- Department of Neurosurgery, Trauma and Burns Center Ben Arous, Ben Arous, Tunisia.
- Department of Neuroradiology, National Institute of Neurology, Tunis, Tunisia.
- Department of Plastic Surgery, Trauma and Burns Center Ben Arous, Ben Arous, Tunisia.
Correspondence Address:
Mohamed Chabaane
Department of Neurosurgery, Trauma and Burns Center Ben Arous, Ben Arous, Tunisia.
DOI:10.25259/SNI_356_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamed Chabaane1, Khalil Ayadi1, Mouna Rkhami1, Cyrine Drissi2, Sarra Houimli3, Kamel Bahri1, Ihsen Zammel1, Mohamed Badri1. Management of a recurrence of a squamous cell carcinoma of the scalp with extension to the brain: A case report and literature review. 21-Oct-2020;11:347
How to cite this URL: Mohamed Chabaane1, Khalil Ayadi1, Mouna Rkhami1, Cyrine Drissi2, Sarra Houimli3, Kamel Bahri1, Ihsen Zammel1, Mohamed Badri1. Management of a recurrence of a squamous cell carcinoma of the scalp with extension to the brain: A case report and literature review. 21-Oct-2020;11:347. Available from: https://surgicalneurologyint.com/surgicalint-articles/10348/
Abstract
Background: Squamous cell carcinoma (SCC) is the most common form of nonmelanoma skin cancer after basal cell carcinoma. Simple excision can be the treatment at early stages of diagnosis. However, at late stages, treatment is more complex due to extension to the skull and the dura. In extremely rare cases, it can invade the brain making it a challenging situation for treatment.
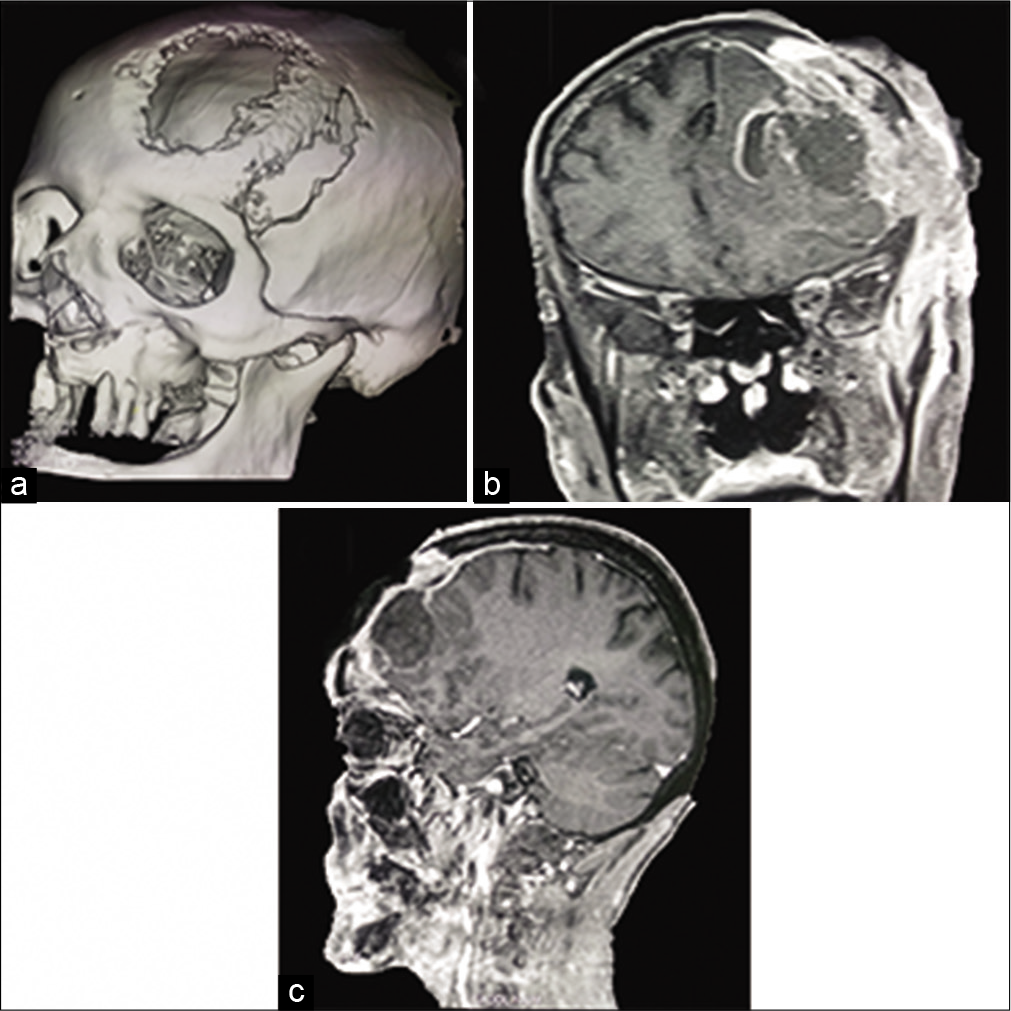
Case Description: We present the case of a 54-year-old man with a history of cutaneous SCC who presented an invasive left frontal recurrence with brain invasion 19 years after initial surgery. The patient underwent surgery which consisted in tumor removal and bone and skin reconstruction. Immediate and late outcomes were favorable.
Conclusion: Multidisciplinary treatment for SCC diagnosed in advanced stages is the best way to obtain encouraging results. Although significant advancements have been made, further study is needed for cases with advanced disease.
Keywords: Neural invasion, Prognosis, Skin carcinoma, Surgery
INTRODUCTION
Squamous cell carcinoma (SCC) is the second most common subtype of nonmelanoma skin cancer representing 20% of these tumors.[
CASE PRESENTATION
A 54-year-old man presented with a history of a left frontal cutaneous cell carcinoma. The patient had surgical removal of the tumor followed by radiation therapy in 2000. He had no metastasis at that time. He was then lost to follow-up for more than a decade. He presented with a painful and ulcerated extensive left frontal cutaneous lesion which occasionally bled. The progressive growth of the lesion was neglected by the patient for years. Because of a rapid progression in the past 3 months, he consulted. No other symptoms were reported. Physical examination showed a 12 × 15 × 14 cm left frontal cauliflower-like mass with a necrotic center and peripheral subcutaneous induration with erythema [
DISCUSSION
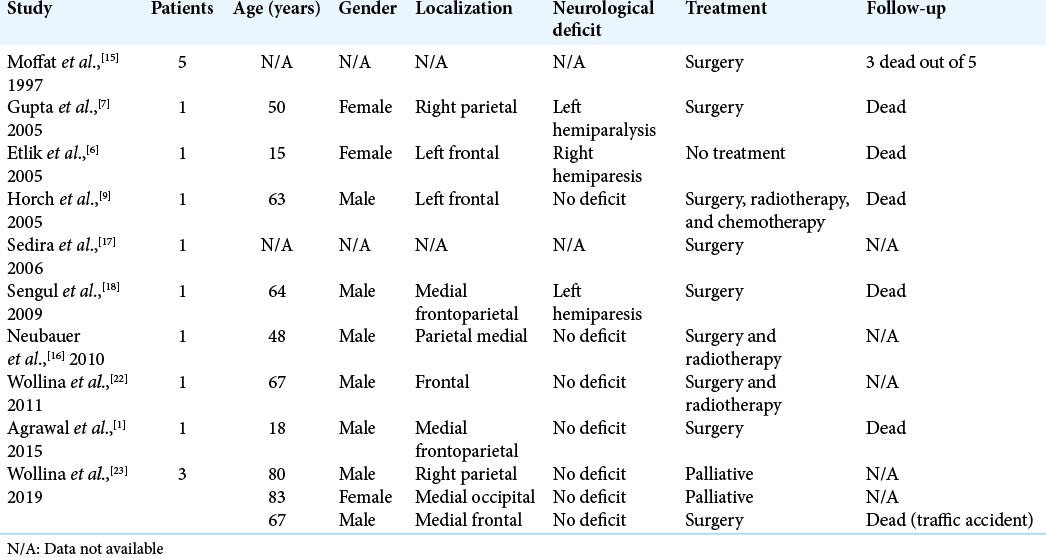
SCC is the second most common subtype of nonmelanoma skin cancer after basal cell carcinoma. Due to their progressive and slow extension, these tumors are usually diagnosed before extension to the skull. However, in late stages of development, the skull and the dura can be invaded. In very few cases, SCC can extend to the brain. PubMed/MEDLINE search using the keywords squamous cell, carcinoma, scalp, and brain, found 16 similar cases with brain invasion [
Recurrence factors are more common in patients who are immunosuppressed, as well those who have tumors with perineural invasion, poor differentiation, deep extension, and those of large size.[
Death rate due to this tumor seems to be low, Estall et al. reported 59% of overall survival and 94% of disease specific survival which suggests that only a small proportion died specifically because of their tumor, age comorbidities were responsible of most deaths.[
CONCLUSION
Treating a SCC can be challenging when diagnosed at an advanced stage. A multidisciplinary team is needed to perform a delicate surgery. Although significant advancements have been made, further study is needed for cases with advanced disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank all the junior physicians that participated in the surgery and the postoperative management of this patient.
References
1. Agrawal M, Bagaria H, Bhasme V, Poonia N, Chakotiya P. Post-burn spontaneous brain fungation caused by infiltrating Marjolin’s ulcer of scalp. Asian J Neurosurg. 2015. 2015: 1-7
2. Brantsch KD, Meisner C, Schonfisch B, Trilling B, WehnerCaroli J, Rocken M. Analysis of risk factors determining prognosis of cutaneous squamous-cell carcinoma: A prospective study. Lancet Oncol. 2008. 9: 713-20
3. Dundar Y, Cannon RB, Hunt JP, Monroe M, Suneja G, Hitchcock YJ. Radiotherapy regimens in patients with nonmelanoma head and neck skin cancers. Int J Dermatol. 2018. 57: 441-8
4. Emsen IM. A great marjolin’s ulcer of the scalp invading outer calvarial bone and its different treatment with support of medpor. J Craniofac Surg. 2008. 19: 1026-9
5. Estall V, Allen A, Webb A, Bressel M, Mc Cormack C, Spillane J. Outcomes following management of squamous cell carcinoma of the scalp: A retrospective series of 235 patients treated at the Peter MacCallum cancer centre. Australas J Dermatol. 2017. 58: e207-15
6. Etlik Ö, Bay A, Izmirli M, Uǧraş S, Yilmaz N, Turan A. Deep intracranial extension of squamous cell carcinoma of the scalp. Pediatr Blood Cancer. 2005. 45: 994-6
7. Gupta SK, Sandhir RK, Jaiswal AK, Kumar S. Marjolin’s ulcer of the scalp invading calvarial bone, dura and brain. J Clin Neurosci. 2005. 12: 693-5
8. Handler MZ, Goldberg DJ. Cutaneous squamous cell carcinoma of the scalp extending to the skull: A case report and review of the literature. J Cosmet Dermatol. 2018. 17: 232-4
9. Horch RE, Stark GB, Beier JP. Unusual explosive growth of a squamous cell carcinoma of the scalp after electrical burn injury and subsequent coverage by sequential free flap vascular connection-a case report. BMC Cancer. 2005. 5: 150
10. Howle JR, Morgan GJ, Kalnins I, Palme CE, Veness MJ. Metastatic cutaneous squamous cell carcinoma of the scalp. ANZ J Surg. 2008. 78: 449-53
11. Jenkins G, Smith AB, Kanatas AN, Houghton DR, Telfer MR. Anatomical restrictions in the surgical excision of scalp squamous cell carcinomas: Does this affect local recurrence and regional nodal metastases?. Int J Oral Maxillofac Surg. 2014. 43: 142-6
12. Kadakia S, Ducic Y, Marra D, Chan D, Saman M, Sawhney R. Cutaneous squamous cell carcinoma of the scalp in the immunocompromised patient: Review of 53 cases. Oral Maxillofac Surg. 2016. 20: 171-5
13. Lang PG, Baun MA, Kwatar R. Aggressive squamous carcinomas of the scalp. Dermatol Surg. 2006. 32: 1163-70
14. Liao CT, Kang CJ, Lee LY, Hseuh C, Lin CY, Fan KH. Association between multidisciplinary team care approach and survival rates in patients with oral cavity squamous cell carcinoma. Head Neck. 2016. 38: E1544-53
15. Moffat DA, Grey P, Ballagh RH, Hardy DG. Extended temporal bone resection for squamous cell carcinoma. Otolaryngol Head Neck Surg. 1997. 116: 617-23
16. Neubauer KE, Goldstein GD, Plumb SJ. Squamous cell carcinoma of the scalp in organ transplant recipients: Exploring mechanisms for recurrence and treatment guidelines. Dermatol Surg. 2010. 36: 185-93
17. Sedira MA, Amin AA, Rifaat MA, El-Sebai HI, El-Badawy MA, Kassem HA. Locally advanced tumors of the scalp: The Egyptian national cancer institute experience. J Egypt Natl Canc Inst. 2006. 18: 250-7
18. Sengul G, Hadi-Kadioglu H. Penetrating Marjolin’s ulcer of scalp involving bone, dura mater and brain caused by blunt trauma to the burned area. Neurocirugia (Astur). 2009. 20: 474-7
19. Stark J, Podda S, Szymanski K. Invasive squamous cell carcinoma of the scalp and calvarium: A multidisciplinary approach. Eplasty. 2016. 16: e29
20. Tan PY, Ek E, Su S, Giorlando F, Dieu T. Incomplete excision of squamous cell carcinoma of the skin: A prospective observational study. Plast Reconstr Surg. 2007. 120: 910-6
21. van Tuyl R, Gussack GS. Prognostic factors in craniofacial surgery. Laryngoscope. 1991. 101: 240-4
22. Wollina U, Bayyoud Y, Kittner T, Dürig E. Giant tricholemmal squamous cell carcinoma with cranial infiltration. J Clin Aesthet Dermatol. 2011. 4: 34-7
23. Wollina U, Kittner T, Nowak A. Nonmelanoma skin cancer with skull infiltration and cranial involvement. Open Access Maced J Med Sci. 2019. 7: 3030-3
24. Ziegler A, Walker R, Varvares M. Oncologic outcomes of invasive squamous cell carcinoma of the scalp requiring resection of cranial bone. J Neurol Surg A Cent Eur Neurosurg. 2016. 77: 308-11