- Department of Spine Surgery, Baby Memorial Hospital, IG road, Calicut, Kerala, India.
Correspondence Address:
Suresh S. Pillai, Department of Spine Surgery, Baby Memorial Hospital, IG road, Calicut, Kerala, India.
DOI:10.25259/SNI_573_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Suresh S. Pillai. Long-term survival following resection of extracompartmental osteosarcoma of the spine – A case report and literature review. 02-Nov-2021;12:545
How to cite this URL: Suresh S. Pillai. Long-term survival following resection of extracompartmental osteosarcoma of the spine – A case report and literature review. 02-Nov-2021;12:545. Available from: https://surgicalneurologyint.com/surgicalint-articles/11213/
Abstract
Background: Osteosarcoma, representing 3% of sarcomas, rarely involves the axial skeleton. The overall 5-year survival is just 18%. Here, we present a 15-year-old female with an extracompartmental osteosarcoma, who following radical spine surgery, chemotherapy, and intensive radiotherapy remained disease-free 15.5 years later.
Case Description: A 15-year-old female presented with an acute right lower extremity monoparesis and T4 relative sensory level attributed to a T4 extracompartmental Osteosarcoma. Following circumferential spine surgery, chemotherapy, and radiotherapy, her tumor did not recur over the 15.5-year follow-up period.
Conclusion: Osteosarcoma rarely presents focally in the spine. When it originates in the spine, there are typically few long-term survivors. Here, we report a 15-year-old female who presented with an acute monoparesis attributed to an extracompartmental T4 spinal osteosarcoma. Following circumferential tumor resection, adjuvant chemotherapy, and radiotherapy, the patient remains disease-free 15.5 years later.
Keywords: Extracompartmental, Osteosarcoma, Paraplegia, Survivor, Thoracic spine
INTRODUCTION
Osteosarcoma, which occurs with a frequency of 5 cases per million population, is a high-grade malignancy, typically found in children. When patients present with spinal lesions, (only 3–5% of the time), they usually already have pulmonary metastases. Here, we report a 15-year-old female who presented with a right lower extremity monoparesis, attributed to a D4 osteosarcoma, with attendant extracompartmental spread. Following circumferential spine surgery, chemotherapy, and radiotherapy, the patient remains disease-free 15.5 years later.
CASE REPORT
A 15-year-old female acutely presented with the right lower extremity paresis (2/5), a D4 sensory level, bilateral lower extremity hyperreflexia/bilateral Babinski responses, and urinary incontinence. Laboratory studies were unremarkable.
Diagnostic studies
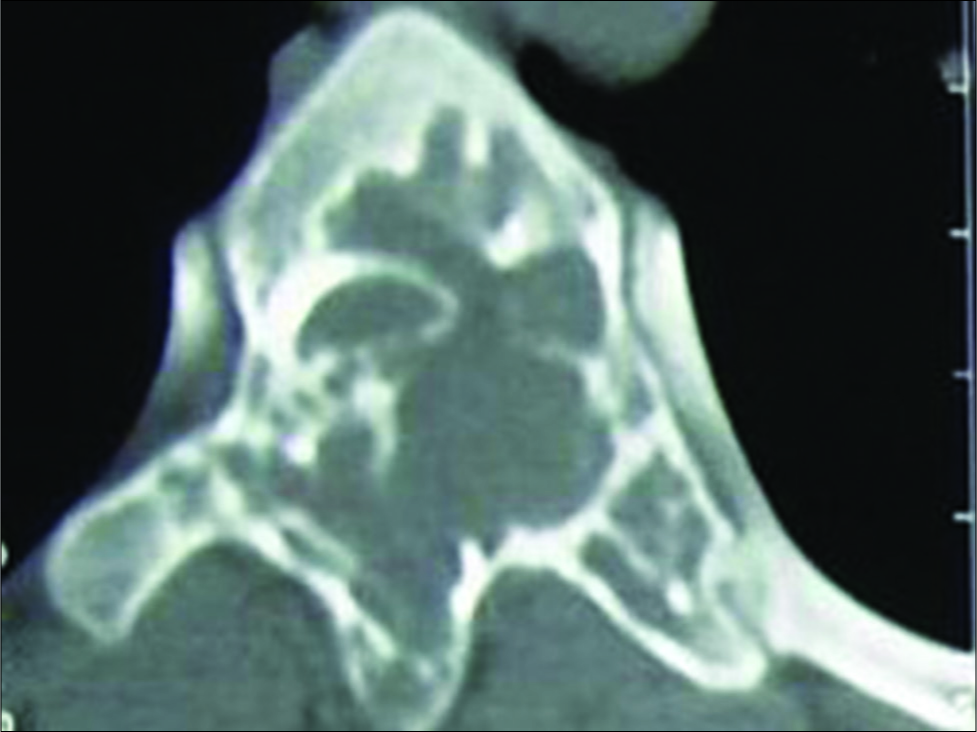
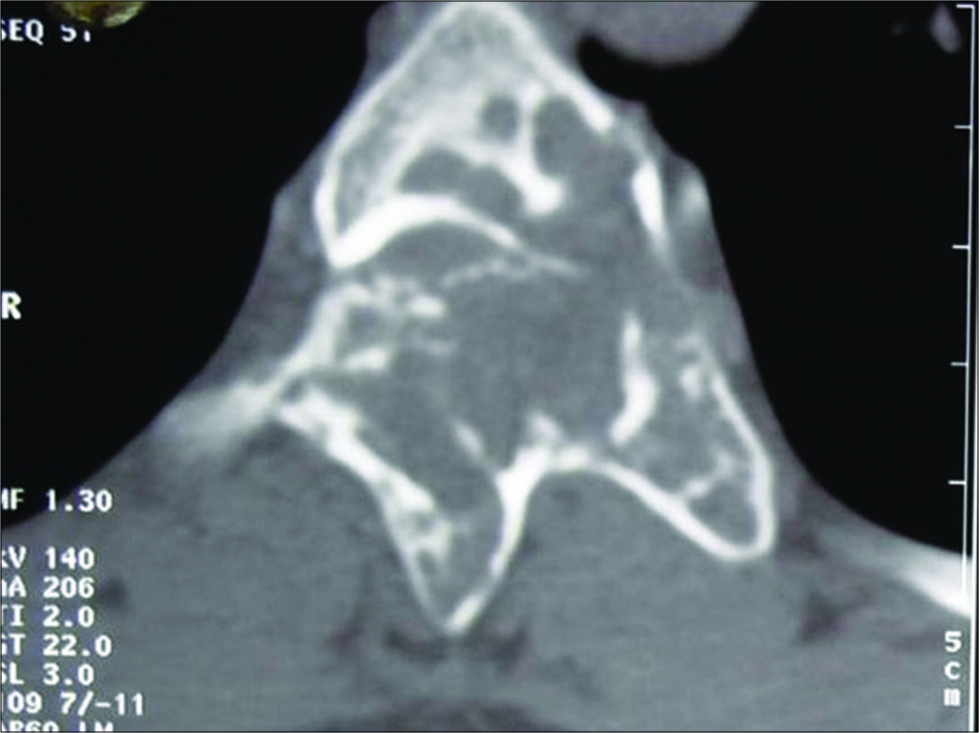
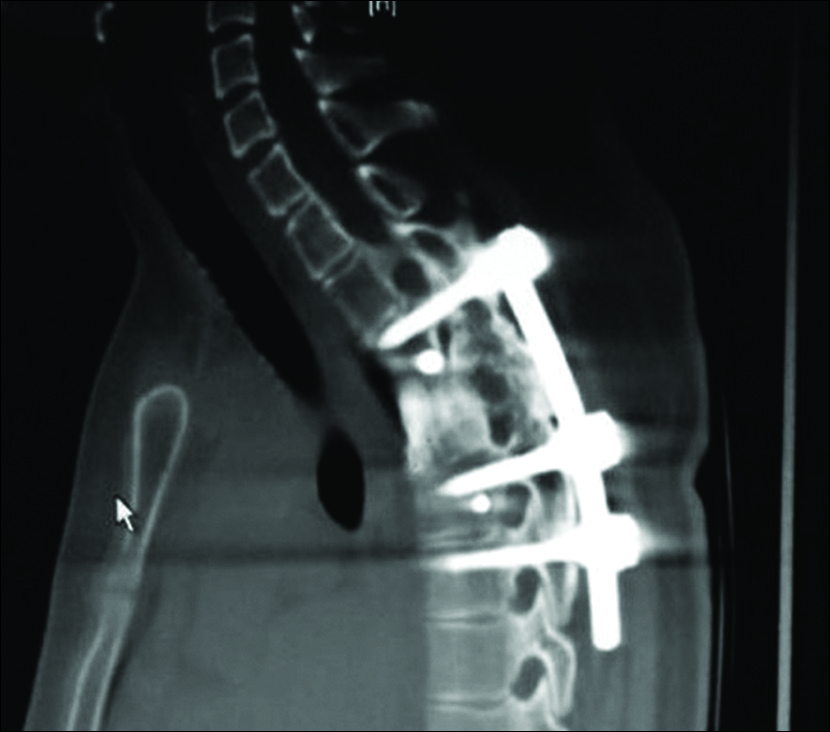
CT findings
The thoracic CT showed an expansile destructive lesion involving the left lamina of D2-5 and left pedicle/spinous process of D4. The accompanying ventral amorphous calcific mass extended from D2-5 level. This resulted in circumferential cord compression and paraparesis [
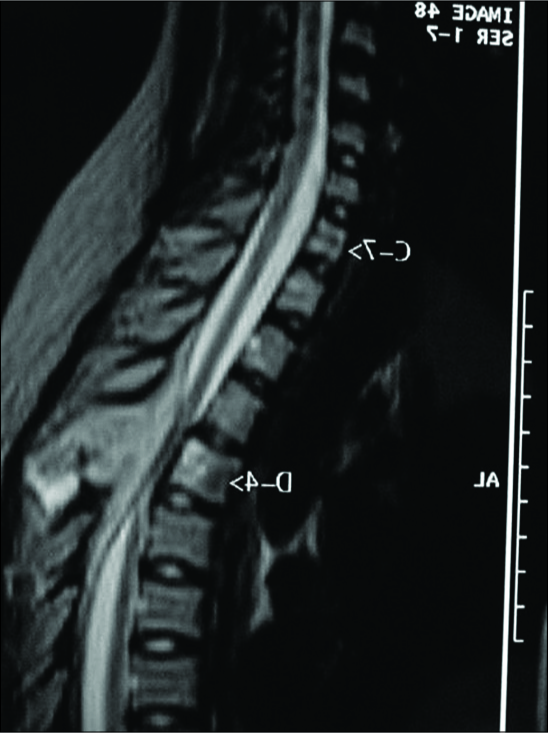
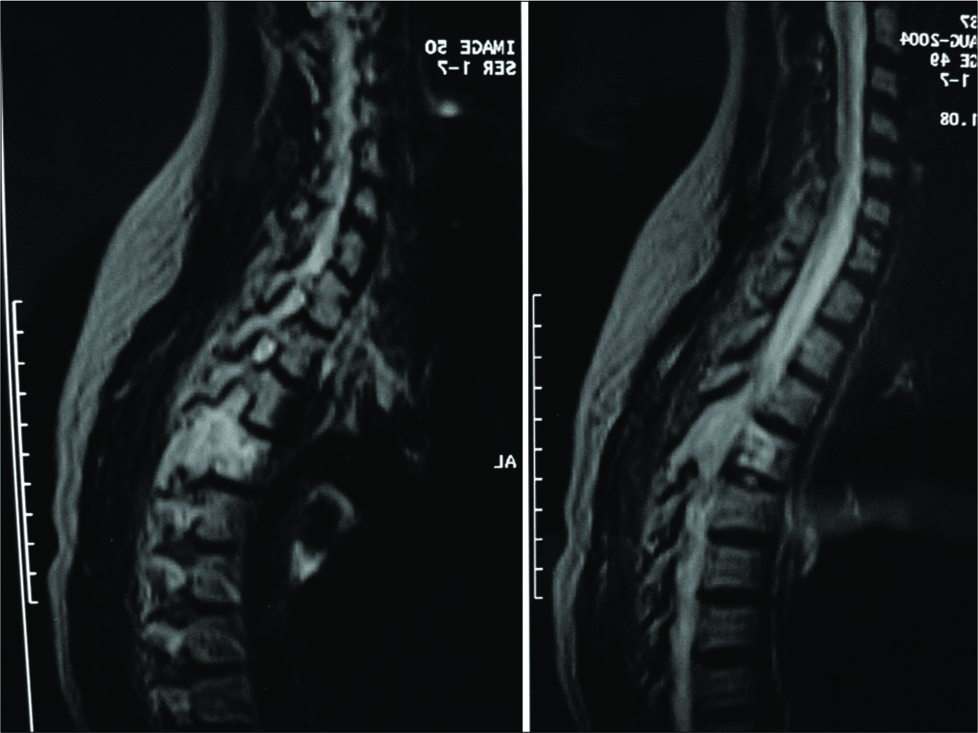
MRI findings
The MR noncontrast and contrast-enhanced studies similarly documented circumferential tumor involvement from the D3-D5 levels. Tumor involved the posterior elements of D3, D4, the body of D4, and there was an additional posterior epidural mass extending all the way from D2-5. The latter resulted in epidural cord compression and high T2 intramedullary cord signal from D2-5 [
Bone scan
The whole-body bone scan showed tumor involving D2 and D3 vertebral bodies.
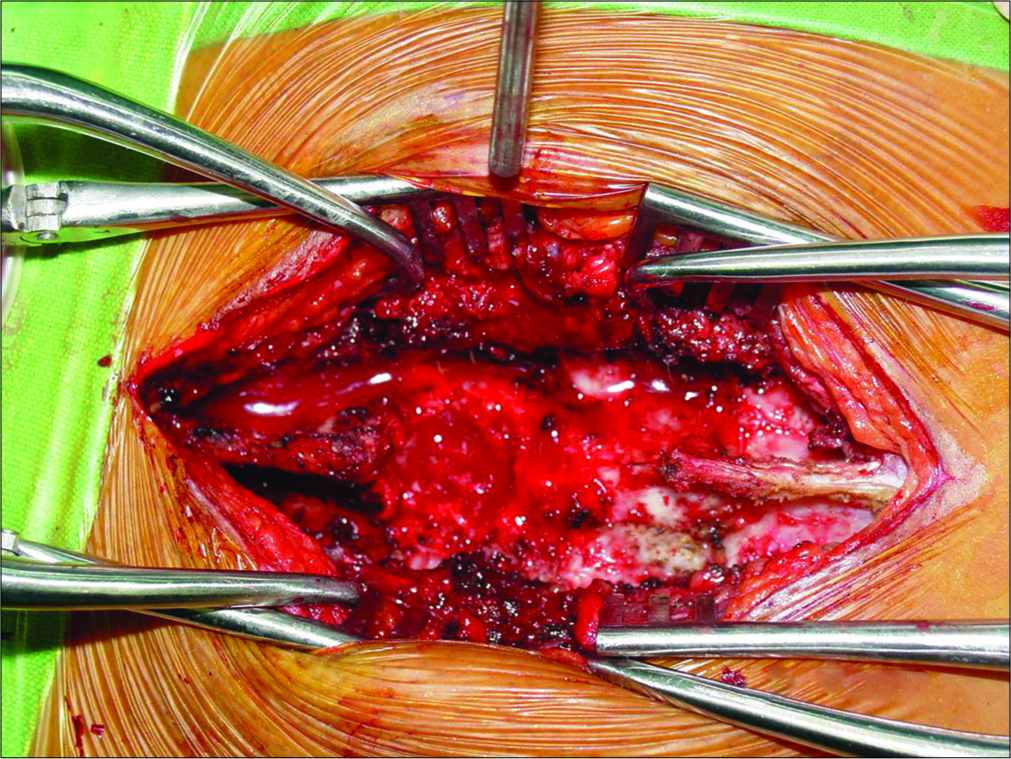
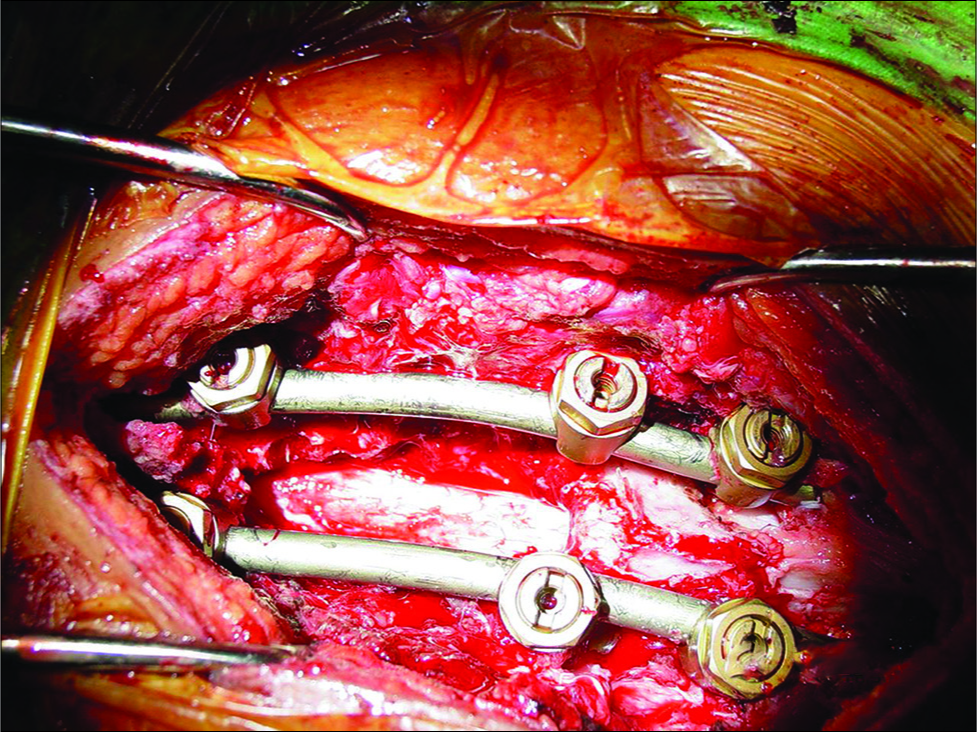
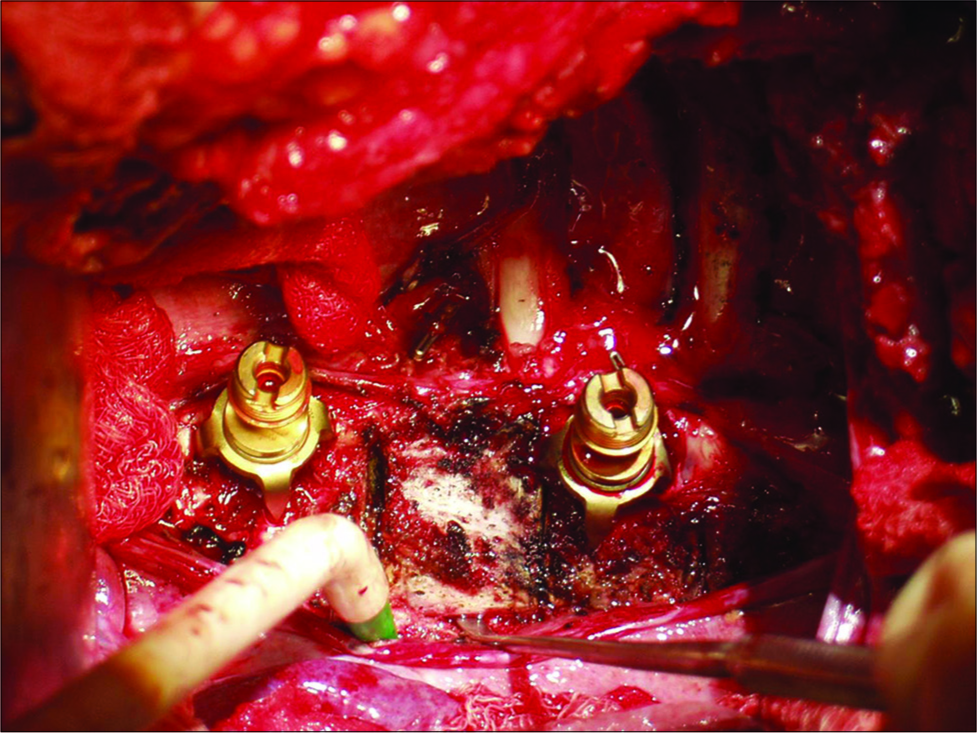
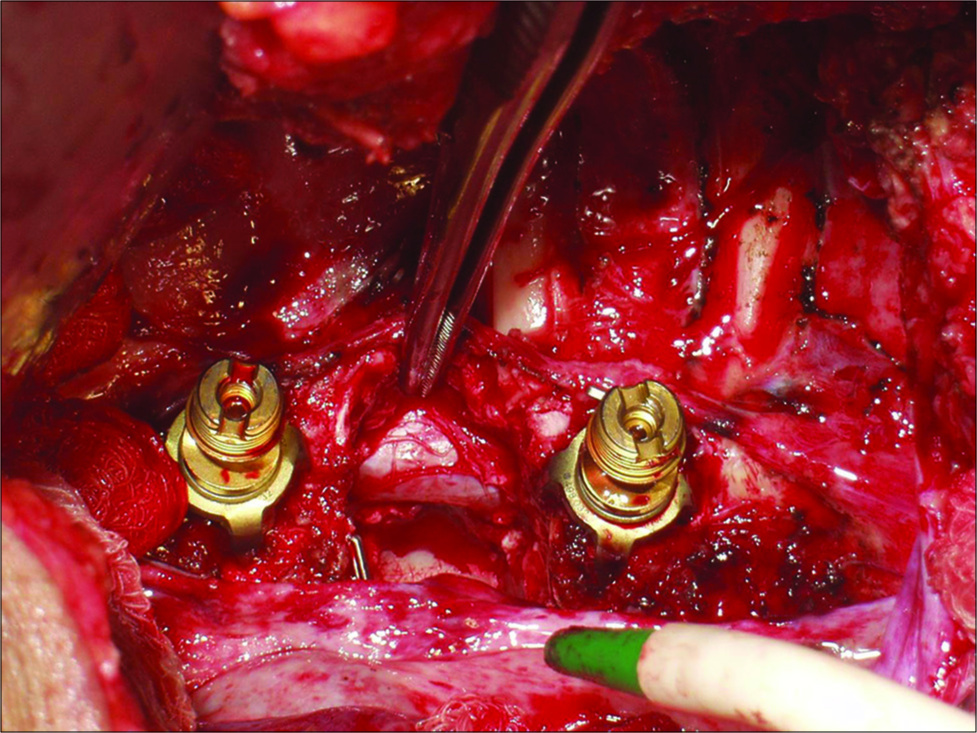
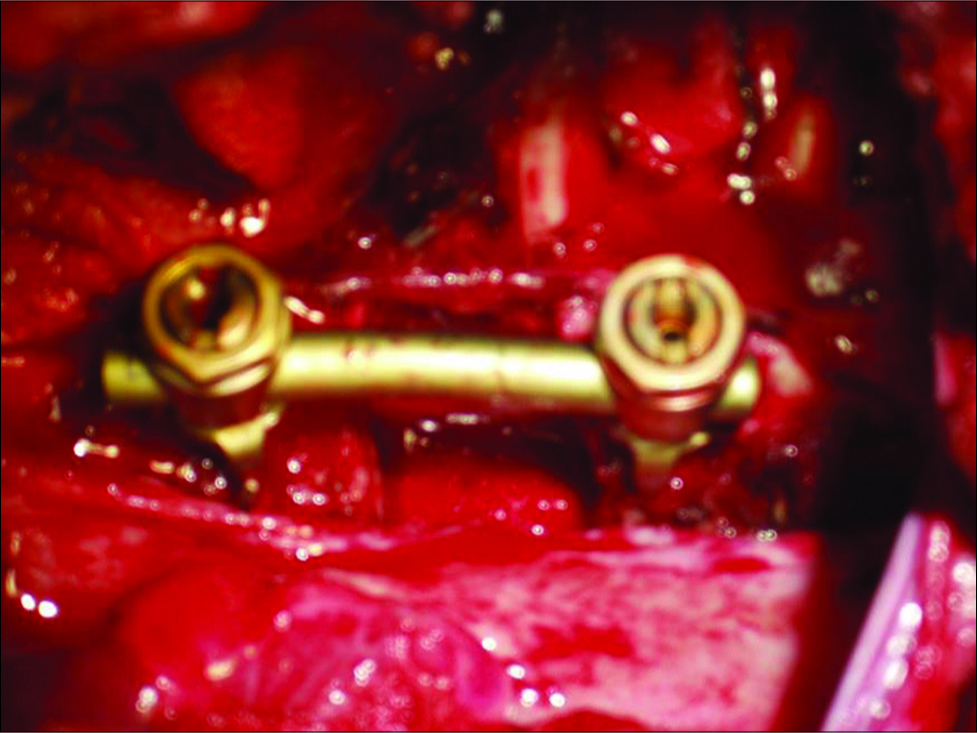
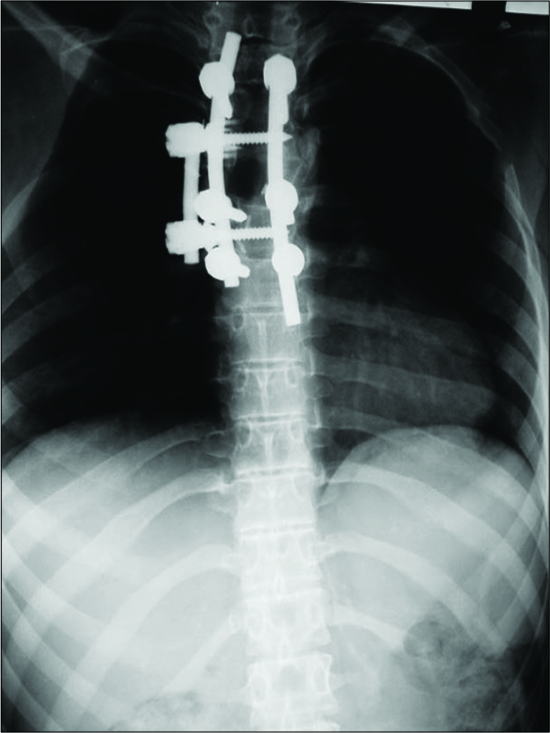
First posterior surgery: laminectomy and pedicle screw fixation
The patient underwent a left sided laminectomy from D2-D5. This allows for epidural tumor resection, additional removal of the left D4 pedicle, and pedicle screw/rod fixation at D3, D5, and D6. The tumor was vascular, soft, and partially calcified.
Pathology
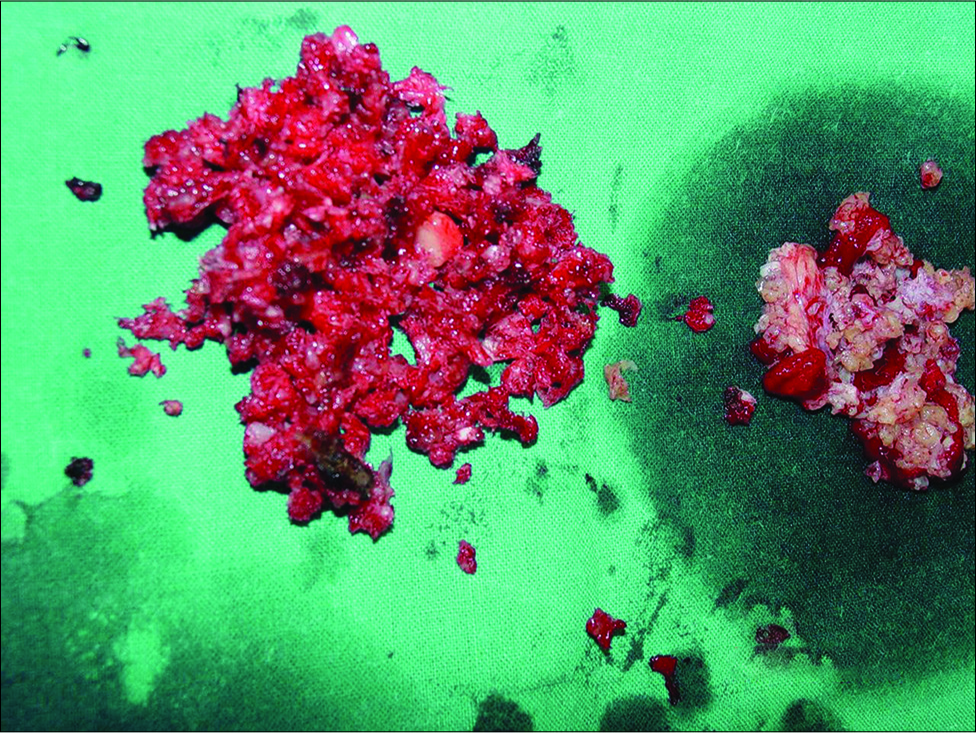
The histopathological examination showed pleomorphic spindle cells that produce disorganized osteoid, consistent with an osteosarcoma [
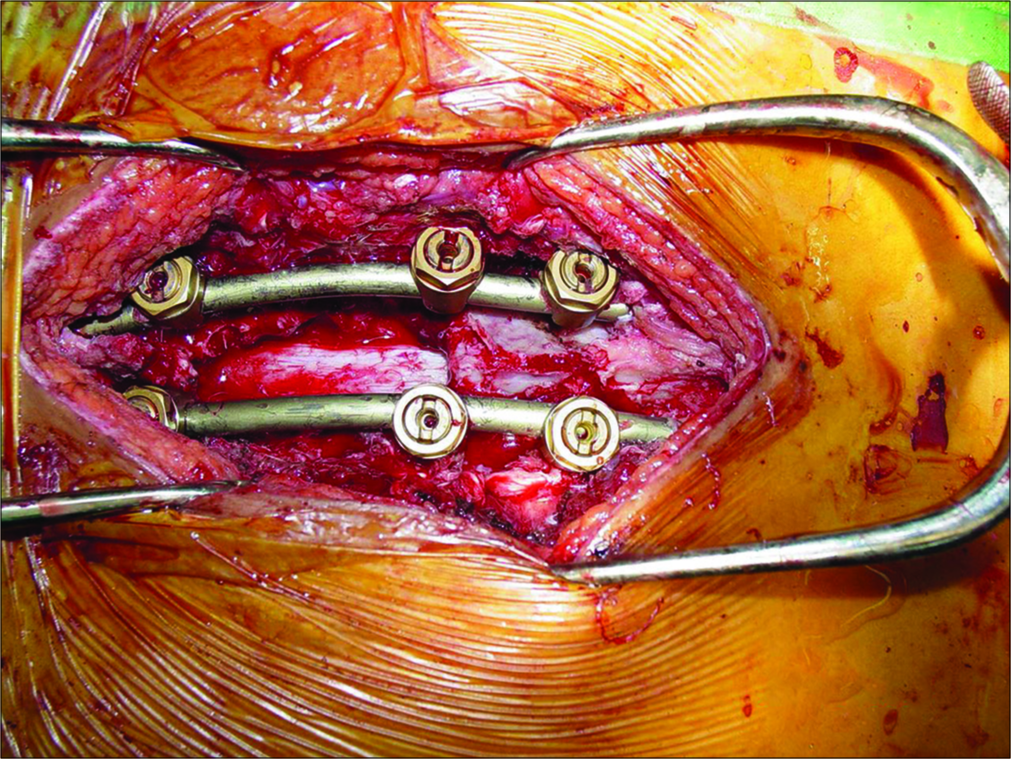
Second surgery: trans-axillary thoracotomy
The patient underwent a second trans-axillary thoracotomy (right) with removal of the 3rd and 4th ribs. This allowed for D4 body resection and D3-D4 and D4-D5 discectomies. This was followed by the anterior placement of an autogenous D3-D5 iliac crest graft [
Secondary pathology
At the second surgery, the osteosarcoma tissue appeared more vascular [
Long-term survival
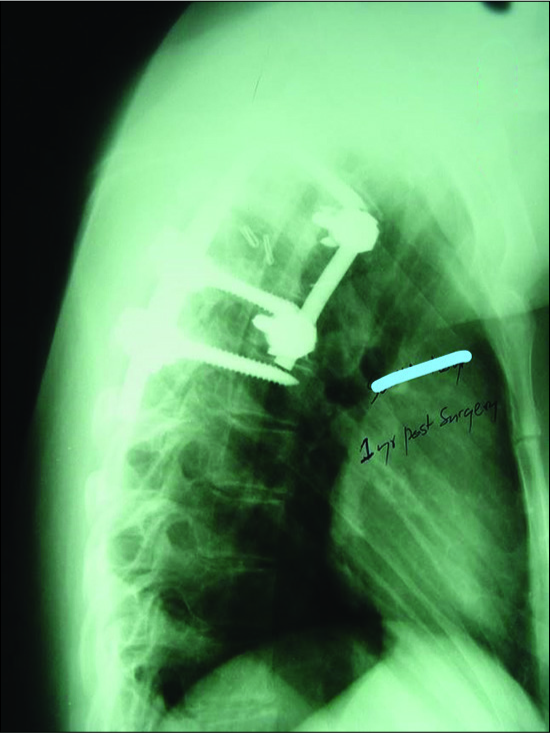
Now 15.5 years later, the patient’s follow-up CT [
Further and her presenting monoparesis has resolved and she has just mild residual spasticity.
DISCUSSION
Histology of osteosarcoma
As shown in the case, osteosarcomas typically demonstrate pleomorphic spindle cells that produce disorganized osteoid.
Survival rates for spinal osteosarcoma
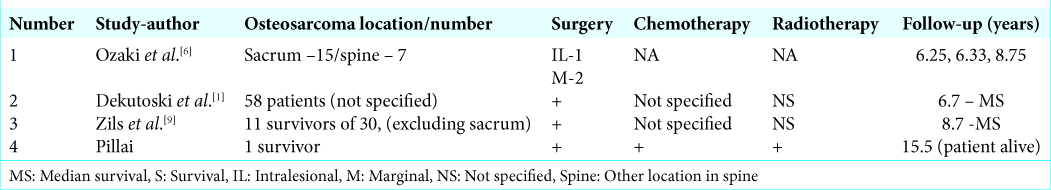
Osteosarcoma is a high-grade malignancy that rarely involves the axial skeleton. The 5-year survival rate for these patients is only 18% of with a median survival of just 23 months.[
Treatment of osteosarcomas
The current treatment for primary spinal osteosarcomas consists of a combination of surgery, chemotherapy (i.e., methotrexate, doxorubicin, and platinum compound ifosfamide) and radiation therapy (i.e., latter used mostly to treat contaminated margins). Despite extensive resections, the local recurrence rate is 30–40%, with a 60–65% incidence of metastases. Additional factors that correlate with poor prognoses include tumors larger than 10 cm, the presence of metastases at the time of surgery, and a sacral tumor location
CONCLUSION
We present a 30.5 year old female who is alive without tumor recurrence 15.5 years following resection of a thoracic D3-D5 multilevel osteosarcoma followed by both radiation and chemotherapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dekutoski MB, Clarke MJ, Rose P, Luzzati A, Rhines LD, Varga PP. Osteosarcoma of the spine: Prognostic variables for local recurrence and overall survival, a multicenter ambispective study. J Neurosurg Spine. 2016. 25: 59-68
2. Kim HJ, McLawhorn AS, Goldstein MJ, Boland PJ. Malignant osseous tumors of the pediatric spine. J Am Acad Orthop Surg. 2012. 20: 646-56
3. Mathew WC, Schwab JH.editors. Current Concepts in Primary Benign. Primary Malignant and Metastatic Tumors of the Spine. 2017. p.
4. Mukherjee D, Chaichana KL, Gokaslan ZL, Aaronson O, Cheng JS, McGirt MJ. Survival of patients with malignant primary osseous spinal neoplasms: Results from the surveillance, epidemiology, and end results (SEER) database from 1973 to 2003. J Neurosurg Spine. 2011. 14: 143-50
5. Ozaki T, Flege S, Liljenqvist U, Hillmann A, Delling G, SalzerKuntschik M. Osteosarcoma of the spine: Experience of the cooperative osteosarcoma study group. Cancer. 2002. 94: 1069-77
6. Ozaki T, Flege S, Liljenqvist U, Hillmann A, Delling G, SalzerKuntschik M. Osteosarcoma of the spine: Experience of the cooperative osteosarcoma study group. Cancer. 2002. 94: 1069-77
7. Schoenfeld AJ, Hornicek FJ, Pedlow FX, Kobayashi W, Garcia RT, DeLaney TF. Osteosarcoma of the spine: Experience in 26 patients treated at the Massachusetts general hospital. Spine J. 2010. 10: 708-14
8. Schwab J, Gasbarrini A, Bandiera S, Boriani L, Amendola L, Picci P. Osteosarcoma of the mobile spine. Spine (Phila Pa 1976). 2012. 37: E381-6
9. Zils K, Bielack S, Wilhelm M, Werner M, Schwarz R, Windhager R. Osteosarcoma of the mobile spine. Ann Oncol. 2013. 24: 2190-5