- Department of Neurosurgery, Helsinki University Central Hospital, Helsinki, Finland
- Department of Neurosurgery, Bergmannstrost Hospital Halle, Halle, Germany
- Burdenko Neurosurgical Institute, Russian Academy of Medical Sciences, Moscow, Russia
Correspondence Address:
Felix Goehre
Department of Neurosurgery, Helsinki University Central Hospital, Helsinki, Finland
DOI:10.4103/2152-7806.157793
Copyright: © 2015 Goehre F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Goehre F, Jahromi BR, Elsharkawy A, Lehto H, Shekhtman O, Andrade-Barazarte H, Munoz F, Hijazy F, Makhkamov M, Hernesniemi J. Lateral supraorbital approach to ipsilateral PCA-P1 and ICA-PCoA aneurysms. Surg Neurol Int 28-May-2015;6:91
How to cite this URL: Goehre F, Jahromi BR, Elsharkawy A, Lehto H, Shekhtman O, Andrade-Barazarte H, Munoz F, Hijazy F, Makhkamov M, Hernesniemi J. Lateral supraorbital approach to ipsilateral PCA-P1 and ICA-PCoA aneurysms. Surg Neurol Int 28-May-2015;6:91. Available from: http://surgicalneurologyint.com/surgicalint_articles/lateral-supraorbital-approach-ipsilateral-pca%e2%80%91p1-ica%e2%80%91pcoa/
Abstract
Background:Aneurysms of the posterior cerebral artery (PCA) are rare and often associated with anterior circulation aneurysms. The lateral supraorbital approach allows for a very fast and safe approach to the ipsilateral lesions Circle of Willis. A technical note on the successful clip occlusion of two aneurysms in the anterior and posterior Circle of Willis via this less invasive approach has not been published before. The objective of this technical note is to describe the simultaneous microsurgical clip occlusion of an ipsilateral PCA-P1 and an internal carotid artery - posterior communicating artery (ICA-PCoA) aneurysm via the lateral supraorbital approach.
Case Description:The authors present a technical report of successful clip occlusions of ipsilateral located PCA-P1 and ICA-PCoA aneurysms. A 59-year-old female patient was diagnosed with a PCA-P1 and an ipsilateral ICA-PCoA aneurysm by computed tomography angiography (CTA) after an ischemic stroke secondary to a contralateral ICA dissection. The patient underwent microsurgical clipping after a lateral supraorbital craniotomy. The intraoperative indocyanine green (ICG) videoangiography and the postoperative CTA showed a complete occlusion of both aneurysms; the parent vessels (ICA and PCA) were patent. The patient presents postoperative no new neurologic deficit.
Conclusion:The lateral supraorbital approach is suitable for the simultaneous microsurgical treatment of proximal anterior circulation and ipsilateral proximal PCA aneurysms. Compared to endovascular treatment, direct visual control of brainstem perforators is possible.
Keywords: Aneurysm, internal carotid artery, lateral supraorbital approach, posterior cerebral artery, posterior communicating artery
INTRODUCTION
Aneurysms of the posterior cerebral artery (PCA) are rare; less than 2% of all cerebral aneurysms involve the PCA.[
Several surgical approaches, such as the pterional,[
The objective of this technical report is to present the lateral supraorbital approach for the microsurgical clip occlusion of ipsilateral internal carotid artery - posterior communicating artery (ICA-PCoA) and PCA-P1 aneurysms under direct visual control of the crucial perforating branches originating from the P1 segment of PCA.
Illustrative case
History and examination
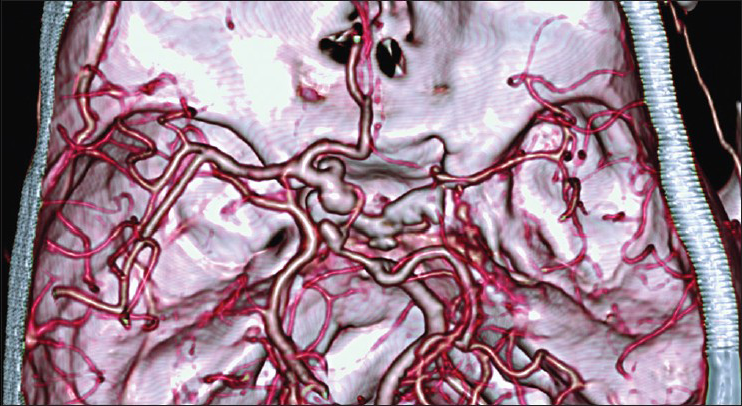
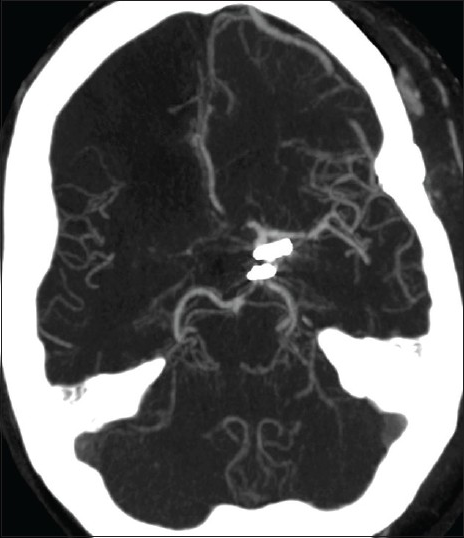
A 59-year-old female patient developed symptoms of a left hemiparesis and a neglect to the left by a right cerebral infarction secondary to an idiopathic right carotid artery dissection. Therefore a cervical and intracranial computed tomography angiography (CTA) was performed. The CTA showed an occlusion of the right carotid artery and two intracranial aneurysms [
Indication
The presented patient had multiple risk factors for intracranial aneurysm rupture (female gender, hypertension, smoker) and an occlusion of the contralateral ICA, which leads to an increasing flow through the affected vessels, ICA, and PCA. Therefore, the indication for an active treatment was given. The operative treatment was performed 6 month after the ischemic stroke.
Positioning and craniotomy
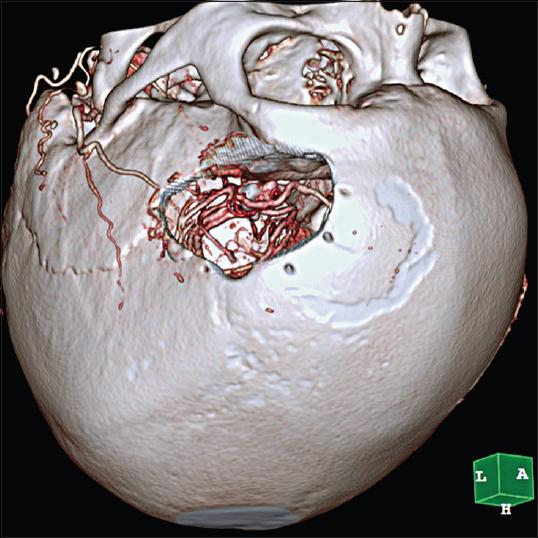
The patient was placed in the supine position with the head rotated 30° to the left using a Sugita clamp. The head was slightly elevated above the heart level. A fast one-layer skin-muscle flap followed by a left sided lateral supraorbital craniotomy was performed [
Intracranial dissection
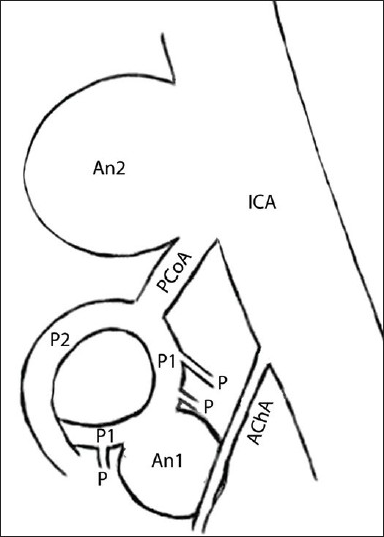
A schematic overview of the angioarchitecture in the surgical field is given in [
Figure 3
Schematic drawing of the PCoA complex, showing the angioarchitecture and the ICA-PCoA and PCA-P1 aneurysms. AChA – anterior choroidal artery, An1 - posterior cerebral artery P1 segment aneurysm, An2 – internal carotid artery - PCoA segment aneurysm, ICA – internal carotid artery, M1 - middle cerebral artery, P – midbrain perforating branches, P1 – posterior cerebral artery P1 segment, P2 – posterior cerebral artery P2 segment, PCoA – posterior communicating artery
Clip occlusion
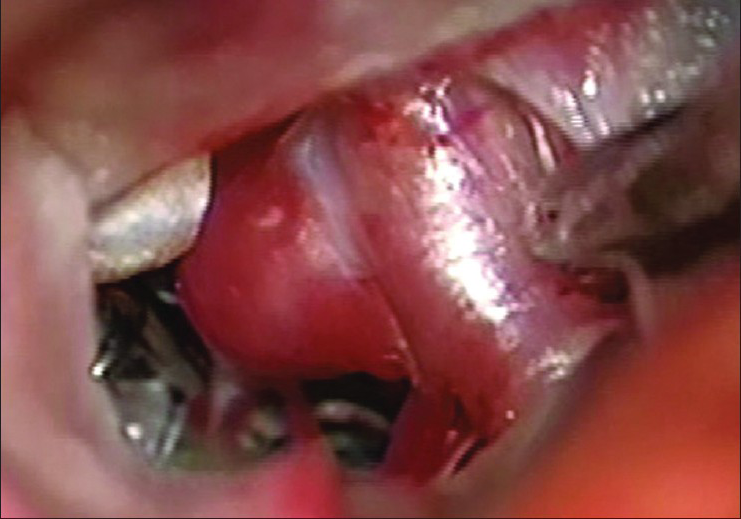
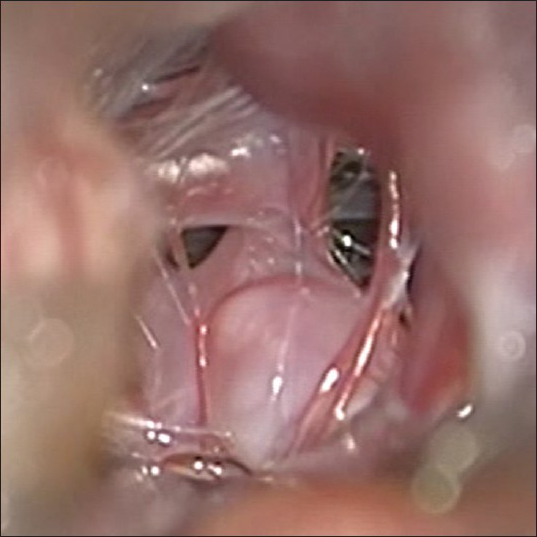
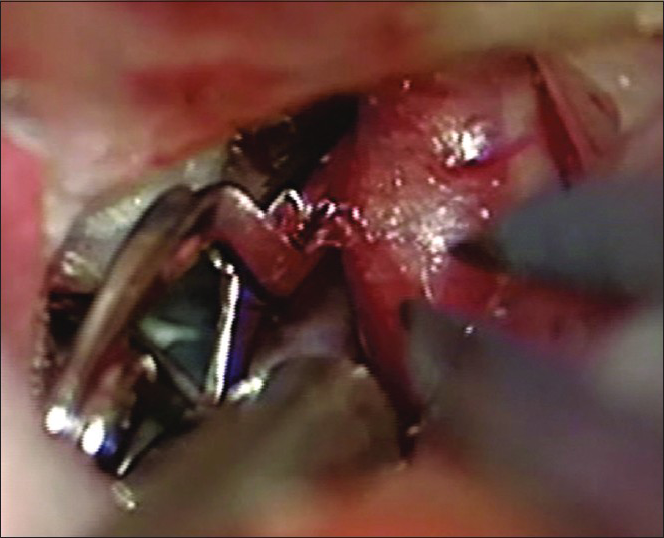
Under direct visual control, a pilot clip was placed on the PCA-P1 aneurysm and the aneurysm was shrunken with bipolar forceps. The attached perforating branches to the aneurysm dome were mobilized. For the placement of the final clip, a temporary clip was placed on the PCA and the aneurysm could be safely clipped using a straight (nontitanium) Yasargil mini-clip [
The ICA-PCoA aneurysm was dissected next. For the exposure of the whole affected ICA segment, arachnoid fibers between the proximal ICA and the optic nerve were cut. An anterior clinoidectomy was not necessary, but the overlying dura was coagulated down to obtain enough space. The whole ICA-PCoA aneurysm became visible. A temporary clip was placed on the ICA and the aneurysm was electro-thermally shrunken; the origin of PCoA became visible. Finally, the ICA-PCoA aneurysm could be occluded with a straight (nontitanium) Yasargil standard-clip [
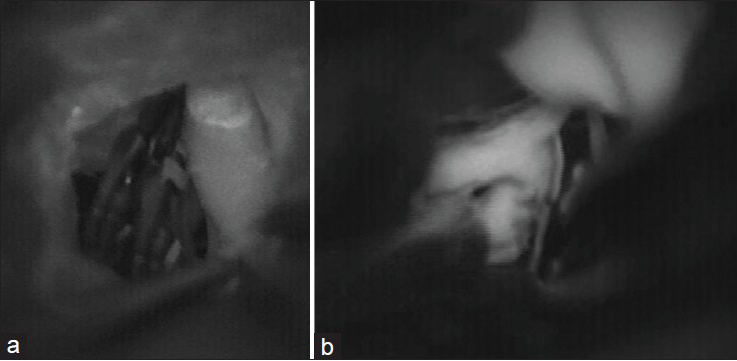
Intraoperative indocyanine green videoangiography
Postclip occlusion intraoperative indocyanine green (ICG) videoangiography provided real time images of the blood flow inside the ICA-C7 [
Operation time
The skin to skin operation time was 55 min. The following times for temporary clipping were used: 65 s of the PCA (PCA-P1 aneurysm) and 70 s of the ICA (ICA-PCoA aneurysm).
Postoperative course
The patient was woken just after the surgery. The postoperative CTA show a reconstructed angioarchitecture without occlusion of the parent vessels or neck remnants [
DISCUSSION
PCA aneurysms are often associated with anterior circulation aneurysms,[
Frontotemporal approaches, in different modifications, are suitable for the treatment of aneurysms located on the ipsilateral side, inside the circle of Willis.[
As a result, in our case, both aneurysms were occluded by microsurgical clipping, without constringence parent vessel lumen or other technical problems and no perioperative complications were observed. Due to modern microsurgical techniques, the lateral supraorbital approach has become a relatively safe procedure in experienced hands.
CONCLUSION
A safe microsurgical treatment of ipsilateral aneurysms inside the circle of Willis is feasible by the lateral supraorbital approach. Compared to endovascular treatment, the important perforating branches can be preserved under direct visual control. However, a critical preoperative decision-making process is needed based on various factors such as estimated vessel occlusion time, anatomical features of the aneurysm, the angioarchitecture and the microsurgical skills.
References
1. Dashti R, Laakso A, Niemelä M, Porras M, Celik O, Navratil O. Application of microscope integrated indocyanine green video-angiography during microneurosurgical treatment of intracranial aneurysms: A review. Acta Neurochir. 2010. 107: S107-9
2. Drake CG, Peerless SJ, Hernesniemi JA.editors. Surgery of Vertebrobasilar Aneurysms. London, Ontario Experience on 1767 Patients. Wien: Springer-Verlag; 1996. p.
3. Gerber C, Neil-Dwyer G, Barrie E. An alternative approach to aneurysms of the posterior cerebral artery. J Neurosurg. 1993. 32: 928-31
4. Goehre F, Jahromi BR, Hernesniemi J, Elsharkawy A, Kivisaari R, von und zu Fraunberg M. Characteristics of Posterior Cerebral Artery (PCA) Aneurysms: An Angiographic Analysis of 93 Aneurysms in 81 Patients. Neurosurgery. 2014. 75: 134-44
5. Goehre F, Kamiyama H, Kosaka A, Tsuboi T, Miyata S, Noda K. The anterior temporal approach for microsurgical thromboembolectomy of an acute proximal posterior cerebral artery occlusion. Neurosurgery. 2014. 10: S174-8
6. Elsharkawy A, Niemelä M, Lehečka M, Lehto H, Jarhomi BR, Goehre F. Focused opening of the sylvian fissure for microsurgical management of MCA aneurysms. Acta Neurochir. 2014. 156: 17-25
7. Hernesniemi J, Ishii K, Niemelä M, Smrcka M, Kivipelto L, Fujiki M. Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir. 2005. 94: S17-21
8. Heros RC, Lee SH. The combined pterional/anterior temporal approach for aneurysms of the upper basilar complex: Technical report. Neurosurgery. 1993. 33: 244-50
9. Honda M, Tsutsumi K, Yokoyama H, Yonekura M, Nagata I. Aneurysms of the posterior cerebral artery: Retrospective review of surgical treatment. Neurol Med Chir (Tokyo). 2004. 44: 164-8
10. Locksley H. Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. Section 5, part 1. Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the operative Study. J Neurosurg. 1966. 25: 219-39
11. Raabe A, Beck J, Gerlach R, Zimmermann M, Seifert V. Near-infrared indocyanine green video angiography: A new method for intraoperative assessment of vascular flow. Neurosurgery. 2003. 52: 132-9
12. Raabe A, Nakaji P, Beck J, Kim LJ, Hsu FP, Kamerman JD. Prospective evaluation of surgical microscope-integrated intraoperative near-infrared indocyanine green videoangiography during aneurysm surgery. J Neurosurg. 2005. 103: 982-9
13. Reisch R, Perneczky A, Filippi R. Surgical technique of the supraorbital key-hole craniotomy. Surg Neurol. 2003. 59: 223-7
14. Romani R, Lehecka M, Gaal E, Toninelli S, Celik O, Niemelä M. Lateral supraorbital approach applied to olfactory groove meningiomas: Experience with 66 consecutive patients. Neurosurgery. 2009. 65: 39-52
15. Sakata S, Fujii K, Matsushima T, Fujiwara S, Fukui M, Matsubara T. Aneurysm of the posterior cerebral artery: Report of eleven cases--surgical approaches and procedures. Neurosurgery. 1993. 32: 163-7
16. Salma A, Alkandari A, Sammet S, Ammirati M. Lateral supraorbital approach vs pterional approach: An anatomic qualitative and quantitative evaluation. Neurosurgery. 2011. 68: S364-72
17. Yasargil MG.editors. Microsurgical Anatomy of the Basal Cisterns and Vessels of the Brain, Diagnostic Studies, General Operative Techniques and Pathological Considerations of Intracranial Aneurysms. Stuttgart, Germany: Georg Thieme-Verlag; 1984. 1:
18. Yasargil MG.editors. Microsurgery. Clinical Considerations, Surgery of the Intracranial Aneurysms and Results. Stuttgart, Germany: Georg Thieme-Verlag; 1984. 2:
19. Yonekawa Y, Roth P, Fandino J, Landlot H. Aneurysms of the posterior cerebral artery and approach selection in their microsurgical treatment: Emphasis on their approaches: SAHEA and SCTTA. Acta Neurochir. 2011. 112: S85-92