- Department of Neurosurgery, Shinsuma General Hospital,
- Department of Neurosurgery, Kobe University Graduate School of Medicine, Kobe,
Correspondence Address:
Hirotomo Tanaka, Department of Neurosurgery, Shinsuma General Hospital, Kobe, Japan.
DOI:10.25259/SNI_471_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hirotomo Tanaka1, Yoshiyuki Takaishi1, Shinichi Miura2, Takashi Mizowaki1, Takeshi Kondoh1, Takashi Sasayama2. Long-term recurrence after surgery for schwannoma of the cauda equina. 23-Jun-2022;13:272
How to cite this URL: Hirotomo Tanaka1, Yoshiyuki Takaishi1, Shinichi Miura2, Takashi Mizowaki1, Takeshi Kondoh1, Takashi Sasayama2. Long-term recurrence after surgery for schwannoma of the cauda equina. 23-Jun-2022;13:272. Available from: https://surgicalneurologyint.com/surgicalint-articles/11679/
Abstract
Background: Cauda equina tumors are rare primary spinal tumors. Histologically, the most common tumor arising from the cauda equina is a schwannoma. However, little is known about the long-term postoperative outcomes of cauda equina schwannoma. Here, we reviewed the median-to-long-term postoperative outcomes of eight of our own patients with schwannomas of the cauda equina.
Methods: Between 2007 and 2020, we, retrospectively, reviewed eight patients with cauda equina schwannomas (CESs) undergoing nine operations at our institution. There were five males and three females averaging 56.5 years of age who were followed for over 40 postoperative months. The study included assessment of the following variables: the modified McCormick scale, tumor size, location, extent of resection, treatment of the tumor involving nerve roots, and postoperative observational follow-up.
Results: Gross-total resection was achieved in all eight patients; none received adjuvant therapy. The involved nerve roots were completely sacrificed in seven patients and partially resected in one. During a median follow-up of 108 months, only one patient sustained a tumor recurrence 164 months following the index surgery.
Conclusion: CESs may recur more than 10 years after the original surgery. Radical resection of the tumor, including complete removal of the involved nerve root during the index surgery, and long-term postoperative follow-up is, therefore, essential.
Keywords: Cauda equina schwannoma, Median-to-long-term outcome, Recurrence, Surgery
INTRODUCTION
Cauda equina schwannomas (CESs) are rare benign tumors that typically precipitate cauda equina syndromes characterized by low back pain, lower extremity sensory/motor disturbances, gait imbalance, and/or bladder/bowel dysfunction. Large or symptomatic CES often warrant surgical resection, but currently, there is no clear role for adjuvant therapy.[
MATERIALS AND METHODS
From 2007 to 2012, we, retrospectively, evaluated eight patients who originally presented with cauda equina syndrome due to schwannomas (CES). Our analysis specifically included assessment of their median-to-long-term postoperative incidence and time to recurrence. All tumors were the WHO grade 1, and all were followed for >40 months after the index surgery. We evaluated the following variables: preoperative neurologic/radiologic findings, modified McCormick scales, extent of resection of the tumor and the tumor-involved nerve root, the use of intraoperative electromyography (i.e., last three cases), and postoperative observational time. Surgery included microsurgical laminotomies (i.e., for the first five cases) and laminectomies (i.e., for the last three cases). All patients underwent postoperative lumbar magnetic resonance imaging (MRI) repeated every 6–12 months over a median follow-up duration of 108 months.
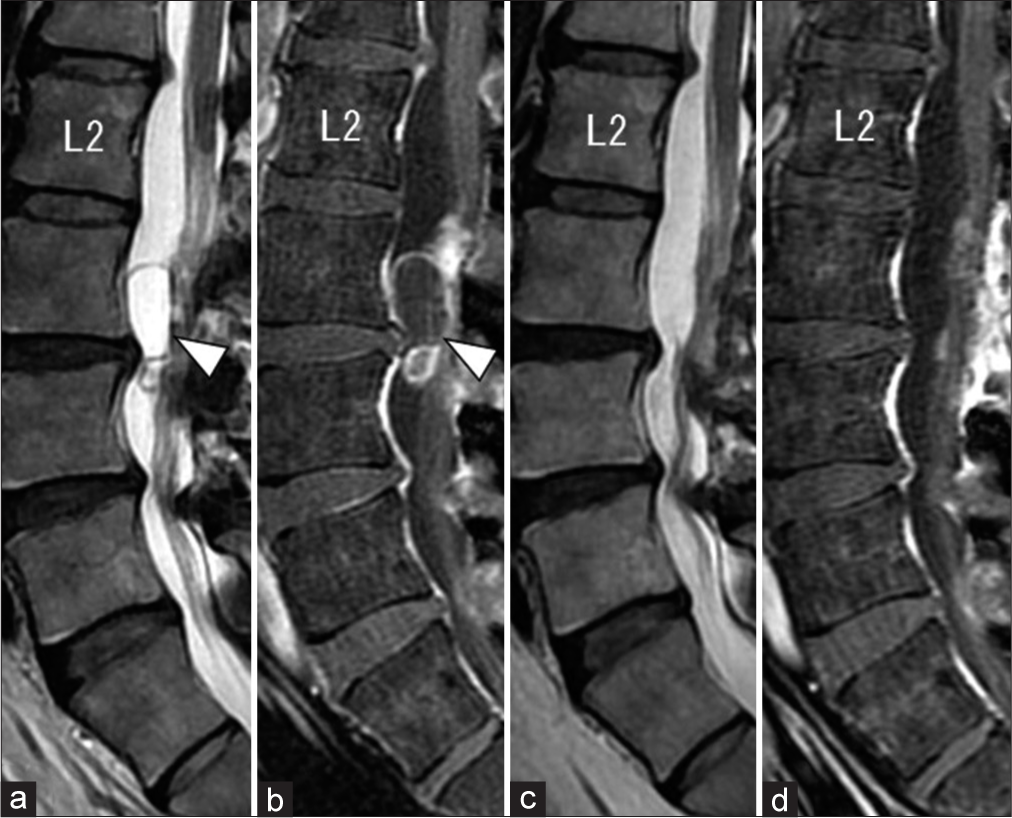
Preoperative data in eight cases
Preoperative symptoms in all eight patients included: low back, buttock, and lower extremity pain, and/or numbness [
RESULTS
Although gross-total resection (GTR) was accomplished in eight patients, the tumor-involved nerve roots were fully resected in seven, but just partially removed in one. Postoperatively, two patients exhibited transient and mild motor weakness of the lower extremities. After a median postoperative follow-up time of 108 months for all eight patients, only one patient experienced a tumor recurrence at 164 postoperative months.
Single case report
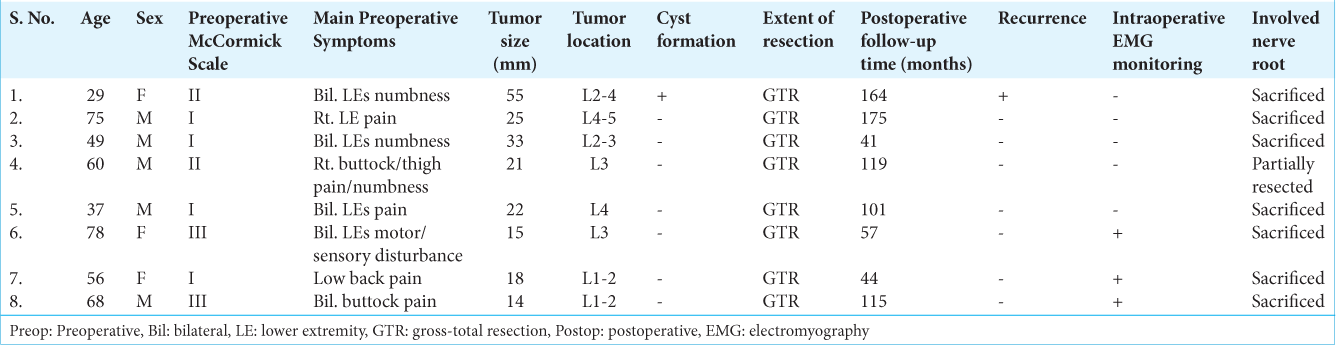
A 29-year-old woman with low back pain and numbness of both lower extremities had an original MRI demonstrating a cauda equina tumor at the L2–L4 levels measuring 55 mm in diameter with rim-enhancing cyst [
Figure 1:
The mid-sagittal view of lumbar MR images before (a and b) and after (c and d) the first surgery. Preoperative T2-weighted (a) and Gd-enhanced T1-weighted (b) images demonstrating intradural cystic tumors at the L2-4 level (white arrowhead). Postoperative T2-weighted (a) and Gd-enhanced T1-weighted (b) images showing no residual tumor.
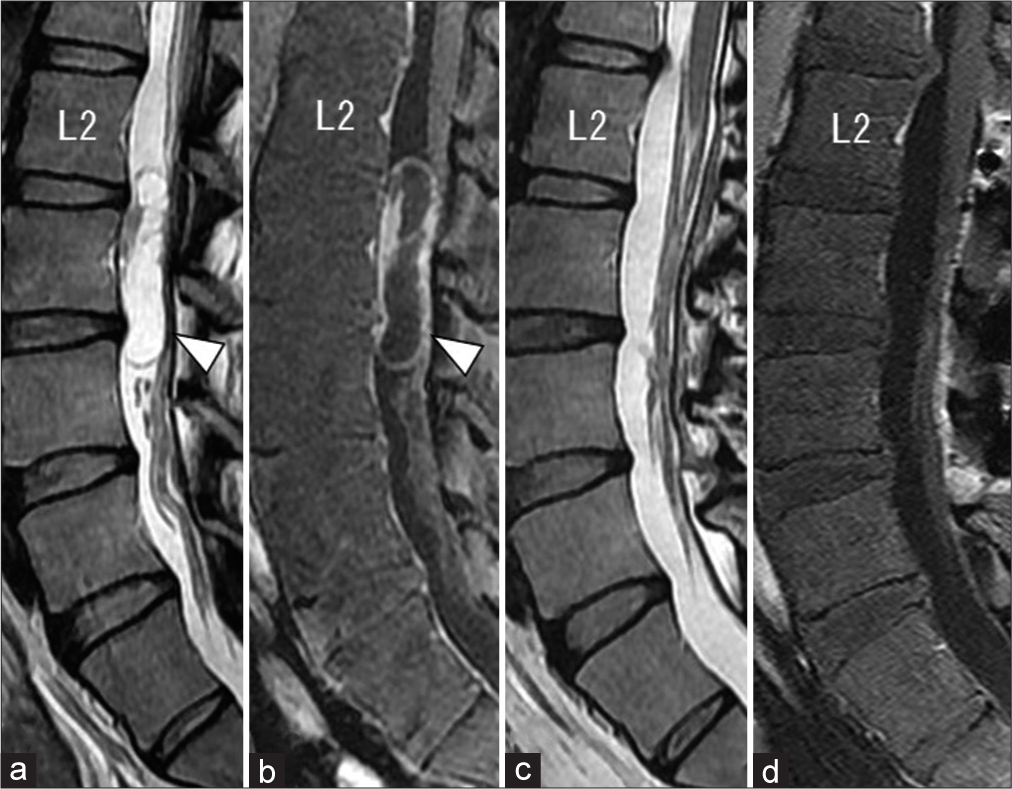
Figure 2:
The mid-sagittal view of lumbar MR images before (a, b) and after (c, d) the second surgery. T2-weighted (a) and Gd-enhanced T1-weighted (b) images showing tumor recurrence at the levels of L3-4 (white arrowhead). Postoperative T2-weighted (c) and Gd-enhanced T1-weighted (d) images showing the total removal of the recurrent tumor.
DISCUSSION
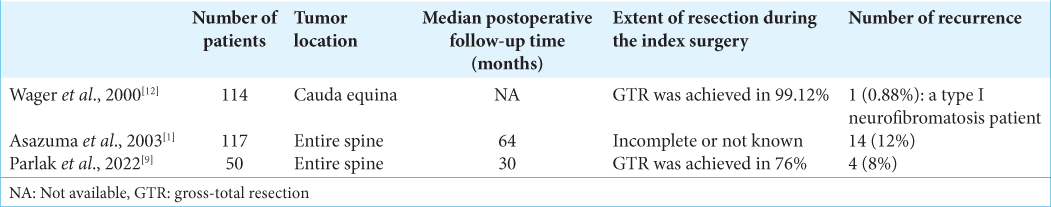
Postoperative delayed recurrence for CES
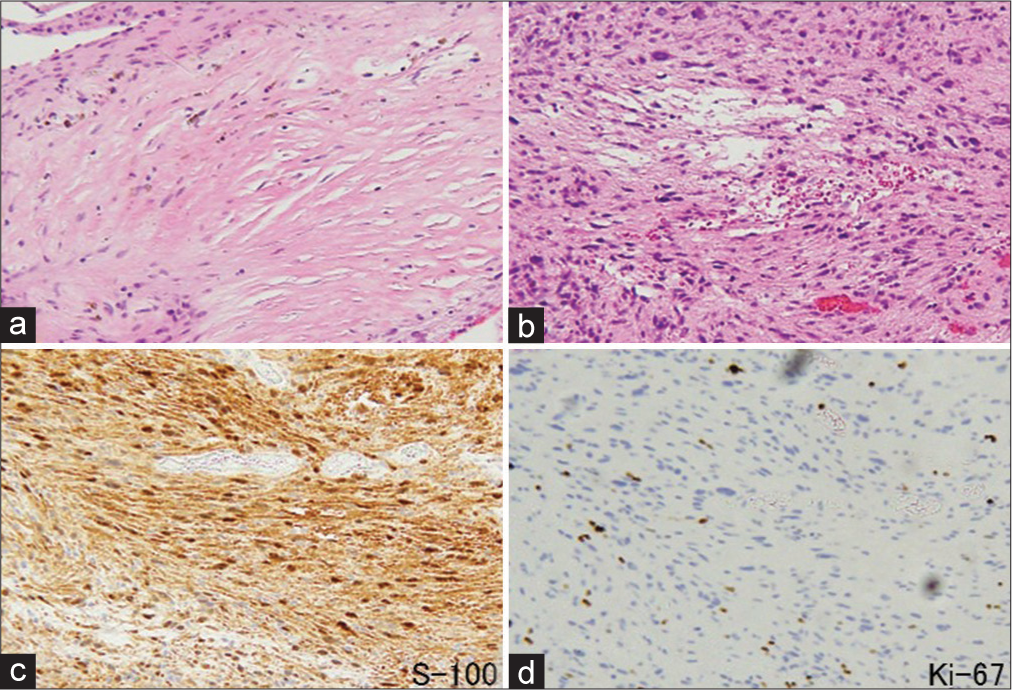
Spinal schwannomas, accounting for 31–49% of cauda equina tumors in adults, are the third most common primary tumor of the spinal cord, meninges, and cauda equina.[
Cause of recurrent CES
Although there are likely several causes for recurrent CES, the most likely factors include: relatively large tumor size, adherence to surrounding nerves resulting in initial partial resections (i.e., attempted preservation of the tumor-involved nerve root thus leaving behind a nidus for recurrence), and cyst formation increasing the risk of “tumor spillage” during the index surgical resection. Lee et al. reported that triggered electromyogram and neurophysiological monitoring provide ideal intraoperative data for deciding whether or not to sacrifice the rootlet.[
Adjunctive therapy
There are a few isolated reports regarding the potential efficacy of stereotactic radiosurgery (SRS) for benign spinal tumors.[
CONCLUSION
We present a case series of eight patients with CES, one of whom experienced recurrence more than 13 years after surgery. This finding should suggest that longer-term follow-up for over 10 years may be necessary to detect recurrent CES.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asazuma T, Toyama Y, Watanabe M, Suzuki N, Fujimura Y, Hirabayashi K. Clinical features associated with recurrence of tumours of the spinal cord and cauda equina. Spinal Cord. 2003. 41: 85-9
2. Chin AL, Fujimoto D, Kumar KA, Tupper L, Mansour S, Chang SD. Long-term update of stereotactic radiosurgery for benign spinal tumors. Neurosurgery. 2019. 85: 708-16
3. Das S, John KD, Urevick AJ, Yusuf MB, Wang D, Ugiliweneza B. Tumors in the cauda equina: A SEER analysis of tumor types and predictors of outcome. J Clin Neurosci. 2020. 81: 227-33
4. Dodd RL, Ryu MR, Kamnerdsupaphon P, Gibbs IC, Chang SD, Adler JR. CyberKnife radiosurgery for benign intradural extramedullary spinal tumors. Neurosurgery. 2006. 58: 674-85
5. Engelhard HH, Villano JL, Porter KR, Stewart AK, Barua M, Barker FG. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equina. J Neurosurg Spine. 2010. 13: 67-77
6. Gerszten PC, Burton SA, Ozhasoglu C, McCue KJ, Quinn AE. Radiosurgery for benign intradural spinal tumors. Neurosurgery. 2008. 62: 887-95
7. Gerszten PC, Quader M, Novotny J, Flickinger JC. Radiosurgery for benign tumors of the spine: Clinical experience and current trends. Technol Cancer Res Treat. 2012. 11: 133-9
8. Lee S, Cho DC, Rhim SC, Lee BJ, Hong SH, Koo YS. Intraoperative monitoring for Cauda Equina tumors: Surgical outcomes and neurophysiological data accrued over 10 years. Neurospine. 2021. 18: 281-9
9. Parlak A, Oppong MD, Jabbarli R, Gembruch O, Dammann P, Wrede K. Do Tumour size, type and localisation affect resection rate in patients with spinal schwannoma?. Medicina (Kaunas). 2022. 58: 357
10. Perez-Pinto F, Abaunza-Camacho JF, Vergara-Garcia D, Benavides C, Riveros WM, Laverde L. Management of recurrent schwannoma of the cauda equina: A case report. Surg Neurol Int. 2021. 12: 312
11. Shin DW, Sohn MJ, Kim HS, Lee DJ, Jeon SR, Hwang YJ. Clinical analysis of spinal stereotactic radiosurgery in the treatment of neurogenic tumors. J Neurosurg Spine. 2015. 23: 429-37
12. Wager M, Lapierre F, Blanc JL, Listrat A, Bataille B. Cauda equina tumors: A French multicenter retrospective review of 231 adult cases and review of the literature. Neurosurg Rev. 2000. 23: 119-29