- Department of Neurosurgery , Post Graduate Institute of Medical Education and Research, Dr. Ram Manohar Lohia Hospital, Baba Kharak Singh Marg, New Delhi, Delhi, India.
- Department of Pathology, Post Graduate Institute of Medical Education and Research, Dr. Ram Manohar Lohia Hospital, Baba Kharak Singh Marg, New Delhi, Delhi, India.
Correspondence Address:
Andrew Aranha
Department of Neurosurgery, Post Graduate Institute of Medical Education and Research, Dr. Ram Manohar Lohia Hospital, Baba Kharak Singh Marg, New Delhi, Delhi, India.
DOI:10.25259/SNI_474_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Andrew Aranha1, Pankaj Kumar1, Ajay Choudhary1, Purnima Paliwal2. Long segment cervicothoracic intramedullary dermoid with concomitant conal lesion – A case report. 29-Aug-2020;11:268
How to cite this URL: Andrew Aranha1, Pankaj Kumar1, Ajay Choudhary1, Purnima Paliwal2. Long segment cervicothoracic intramedullary dermoid with concomitant conal lesion – A case report. 29-Aug-2020;11:268. Available from: https://surgicalneurologyint.com/surgicalint-articles/10236/
Abstract
Background: Spinal dermoid cysts are benign tumors that result from congenital or acquired ectodermal inclusions. Long segment intramedullary involvement of the spinal cord is exceedingly rare, and there are only a handful of case reports found in the literature.
Case Description: A 30-year-old female presented with a 3-month history of myelopathy characterized by progressive quadriparesis and urinary incontinence. Magnetic resonance imaging revealed multifocal heterogeneous intramedullary masses extending from C2 to T4 and at T12–L1 with similar intensity lesions seen within the central cord from T5 to T11 level. Following tumor decompression, she showed significant improvement in neurological function 1 month later. The histopathological examination confirmed the diagnosis of a multifocal intramedullary dermoid cyst.
Conclusion: Partial surgical extirpation is a reasonable treatment for long segment intramedullary dermoid cysts, particularly when the tumor capsule is adherent to critical adjacent neural tissues.
Keywords: Dermoid cyst, Inclusion cyst, Intramedullary tumor, Spinal tumor
INTRODUCTION
Spinal dermoid cysts are benign tumors that result from congenital or acquired ectodermal inclusions.[
Here, we report a C2–L1 long segment cervical to conus medullaris intramedullary dermoid cyst along with satellite lesions.
CASE DESCRIPTION
History and examination
A 30-year-old female presented with a 3-month history of progressive quadriparesis and urinary incontinence. The neurological examination revealed atrophy of the intrinsic muscles of the hands, mild bilateral triceps weakness, and bilateral lower extremity weakness (4/5). Deep tendon reflexes were absent bilaterally at the triceps levels but hyperactive in both lower extremities with bilateral Babinski responses.
Imaging
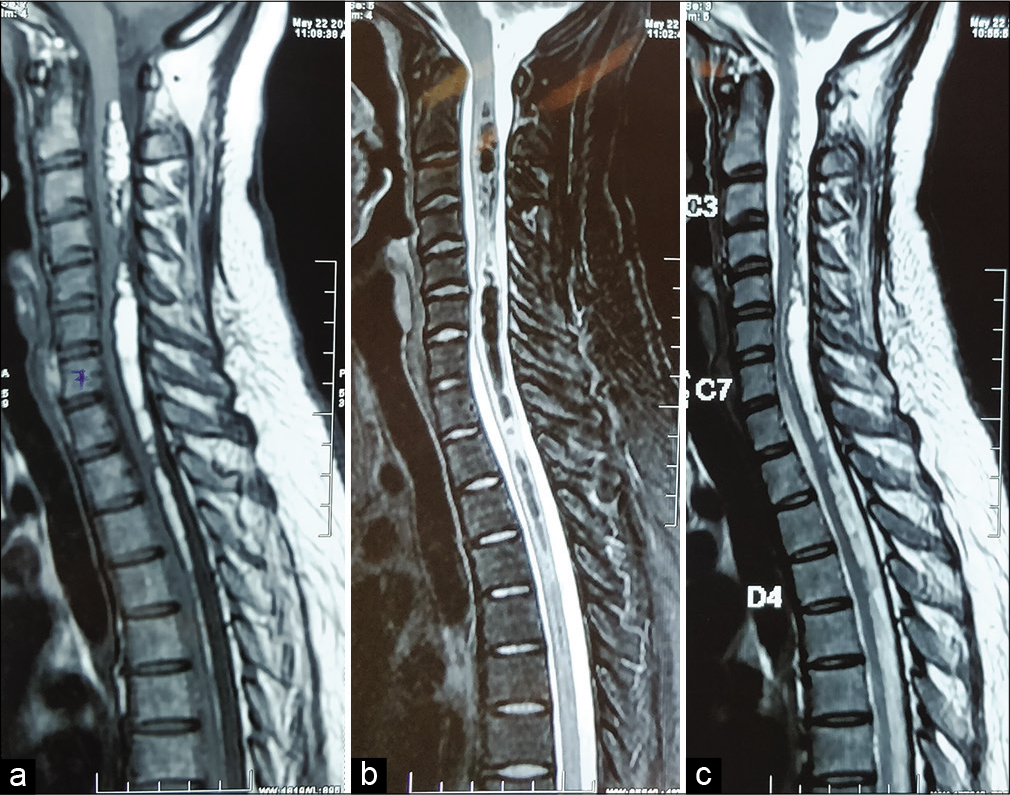
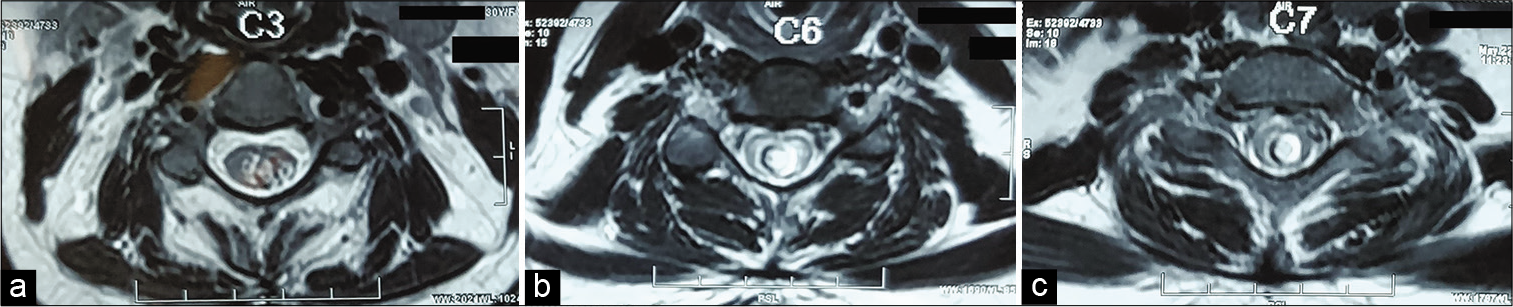
The MR revealed multifocal heterogeneous intramedullary masses extending from C2 to T4 and T12–L1; similar intensity lesions were seen within the central cord from T5 to T11 level [
Surgery
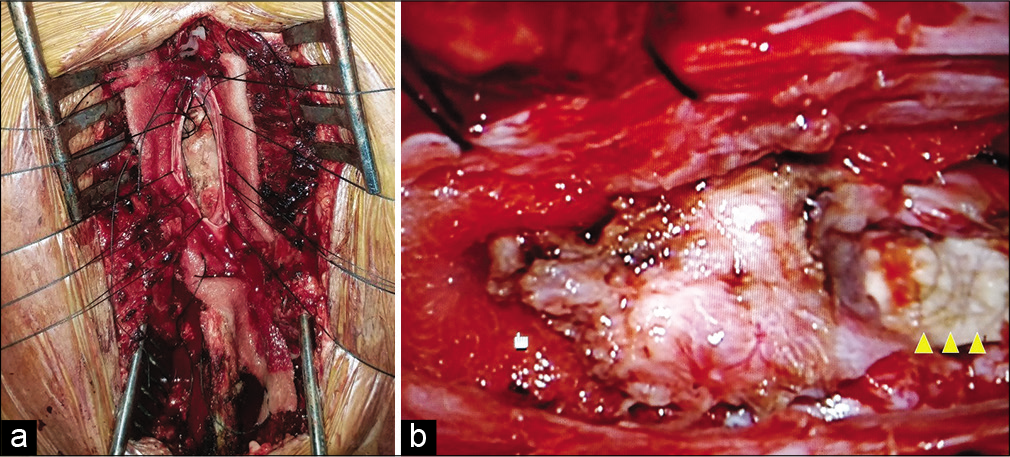
The patient underwent a C2–T4 and T12–L1 laminectomy utilizing intraoperative SSEP and MEP neuromonitoring. Once the dura mater was opened, an expanded spinal cord was immediately identified [
Postoperative course
The postoperative period was uneventful and the patient was discharged on postoperative day 6 requiring intermittent catheterization. Within 1 month, she reported improvement in all modalities. No further postoperative MR imaging was available.
Histopathology
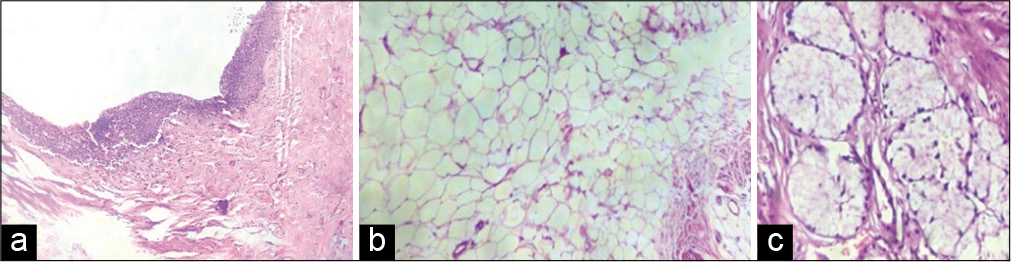
Biopsies from multiple sites were suggestive of a dermoid cyst showing: stratified squamous epithelium along with fibro-collagenous tissue with blood vessels, glial tissue, hair shafts, adipocytes, and areas of calcification [
DISCUSSION
Frequency and epidemiology
Dermoid tumors are rare lesions which constitute around 0.8–1.1% of intraspinal tumors.[
Imaging
Due to the varying amounts of soft tissue, fat, calcium, and hemorrhage, MRI typically demonstrates heterogeneous signal intensity lesions with the relatively high signal from fat (e.g., on MRI T1W images) making the identification of its lipid component more readily apparent.[
Rupture tendency for spinal dermoids
Spinal dermoid cysts are known to rupture, and their content can spread throughout the subarachnoid space and ventricular system.[
Prior reports of extensive intramedullary dermoid cysts
A holocord intramedullary dermoid has only been reported once in the literature involving a patient who refused surgery.[
Recommended treatment of intramedullary spinal dermoids
Given the indolent, benign nature of these tumors, asymptomatic lesions should ideally be managed conservatively.[
CONCLUSION
Intramedullary spinal dermoid cysts are rare tumors. Here, we report successful partial resection of intramedullary cord lesion extending from C2–L1 treated with skip laminectomies C2–T4 and T12–L1 laminectomies.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Calabro F, Capellini C, Jinkins JR. Rupture of spinal dermoid tumors with spread of fatty droplets in the cerebrospinal fluid pathways. Neuroradiology. 2000. 42: 572-9
2. Garg A, Gupta V, Gaikwad S, Deol P, Mishra NK, Suri A. Isolated central canal rupture of spinal dermoid: Report of two cases. Australas Radiol. 2003. 47: 194-7
3. Lunardi P, Missori P, Gagliardi FM, Fortuna A. Long-term results of the surgical treatment of spinal dermoid and epidermoid tumors. Neurosurgery. 1989. 25: 860-4
4. Ogden AT, Khandji AG, McCormick PC, Kaiser MG. Intramedullary inclusion cysts of the cervicothoracic junction. Report of two cases in adults and review of the literature. J Neurosurg Spine. 2007. 7: 236-42
5. Sharma N, Chandra T, Sharma A, Bajaj M, Kundu R. Long-segment intramedullary spinal dermoid. Indian J Radiol Imaging. 2009. 19: 148-50
6. Shukla K, Bhaskar S, Garg M, Bharti JN, Yadav A, Jha DK. Long-segment intramedullary spinal dermoid. Interdiscip Neurosurg. 2020. 20: 100648
7. Tassigny D, Fomekong E, Koerts G, Raftopoulos C. Intramedullary holocord abscess secondary to infected dermoid cyst. Acta Neurochir (Wien). 2018. 160: 209-12