- Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, United States,
- Department of Biostatistics and Epidemiology, University of Oklahoma Health Sciences Center, Oklahoma City, United States.
Correspondence Address:
Alison M. Westrup, Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, United States.
DOI:10.25259/SNI_107_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alison M. Westrup1, Landon S. Hendrickson1, Kendall L. Hughes1, Jaylun I. Smith1, Christen M. O’Neal1, Sixia Chen2, Andrew K. Conner1. Management of nonoperative cervical spine fractures: An institutional analysis of follow-up duration and image acquisition. 23-Jun-2022;13:260
How to cite this URL: Alison M. Westrup1, Landon S. Hendrickson1, Kendall L. Hughes1, Jaylun I. Smith1, Christen M. O’Neal1, Sixia Chen2, Andrew K. Conner1. Management of nonoperative cervical spine fractures: An institutional analysis of follow-up duration and image acquisition. 23-Jun-2022;13:260. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11667
Abstract
Background: How long do nonoperative cervical fractures have to be followed and with how many imaging studies?
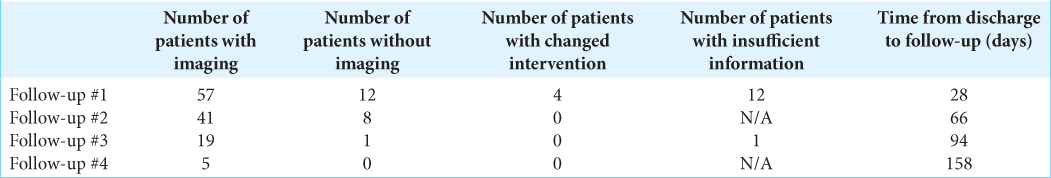
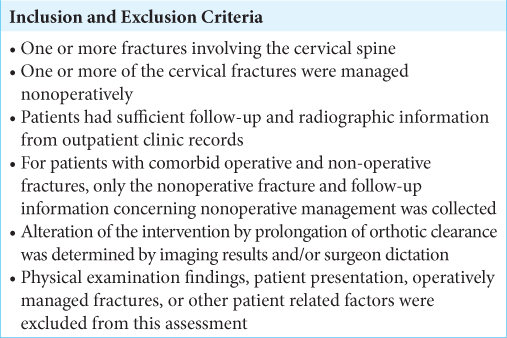
Methods: We reviewed 69 adult patients with 122 (31 occiptocervical and 91 sub-axial) cervical fractures; at least one of the cervical fractures was managed nonoperatively. Outcomes were assessed along with the optimal follow-up duration and frequency of various diagnostic studies.
Results: An average of four follow-up visits occurred on average 28-, 66-, 94-, and 158-day post hospital discharge. The average time between discharge and orthotic clearance was 70 days (±32.4 days). Radiographic studies were obtained at follow-up visits, respectively, in, 82.6%, 83.6%, 94.7%, and 100% of patients.
Conclusion: The trend for managing nonoperative cervical fractures was an unduly prolonged follow-up duration that included obtaining too many imaging studies.
Keywords: Cervical fracture, Cervical spine, Conservative management, Non-operative, Orthotic
INTRODUCTION
Recent studies have reported that 0.6% of the cumulative risk of cancer to 75 years of age can be attributable to diagnostic X-rays and estimate that 0.4% of cancers in the United States are caused by CT scans.[
MATERIALS AND METHODS
Clinical data
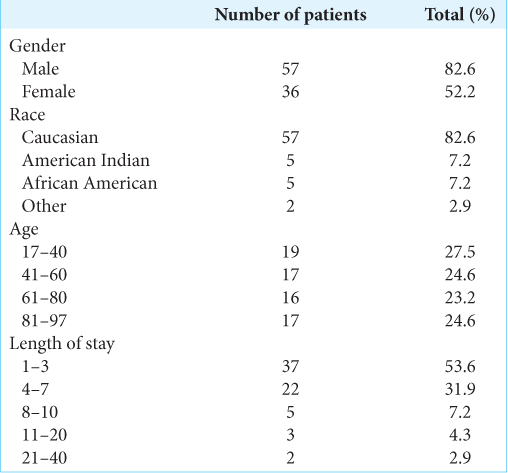
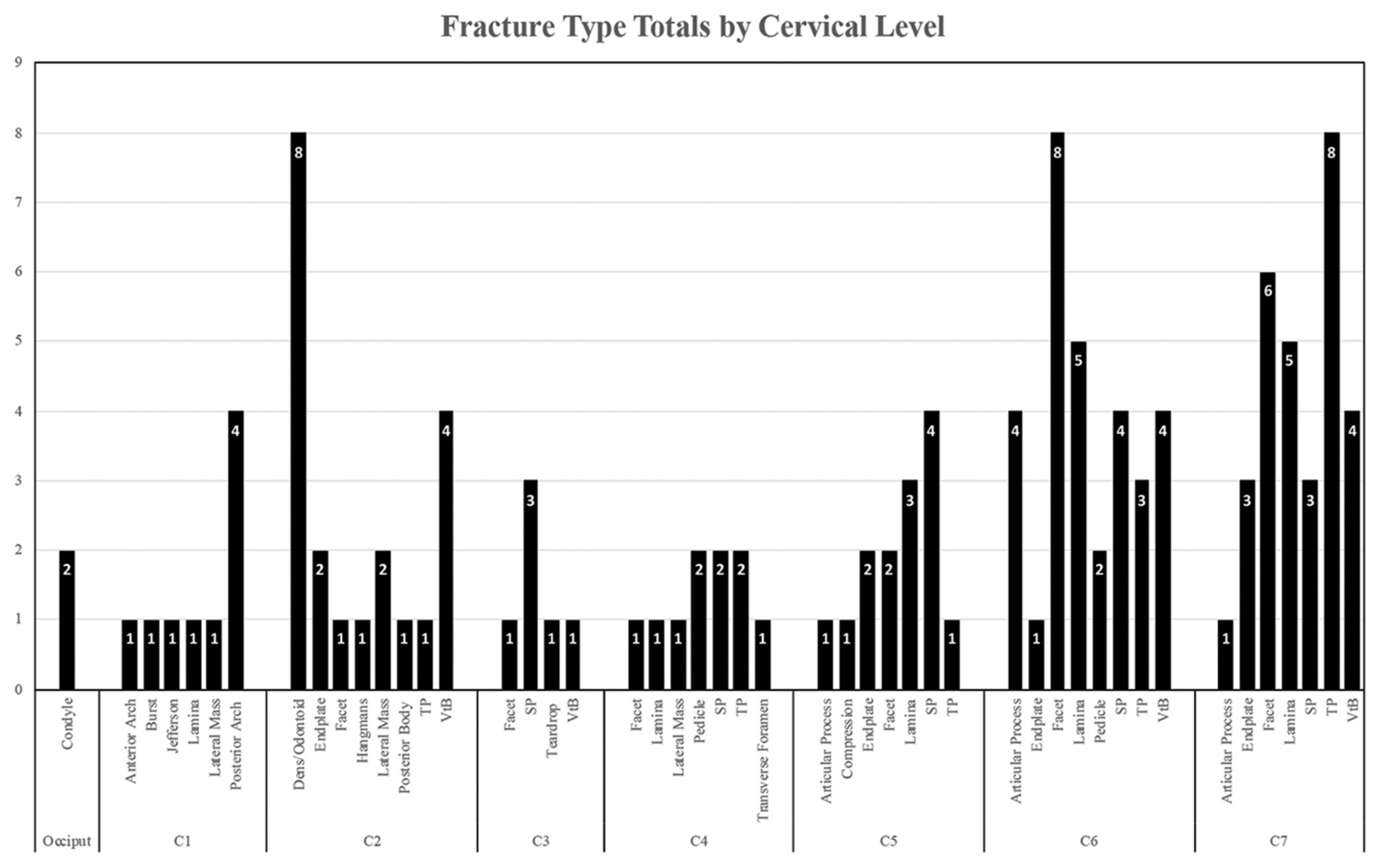
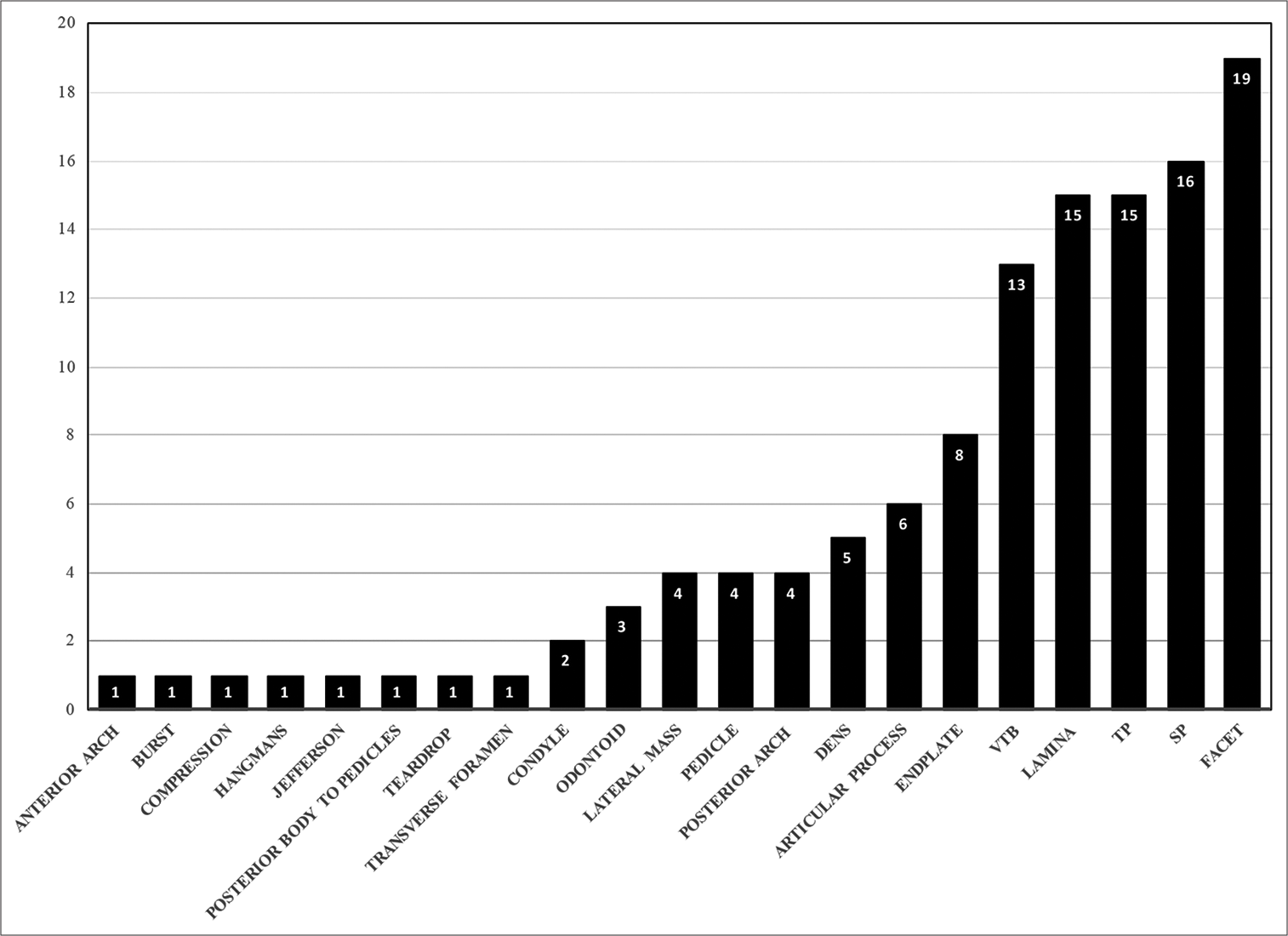
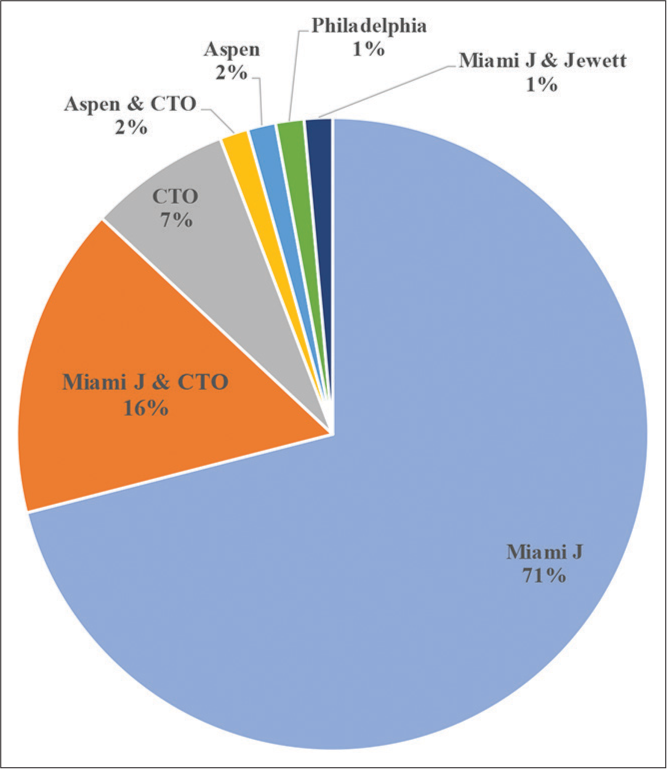
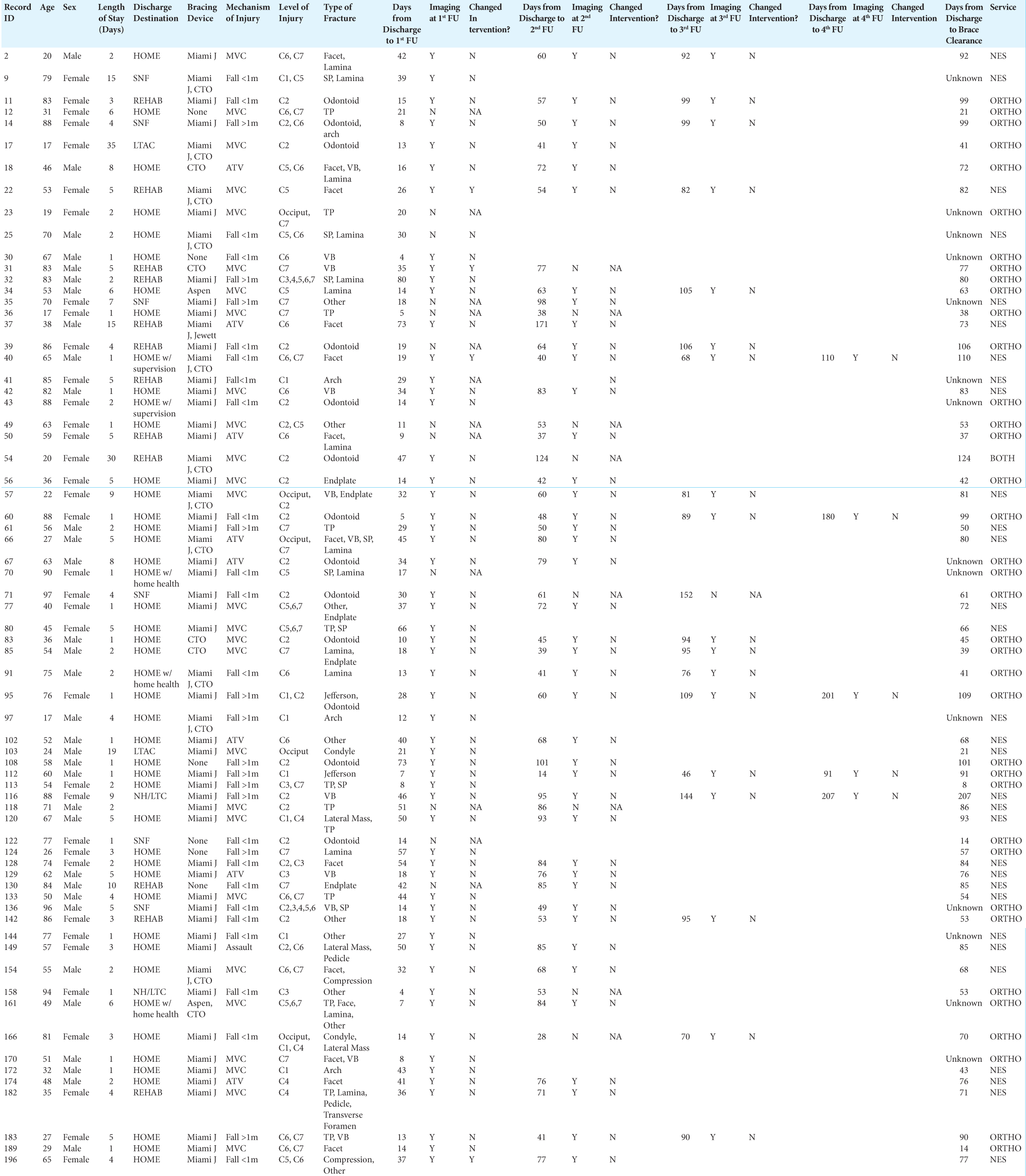
There were 69 patients included in this study (122 fractures) who averaged 58 years of age. The most common mechanism of injury was motor vehicle accidents (n = 27, 39%), followed by falls <1 m (n = 21, 30%). Other variables studied included: patient demographics, average hospital length of stay, and the types of nonoperative cervical fractures treated [
RESULTS
The study revealed that all patients had, on average, four follow-up visits occurred on average 28-, 66-, 94-, and 158-day post hospital discharge [Supplemental
DISCUSSION
This analysis of the nonoperative management of 69 adults confirmed that only their initial postoperative X-rays obtained at an average of 28-day post discharge impacted their clinical management. All subsequent X-rays obtained at an average of 66-, 94-, and 158-day post discharge did not. Therefore, repeating postoperative X-rays and exposing patients to additional radiation with prolongation of the follow-up period were all unnecessary.
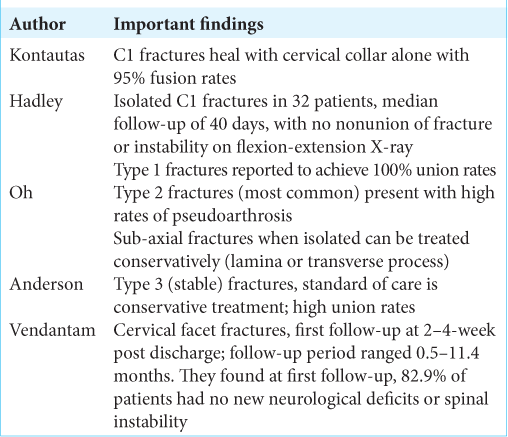
Success of conservative management of C1-C2 fractures
Kontautas et al. and Hadley et al. found that isolated C1 fractures heal well with a cervical collar alone(95% fusion rate).[
In our cohort, none the patients with isolated C1 fractures were followed beyond the second follow-up visit at 66-days, and further imaging never altered the clinical management. For isolated C2 fractures, our cohort consisted of 15 patients; managed with various orthoses with orthotic clearance on average 83-day post discharge [
Conservative management of sub-axial fractures
Vedantam et al. reviewed 35 patients with sub-axial facet fractures managed non-operatively (cervical bracing alone) and 82.9% of patients fused successfully.[
Optimal follow-up for nonsurgical cervical fractures
At present, there are few recommendations regarding the optimal the number/types of imaging studies needed to follow patients with nonoperative cervical fractures and the optimal follow-up duration. Here, in 69 patients, we found that most will undergo a change in therapy/intervention based on X-ray studies obtained at the first follow-up visit, 28-day post discharge. Interestingly, no patients required additional alterations in management based on X-rays obtained on average 66-, 94-, and 158-day post discharge. Nonetheless, as patients typically had cervical orthoses removed an average of 70-day post discharge; the second follow-up visit was likely necessary.
CONCLUSION
When we studied 69 patients treated conservatively for nonoperative cervical spine fractures, we found that X-ray studies obtained on average 28-, 66-, 94-, and 158-day post discharge did not significantly alter patients’ clinical management, but unnecessarily prolonged the follow-up duration.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
SUPPLEMENTAL TABLES
References
1. Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974. 56: 1663-74
2. Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007. 357: 2277-84
3. de Gonzalez AB, Darby S. Risk of cancer from diagnostic X-rays: Estimates for the UK and 14 other countries. Lancet. 2004. 363: 345-51
4. Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute traumatic atlas fractures: Management and long term outcome. Neurosurgery. 1988. 23: 31-5
5. Kontautas E, Ambrozaitis KV, Kalesinskas RJ, Spakauskas B. Management of acute traumatic atlas fractures. J Spinal Disord Tech. 2005. 18: 402-5
6. Oh J, Hee HT, Butler .editors. Outcomes of cervical spine injuries following non-operative management. Cervical Spine Injuries: Epidemiology, Long-Term Outcomes and Complications. Hauppauge, New York: Nova Publishers; 2015. p. 19-38
7. Vedantam A, Fridley JS, Navarro JC, Gopinath SP. Management of acute unilateral nondisplaced subaxial cervical facet fractures. Oper Neurosurg (Hagerstown). 2018. 14: 104-11