- Department of Orthopaedics and Spine Surgery, Bharat Ratna Dr. Babasaheb Ambedkar Memorial Hospital, Byculla East,
- ASSI Fellow, Lilavati Hospital and Research Centre, Bandra,
- Department of Orthopaedics, Seth GSMC and KEMH, Parel, Mumbai, Maharashtra, India.
Correspondence Address:
Harsh Agrawal, Department of Orthopaedics and Spine Surgery, Bharat Ratna Dr. Babasaheb Ambedkar Memorial Hospital, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_238_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Harsh Agrawal1, Ayush Sharma1, Vijay Singh1, Atif Naseem1, Manojkumar Gaddikeri2, Ankit Amin3. Long-segment fixation versus short-segment fixation with instrumentation of index vertebra for thoracolumbar fractures. 03-Jun-2022;13:233
How to cite this URL: Harsh Agrawal1, Ayush Sharma1, Vijay Singh1, Atif Naseem1, Manojkumar Gaddikeri2, Ankit Amin3. Long-segment fixation versus short-segment fixation with instrumentation of index vertebra for thoracolumbar fractures. 03-Jun-2022;13:233. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11634
Abstract
Background: We assessed and analyzed the clinical, perioperative, functional, and radiological outcomes of long- versus short-segment (SS) fixation of thoracolumbar spine fractures that included the index vertebra.
Methods: We retrospectively evaluated 119 patients with thoracolumbar spine fractures (i.e., using AO classification system). The patient was followed up for a minimum of 1 year at which time the angles of correction were measured on lateral X-rays (i.e., using Cobb’s method). Neurological grading employed the Frankel’s grading system. Operative time, perioperative blood loss, and time to mobilization were also analyzed.
Results: After 1 year, the loss of kyphosis was not significantly different between the two groups. Although there were no statistical differences in terms, regarding neurological outcomes, time to mobilization, or duration of hospitalization, the operative times and perioperative blood loss were significantly reduced in patients undergoing SS fixation.
Conclusion: We determined the efficacy of SS fixation for thoracolumbar fractures including the index vertebra.
Keywords: Fixation, Pedicle screws, Spine trauma, Thoracolumbar fracture, Treatment
INTRODUCTION
The goals for treating thoracolumbar fractures include; the restoration of vertebral column stability, obtaining adequate decompression of the spinal canal, and early mobilization of the patient. The classical “long-segment” constructs include instrumenting two or three levels above and below the injured level,[
MATERIALS AND METHODS
We evaluated 119 adults who sustained single level posttraumatic thoracolumbar fracture/ fracture dislocation. The CT scans had to document that at least one side of the fractured vertebra/pedicle was intact. Where feasible, patients also underwent MRI scans to evaluate spinal cord compression, the status of the anterior/posterior longitudinal ligaments, and the intervertebral disk.
Clinical data
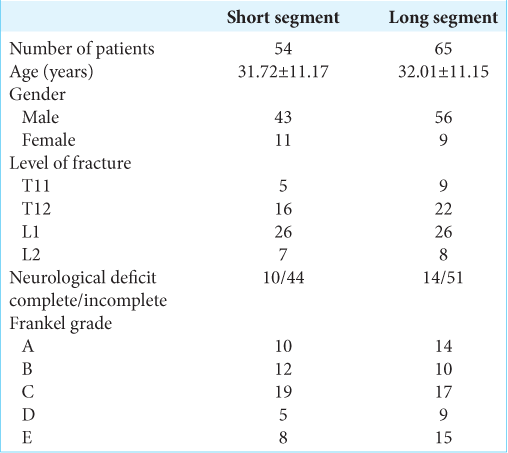
Multiple baseline parameters were also recorded [
Fracture patterns using AO spine injury classification systems
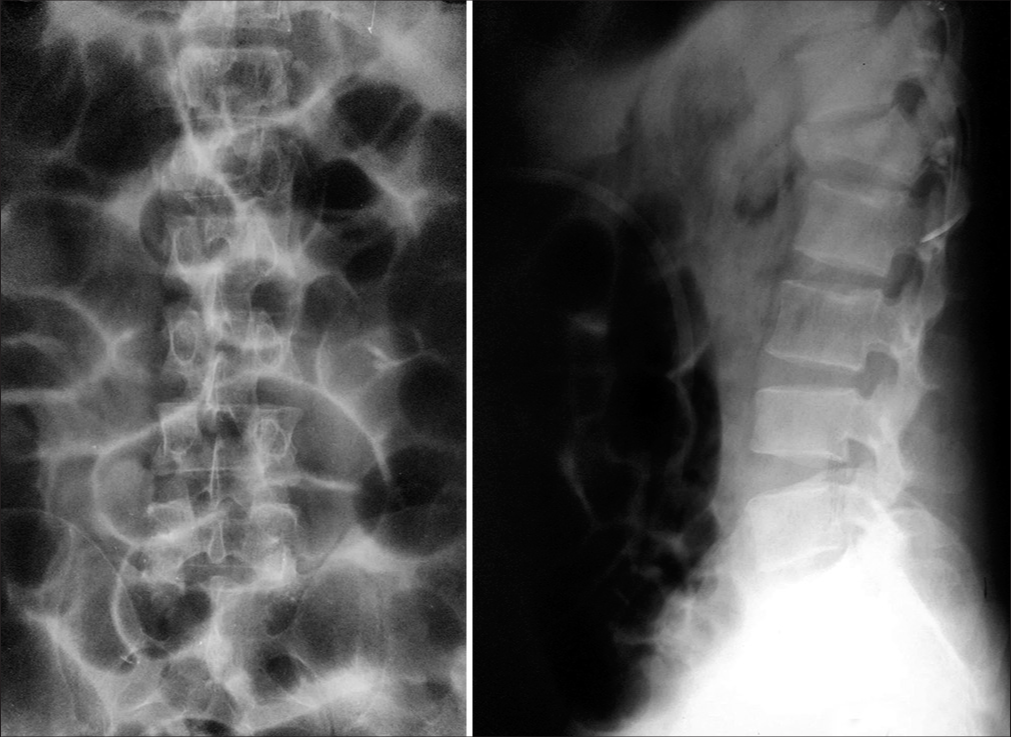
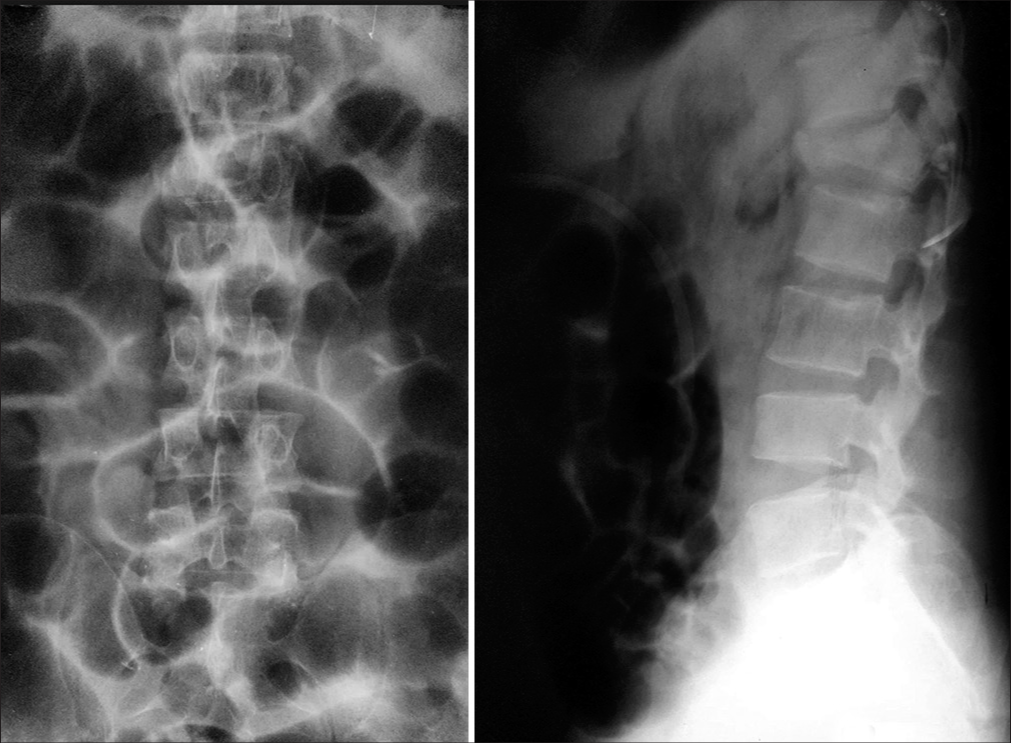
We used the AO spine injury classification systems for evaluating fractures. Patients underwent either SS fixation or long-segment fixation at the discretion of the surgeon (i.e., not randomized). A plain radiographs were evaluated preoperatively and postoperatively for kyphotic angulation using the Cobb method.[
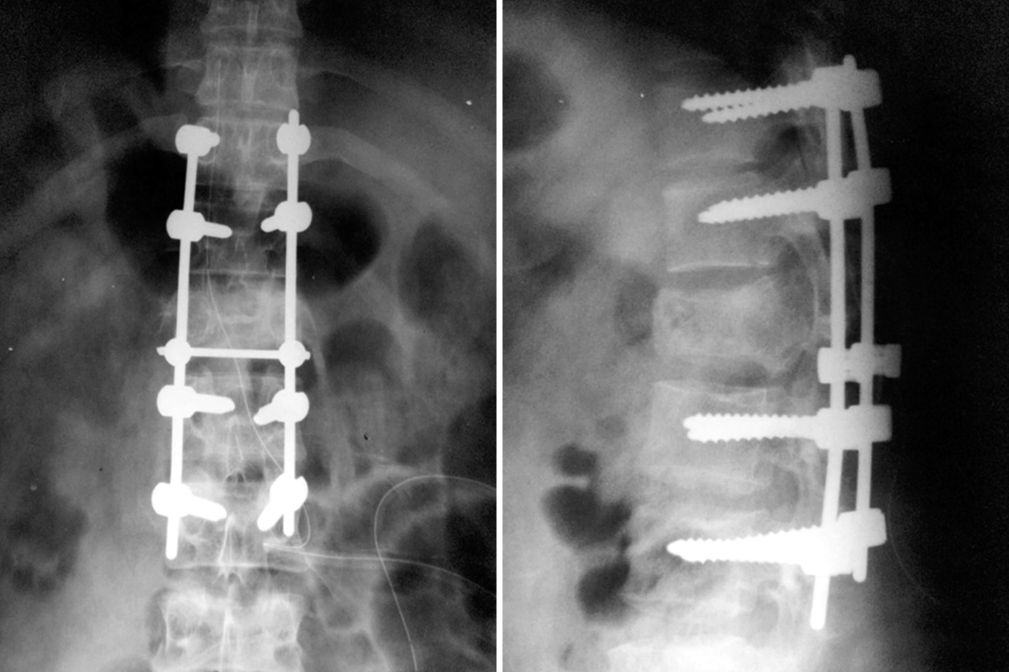
Short- and long-segment fixation
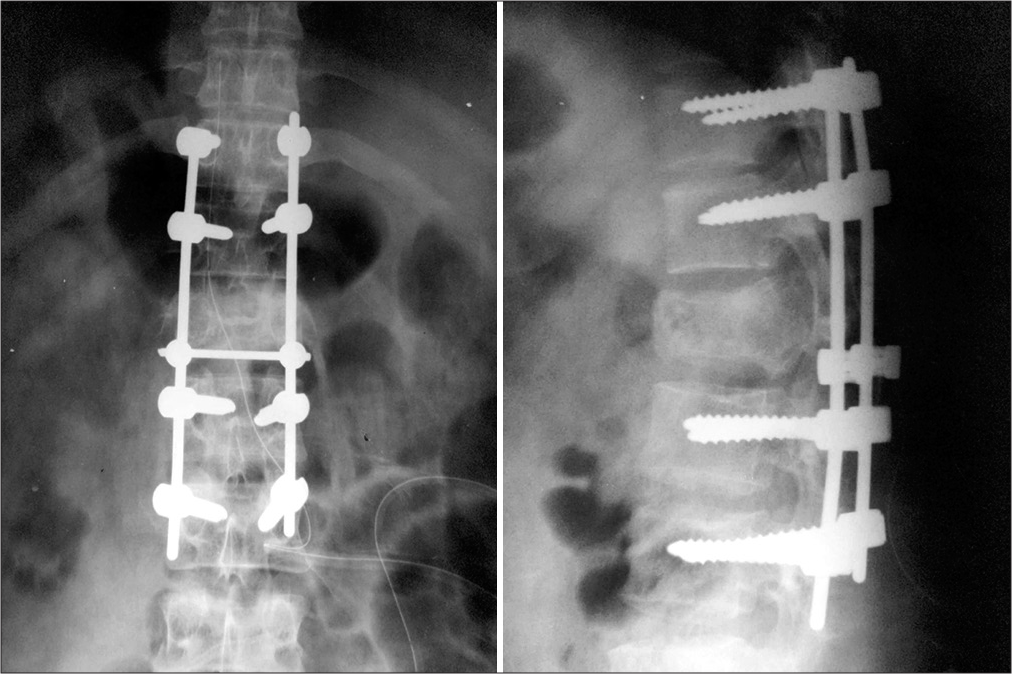
SS fixations included pedicle screws placed one level above and one level below the fracture site, pedicle screws inserted into the index vertebra, followed by rod application (i.e., contoured rods using ligamentotaxis to correct kyphosis and perform lordotic distraction) [
RESULTS
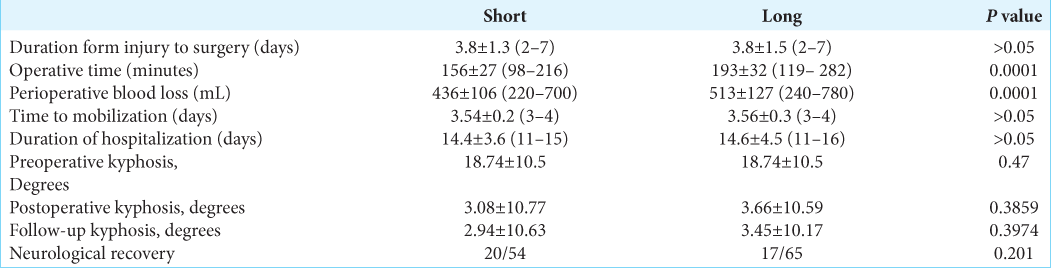
Improvement was based on achieving a postoperative Frankel Grade C or above, and comparable neurological recoveries were noted in both groups. Although there were no statistical difference between the two groups in terms of duration from injury to surgery, time to mobilization, and duration of hospitalization, operative time and perioperative blood loss were significantly reduced for SS fusions (P < 0.0001) [
Postoperative complications
Complications were encountered in 20 patients. Eight dural tears were managed with Prolene 5-0 sutures reinforced with Fat; all dural leak repairs proved successful.[
DISCUSSION
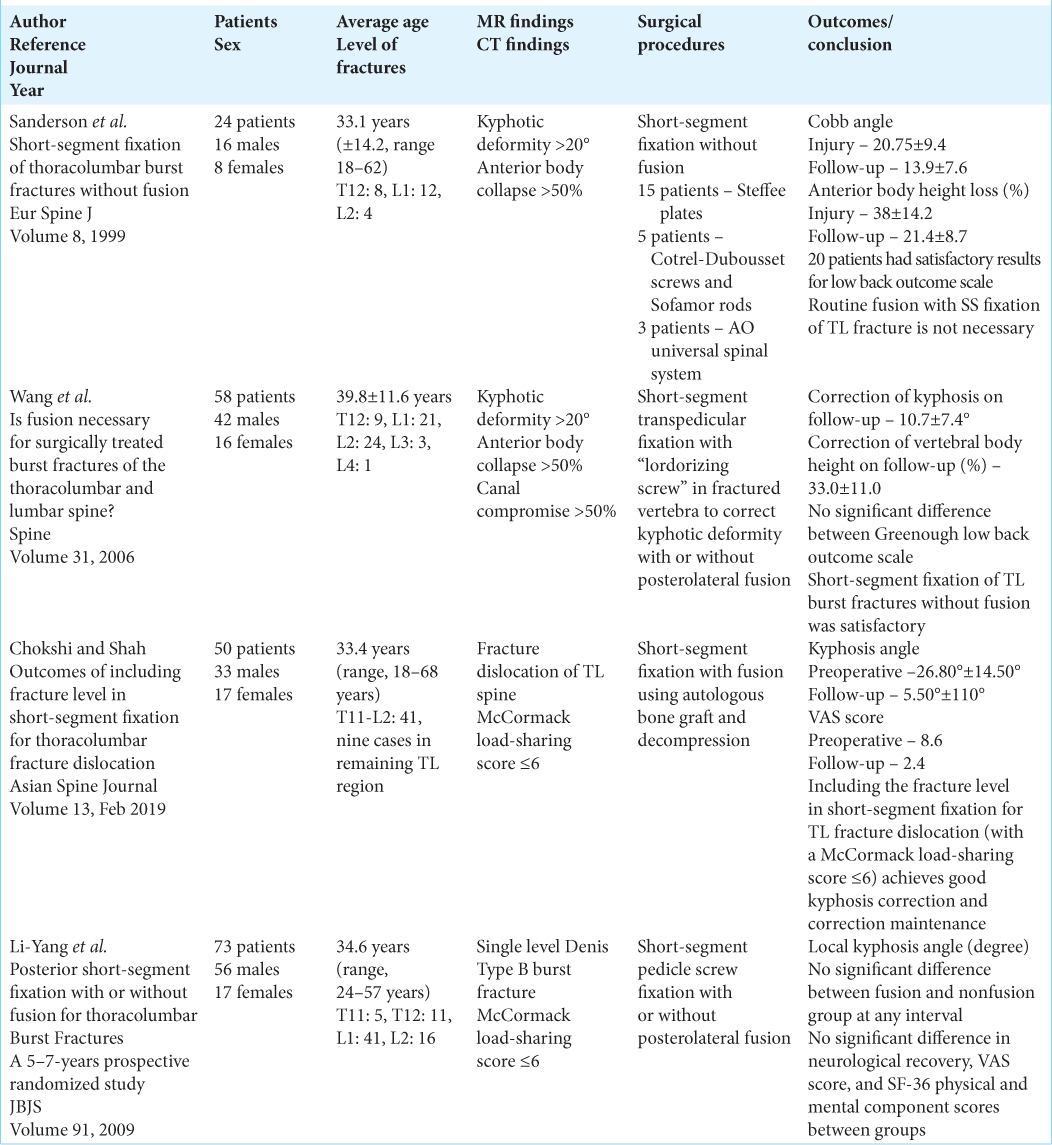
Although many studies have documented the efficacy of long-segment fixation for the treatment of thoracolumbar fractures, SS fusions have increasingly proved as effective [
CONCLUSION
We concluded that SS fixation was as effective as long-segment fusion for treating thoracolumbar fractures.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Chokshi JJ, Shah M. Outcomes of including fracture level in short-segment fixation for thoracolumbar fracture dislocation. Asian Spine J. 2019. 13: 56-60
2. Cobb JR. Outline for the study of scoliosis. AAOS Instr Course Lect. 1984. 5: 261-75
3. Dick W, Kluger P, Magerl F, Woersdörfer O, Zäch G. A new device for internal fixation of thoracolumbar and lumbar spine fractures: The “fixateur interne”. Paraplegia. 1985. 23: 225-32
4. Epstein NE. A review article on the diagnosis and treatment of cerebrospinal fluid fistulas and dural tears occurring during spinal surgery. Surg Neurol Int. 2013. 4: S301-17
5. Li-Yang D, Lei-Sheng J, Sheng-Dan J. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. A five to seven-year prospective randomized study. J Bone Joint Surg Am. 2009. 91: 1033-41
6. Sanderson PL, Fraser RD, Hall DJ, Cain CM, Osti OL, Potter GR. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999. 8: 495-500
7. Sasso RC, Cotler HB. Posterior instrumentation and fusion for unstable fractures and fracture-dislocations of the thoracic and lumbar spine. A comparative study of three fixation devices in 70 patients. Spine (Phila Pa 1976). 1993. 18: 450-60
8. Tasdemiroglu E, Tibbs PA. Long-term follow-up results of thoracolumbar fractures after posterior instrumentation. Spine (Phila Pa 1976). 1995. 20: 1704-8
9. Wang ST, Ma HL, Liu CL, Yu WK, Chang MC, Chen TH. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine? A prospective, randomized study. Spine (Phila Pa 1976). 2006. 31: 2646-52