- Department of Neurosurgery, Barrow Neurological Institute, Phoenix, Arizona, United States
- Department of Neurosurgery, Perelman School of Medicine, University of Pennsylvania, Philadelphia, United States.
Correspondence Address:
John E. Wanebo, Department of Neurosurgery, Barrow Neurological Institute, Phoenix, Arizona, United States.
DOI:10.25259/SNI_796_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Steve S. Cho1, S. Harrison Farber1, Hayley Kiernan1, Clare W. Teng2, Oliver R. Wanebo1, Francisco A. Ponce1, Luis M. Tumialán1, John E. Wanebo1. Management of hangman’s fractures using anchored anterior cervical cages. 07-Apr-2023;14:125
How to cite this URL: Steve S. Cho1, S. Harrison Farber1, Hayley Kiernan1, Clare W. Teng2, Oliver R. Wanebo1, Francisco A. Ponce1, Luis M. Tumialán1, John E. Wanebo1. Management of hangman’s fractures using anchored anterior cervical cages. 07-Apr-2023;14:125. Available from: https://surgicalneurologyint.com/surgicalint-articles/12244/
Abstract
Background: Hangman’s fractures comprise approximately 20% of C2 fractures and often require surgery to correct significant angulation and/or subluxation. Recently, anchored anterior cervical cages (ACCs) have been used to fuse C2-3 as they reduce the risks of soft-tissue dissection, bone drilling, operative time, and postoperative dysphagia.
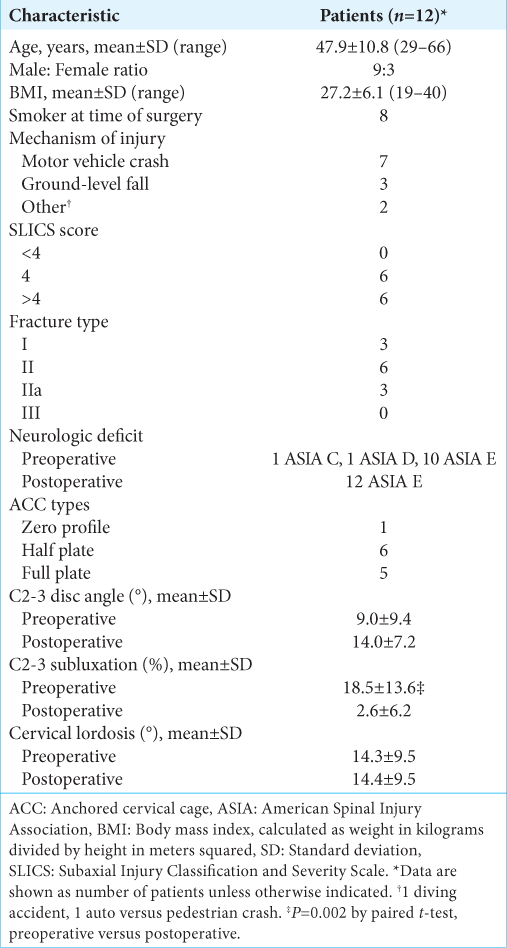
Methods: This single-center and retrospective study (2012–2019) included 12 patients (3 type I, 6 type II, and 3 type IIa fractures) undergoing C2-3 ACCs (zero profile, half plate, full plate). Preoperative and postoperative radiographic and clinical data were analyzed.
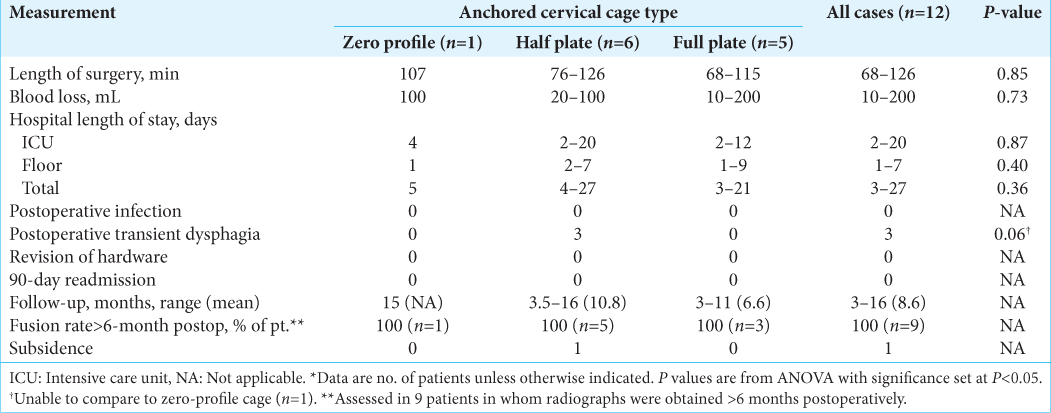
Results: The 12 patients demonstrated the following findings: a mean operative time of 106 ± 21 min, blood loss averaging 67 ± 58 mL, and mean length of stay of 9.8 ± 7.7 days (6.4 ± 5.5 days in intensive care). The mean differences in preoperative versus postoperative radiographs showed an increase in disc angle (9.0° ± 9.4° vs. 14.0° ± 7.2°), reduction of subluxation (18.5% ± 13.6% vs. 2.6% ± 6.2%), and maintenance of C2-7 lordosis (14.3° ± 9.5° vs. 14.4° ± 9.5°). All patients demonstrated fusion on dynamic films obtained >6 months postoperatively. In addition, only one patient had Grade 0 subsidence, three had transient postoperative dysphagia, whereas none had either intraoperative complications or 90-day readmissions.
Conclusion: ACCs proved to be a viable alternative to traditional anterior cervical discectomy/fusion to treat 12 patients with C2-3 hangman’s fractures in this preliminary study.
Keywords: Anchored cervical cages, Anterior cervical discectomy and fusion, Hangman’s fracture, Zero-profile
INTRODUCTION
Surgical alternatives for C2-C3 fusions include C2 pedicle screws, C2-3/C1-3 posterior spinal fusion, single-level C2-3 anterior cervical discectomy and fusion (ACDF), or, since 2009, anchored cervical cages (ACCs: Zero profile, half plate, or full plate).[
MATERIALS AND METHODS
Study design
We performed an IRB-approved retrospective cohort study of 12 patients who underwent C2-3 ACDF with ACCs to treat traumatic C2 pars fractures between 2012 and 2019. Patient billing codes, operative notes, and imaging data were evaluated by three senior authors blinded to the study design. Anteroposterior and lateral cervical radiographs were obtained 1 month postoperatively, and dynamic films obtained >6 months postoperatively were used to assess fusion (i.e., criteria of <2 mm between C2 and C3 spinous processes).[
Clinical data
Twelve patients underwent C2-3 ACDF with ACCs to treat traumatic hangman’s fractures [
Preoperative imaging
In the 12 patients, the mean preoperative C2-3 disc angle was 9.0° ± 9.4°, whereas the mean preoperative subluxation, relative to the length of the C3 superior endplate, was 18.5% ± 13.6% [
Operative procedure
One of three types of ACC devices was placed following routine C2-3 anterior discectomies. These devices were all polyetheretherketone cages with the following designs: Zero-profile plates (n = 1), half plates (n = 6), and full plates (n = 5). The choice of plate type was based on the fracture morphology and presence of osteophytes. For those with Subaxial Injury Classification and Severity Scale score ≥4, a half- or full-plate ACC was used, except when significant osteophytes made it difficult to place the plate safely.
Statistical analysis
Statistical analyses were performed using STATA 10 and included paired t-tests and analysis of variance (ANOVA).
RESULTS
Postoperative imaging
For all 12 patients, the mean postoperative C2-3 disc angle on postoperative images averaged 14.0° ± 7.2° and the mean postoperative subluxation for all 12 patients was 2.6% ± 6.2% [
Comparable postoperative results/outcomes for all three fusion constructs
Fusion rates were comparable for all three types of fusion plates (i.e., a zero-profile plate [one patient], half plate [six patients], and full plate [five patients]) as documented using the ANOVA test [
Postoperative complications limited to dysphagia
The only postoperative complication observed in all three treatment groups were three instances of dysphagia at the time of discharge (i.e., resolved within 1–2 postoperative months). On follow-up, 10 patients remained in American Spinal Injury Association (ASIA) E, while the two patients with preoperative ASIA C and ASIA D deficits improved to ASIA E status.
DISCUSSION
ACCs viable alternative for anterior stabilization of C2-3 hangman’s fractures
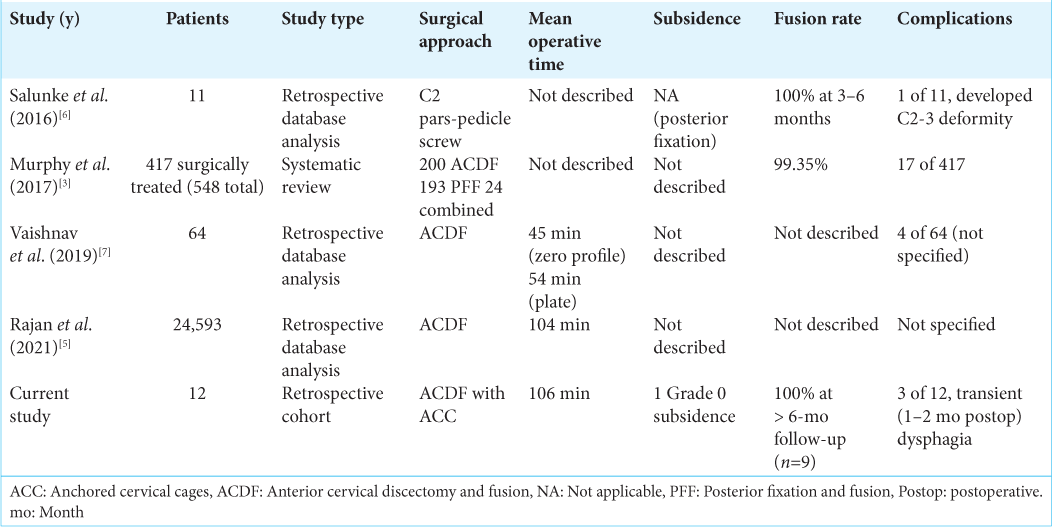
Surgical stabilization for traumatic hangman’s fractures is typically achieved using one of several constructs: C2 pedicle screws, C1-3 posterior spinal fusion, or C2-3 ACDF. However, ACCs, with the anterior plate attached to the graft and directly fixed to the vertebral bodies, offer a viable alternative to the traditional ACDF.[
Comparable operative time and fusion but possibly reduced dysphagia rates for single-level ACCs versus ACDF
Our mean operative time for a single-level ACC at the C2-3 level was 106 min versus an average time for a single-level ACDF of 104 min in a retrospective study of 24,593 patients.[
CONCLUSION
We successfully used three types of ACC devices to perform 12 C2-3 fusions for treatment of traumatic hangman’s fractures. ACCs offered comparable operative times and fusion rates with similar to lower rates of postoperative dysphagia compared with standard fixation techniques.
Declaration of patient consent
Patient’s consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
John E. Wanebo is a consultant for Zimmer Biomet. All other authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this manuscript. Portions of this manuscript were presented orally at the Western Neurosurgical Society 63rd Annual Meeting, September 9, 2017, Banff, Canada.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
We thank the staff of Neuroscience Publications at Barrow Neurological Institute for assistance with manuscript preparation.
References
1. Kaiser MG, Mummaneni PV, Matz PG, Anderson PA, Groff MW, Heary RF. Radiographic assessment of cervical subaxial fusion. J Neurosurg Spine. 2009. 11: 221-7
2. Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 2013. 19: 110-8
3. Murphy H, Schroeder GD, Shi WJ, Kepler CK, Kurd MF, Fleischman AN. Management of Hangman’s fractures: A systematic review. J Orthop Trauma. 2017. 31: S90-5
4. Panchal R, Gandhi A, Ferry C, Farmer S, Hansmann J, Wanebo J. A biomechanical evaluation of a next-generation integrated and modular ACDF device possessing full-plate, half-plate, and no-profile fixation iterations. Global Spine J. 2019. 9: 826-33
5. Rajan PV, Emara AK, Ng M, Grits D, Pelle DW, Savage JW. Longer operative time associated with prolonged length of stay, non-home discharge and transfusion requirement after anterior cervical discectomy and fusion: An analysis of 24,593 cases. Spine J. 2021. 21: 1718-28
6. Salunke P, Sahoo SK, Krishnan P, Chaterjee D, Sodhi HB. Are C2 pars-pedicle screws alone for Type II Hangman’s fracture overrated?. Clin Neurol Neurosurg. 2016. 141: 7-12
7. Vaishnav AS, Saville P, McAnany S, Patel D, Haws B, Khechen B. Predictive factors of postoperative dysphagia in single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2019. 44: E400-7