach to third cranial nerve palsies. AJNR Am J Neuroradiol. 1987. 8: 459-68
8. Shimizu H, Shimomura Y, Inukai T, Takahashi M, Uehara Y, Kobayashi I. Immediate improvement of diabetic mononeuropathy after intravenous administration of prostaglandin E1. Jpn J Med. 1990. 29: 222-5
9. Simopoulos TT, Kraemer JJ, Glazer P, Bajwa ZH. Vertebral osteomyelitis: A potentially catastrophic outcome after lumbar epidural steroid injection. Pain Physician. 2008. 11: 693-7
10. Watanabe K, Hagura R, Akanuma Y, Takasu T, Kajinuma H, Kuzuya N. Characteristics of cranial nerve palsies in diabetic patients. Diabetes Res Clin Pract. 1990. 10: 19-27