- Departments of Neurosurgery, Avicenne Military Hospital of Marrakech and Mohammed V University in Rabat, Rabat, Morocco.
- Departments of Physical Medicine and Functional Rehabilitation, Avicenne Military Hospital of Marrakech and Mohammed V University in Rabat, Rabat, Morocco.
Correspondence Address:
Ali Akhaddar
Departments of Physical Medicine and Functional Rehabilitation, Avicenne Military Hospital of Marrakech and Mohammed V University in Rabat, Rabat, Morocco.
DOI:10.25259/SNI_287_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Akhaddar A, Arabi H. Isolated painless scoliosis in lumbar disc herniation. Surg Neurol Int 20-Jun-2020;11:159
How to cite this URL: Akhaddar A, Arabi H. Isolated painless scoliosis in lumbar disc herniation. Surg Neurol Int 20-Jun-2020;11:159. Available from: https://surgicalneurologyint.com/surgicalint-articles/10094/
To the Editor,
Painful scoliosis and lumbar disc herniations (LDHs) are well documented in the pediatric, adolescent, and young adult populations.[
CASE REPORT
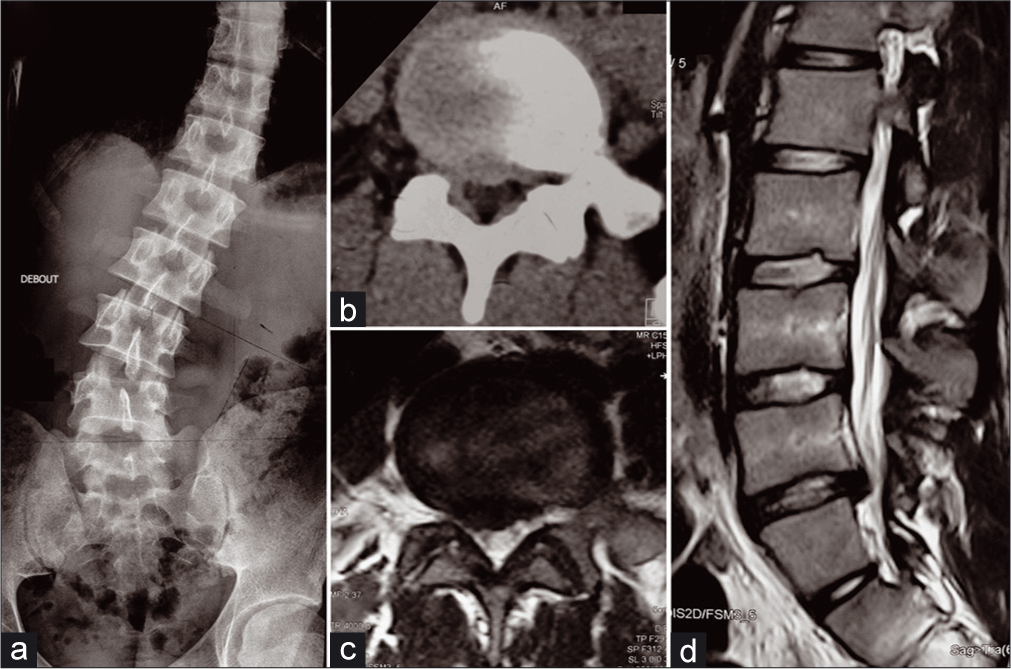
A 24-year-old male presented with a 12-month history of progressive scoliosis and difficulty walking without spinal or radicular pain. For the past several months, he had been misdiagnosed as having idiopathic scoliosis and was being treated with bracing and physical therapy without any improvement. On examination, he had a significant scoliotic deformity (i.e., tilt to the left) with a reduced range of lumbar motion and/muscle spasm restricting right lateral flexion [
Figure 2:
Anteroposterior plain radiograph of the thoracolumbar spine showing a primary right lumbar curve (Cobb angle 30° and 70 mm deviation) without rotational spinal deformity (a), axial lumbar spinal computed tomography scan (b), axial (c), and sagittal T2- weighted images (d) demonstrating a right paramedian lumbar disc herniation at L4–L5 level.
CONCLUSION
In the pediatric, adolescent, and young adult populations, and acute LDH should be ruled out with MR studies as potential causes of and/or contributing to “deformity” before assigning a diagnosis of thoracolumbar scoliosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akhaddar A, Belfquih H, Oukabli M, Boucetta M. Posterior ring apophysis separation combined with lumbar disc herniation in adults: A 10-year experience in the surgical management of 87 cases. J Neurosurg Spine. 2011. 14: 475-83
2. Krishnan KM, Newey ML. Lumbar scoliosis associated with a disc herniation in an adult. Rheumatol (Oxford). 2001. 40: 1427-8
3. Suk KS, Lee HM, Moon SH, Kim NH. Lumbosacral scoliotic list by lumbar disc herniation. Spine (Phila Pa 1976). 2001. 15: 667-71