- Department of Neurosurgery, Princess Alexandra Hospital, Brisbane, QLD, Australia
- Department of Anatomical Pathology, Princess Alexandra Hospital, Brisbane, QLD, Australia
Correspondence Address:
Saif Yousif
Department of Neurosurgery, Princess Alexandra Hospital, Brisbane, QLD, Australia
DOI:10.4103/sni.sni_244_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Saif Yousif, Guy Lampe, Ananthababu Pattavilakom. Large frontal osseous hemangioma with dural sinus involvement in a patient with Klippel-Trenaunay syndrome: A rare case report. 11-Oct-2018;9:205
How to cite this URL: Saif Yousif, Guy Lampe, Ananthababu Pattavilakom. Large frontal osseous hemangioma with dural sinus involvement in a patient with Klippel-Trenaunay syndrome: A rare case report. 11-Oct-2018;9:205. Available from: http://surgicalneurologyint.com/surgicalint-articles/9033/
Abstract
Background:We present one of the first documented cases in the literature of an adult with Klippel-Trenaunay syndrome (KTS) with a large frontal osseous hemangioma.
Case Description:A 30-year-old male presented with a rapidly enlarging frontal skull lesion that had developed in only 3 months. Radiological investigation revealed a highly vascular lesion attached to the frontal bone. The lesion was surgically resected with the patient making complete recovery. Histopathology was consistent with an osseous hemangioma.
Conclusion:We report the clinical presentation and surgical management of a rare presentation of osseous hemangioma in a patient with KTS.
Keywords: Hemangioma, Klippel-Trenaunay syndrome, Neuropathology
INTRODUCTION
Klippel-Trenaunay syndrome (KTS) is a rare congenital disorder characterized by the classic triad of capillary malformation, venous malformation, and limb overgrowth.[
CASE REPORT
A 30-year-old male with a known history of KTS presented with a rapidly enlarging subcutaneous central frontal mass, measuring 41 × 47 × 54 mm since its formation just 3 months earlier causing pain and an obvious cosmetic defect. The patient had no demonstrable neurological signs on examination with normal pre-operative laboratory studies, however, had previous episodes of significant hemorrhage arising from the lesion as a result of minor trauma.
Clinically, the patient was dysmorphic, most notably severe soft tissue overgrowth, bilateral lower limb lymphoedema, and cellulitis. Despite this, he had no history of other complications arising as a result of his KTS such as malignancy or peripheral hemangioma.
Radiological findings initially began with computed tomography angiogram, which revealed a destructive expansile arterially-enhancing lesion arising from the frontal bone. Heterogenous contrast enhancement on magnetic resonance imaging [
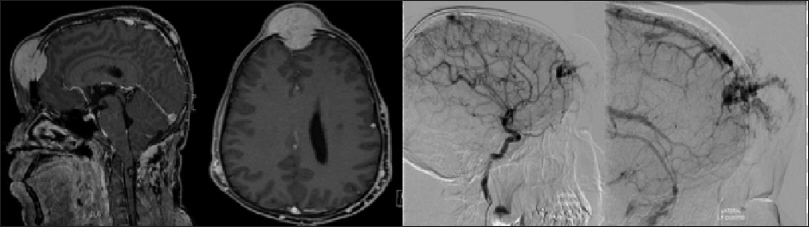
Figure 1
T1 weighted post contrast magnetic resonance imaging depicting the destructive nature and invasion of the vascular lesion; although it is closely associated with dura and superior saggital sinus, there is no evidence of parenchymal invasion. Digital Subtraction Cerebral Angiogram (right sided image) further characterizing the vascular lesion; arterial supply with fistulization from the ophthalmic artery and also some lesser arterial supply from the superficial temporal arteries bilaterally
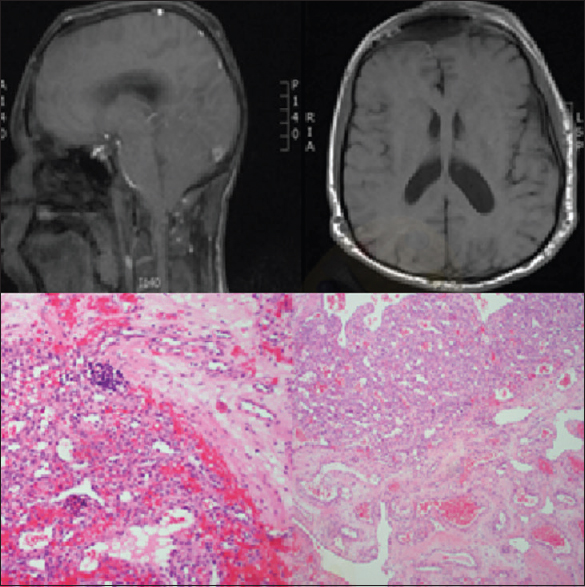
Gross total resection consisted of a T-shaped incision followed by bilateral frontal craniectomies [
Postoperatively, the patient had a full recovery. Histopathological hemotoxylin and eosin stains revealed the lesion extending through bone, with a small foci of extramedullary hemopoiesis, consistent with hemangioma. There has been no evidence of recurrence 6 months post resection.
DISCUSSION
Since its description in the early 20th century, prevalence has remained uncommon.
To our knowledge, vascular lesions arising from the skull in patients with KTS have not been previously described in the literature. Previous reports do highlight the increased prevalence and wide variability of malignancy in patients with KTS peripherally and in the spine.[
Hemangioma are benign vascular tumors, most commonly seen in pediatric age groups.[
Intraoperatively, the tumor was seen to locally invade into calvaria with evidence of skull remodeling and destruction which is scarcely discussed as a characteristic of vascular hemangioma in past literature. Gross total resection is the gold standard of therapy and recommended by the authors. This minimizes recurrence and allows for tissue histopathological diagnosis in a syndrome known for predisposition to malignancy. The role for non-operative management in hemangioma including radiotherapy still exists.[
Postoperatively, the patient received regular follow-up with radiological screening for tumor recurrence.
We, as the authors would like to highlight this unique case of an intracranial osseous hemangioma with frontal skull based origin in a patient with KTS, a rare syndrome with a predisposition to malignancy. There are associated dangers and complexities for the surgeon involved in resection of these uncommon lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Kihiczak GG, Meine JG, Schwartz RA, Janniger CK. Klippel-Trenaunay syndrome: A multisystem disorder possibly resulting from a pathogenic gene for vascular and tissue overgrowth. Int J Dermatol. 2006. 45: 883-90
2. Morace R, Marongiu A, Vangelista T, Galasso V, Colonnese C, Giangaspero F. Intracranial capillary hemangioma: A description of four cases. World Neurosurg. 2012. 78: 191.E15-21
3. Phi JH, Kim SK, Cho A, Kim DG, Paek SH, Park SH. Intracranial capillary hemangioma: Extra-axial tumorous lesions closely mimicking meningioma. J Neurooncol. 2012. 109: 177-85
4. Simon SL, Moonis G, Judkins AR, Scobie J, Burnett MG, Riina HA. Intracranial capillary hemangioma: Case report and review of the literature. Surg Neurol. 2005. 64: 154-9
5. Spallone A, Tcherekayev VA. Simultaneous occurrence of aneurysm and multiple meningioma in Klippel-Trenaunay patients: Case report. Surg Neurol. 1996. 45: 241-4
6. Uller W, Fishman SJ, Alomari AI. Overgrowth syndromes with complex vascular anomalies. Semin Pediatr Surg. 2014. 23: 208-15
7. Yilmaz T, Cikla U, Kirst A, Baskaya MK. Glioblastoma multiforme in Klippel-Trenaunay-weber syndrome: A case report. J Med Case Rep. 2015. 9: 83-