- Department of Neurosurgery, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
DOI:10.25259/SNI-75-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sajjad Muhammad, Mika Niemelä. Management of oculomotor nerve schwannoma: Systematic review of literature and illustrative case. 26-Mar-2019;10:40
How to cite this URL: Sajjad Muhammad, Mika Niemelä. Management of oculomotor nerve schwannoma: Systematic review of literature and illustrative case. 26-Mar-2019;10:40. Available from: http://surgicalneurologyint.com/surgicalint-articles/9244/
Abstract
Background: Oculomotor nerve schwannoma (ONS) is an extremely rare intracranial benign tumor. Till date, there is no standard treatment of oculomotor schwannoma. Here, we present an illustrative case report of ONS, perform a systematic review of literature on surgically and radiosurgically treated cases and morbidity related to both treatment modalities.
Methods: We performed a systematic review of literature for cases with ONS treated with surgery or radiosurgery using PubMed/Ovid Medline.
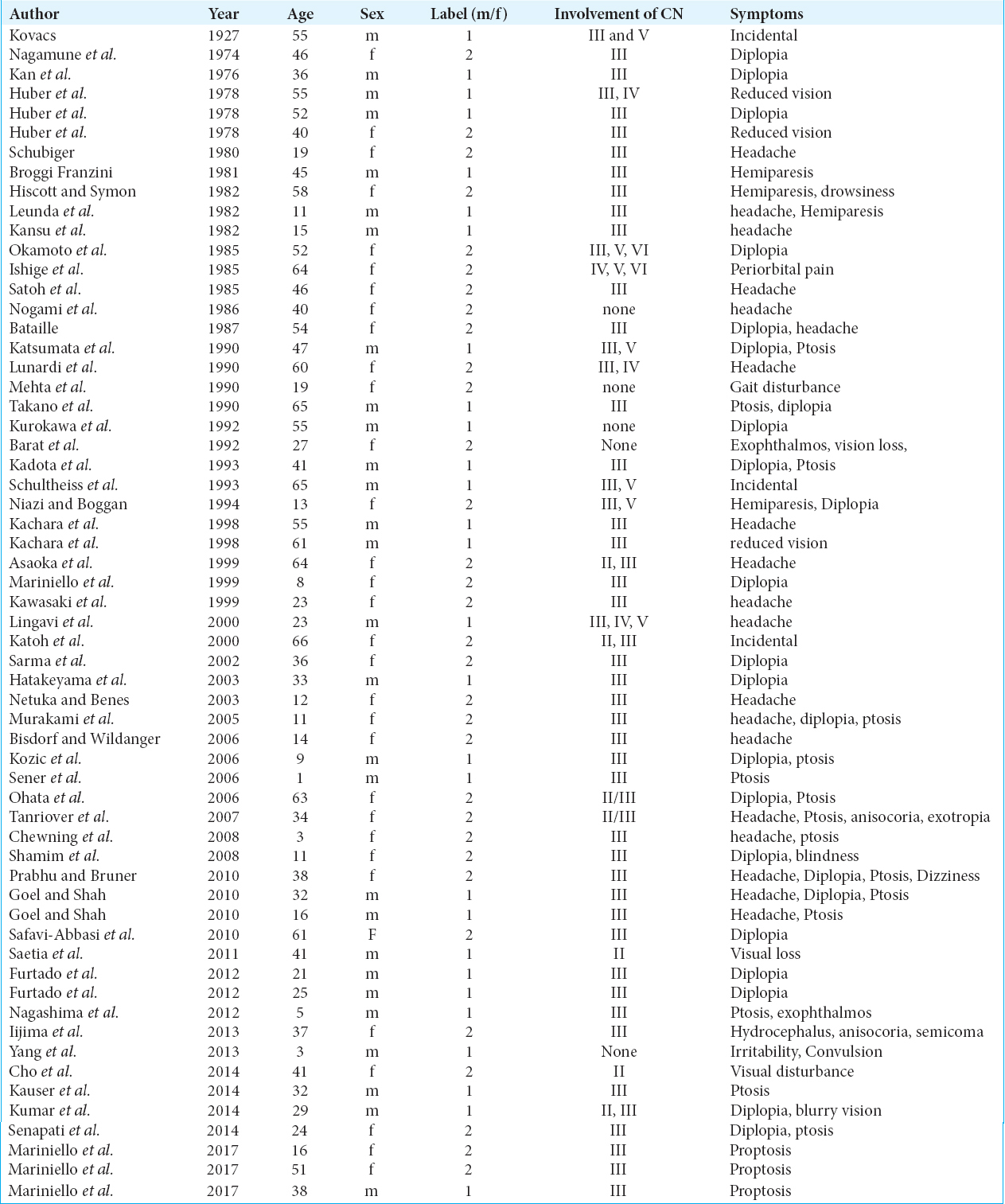
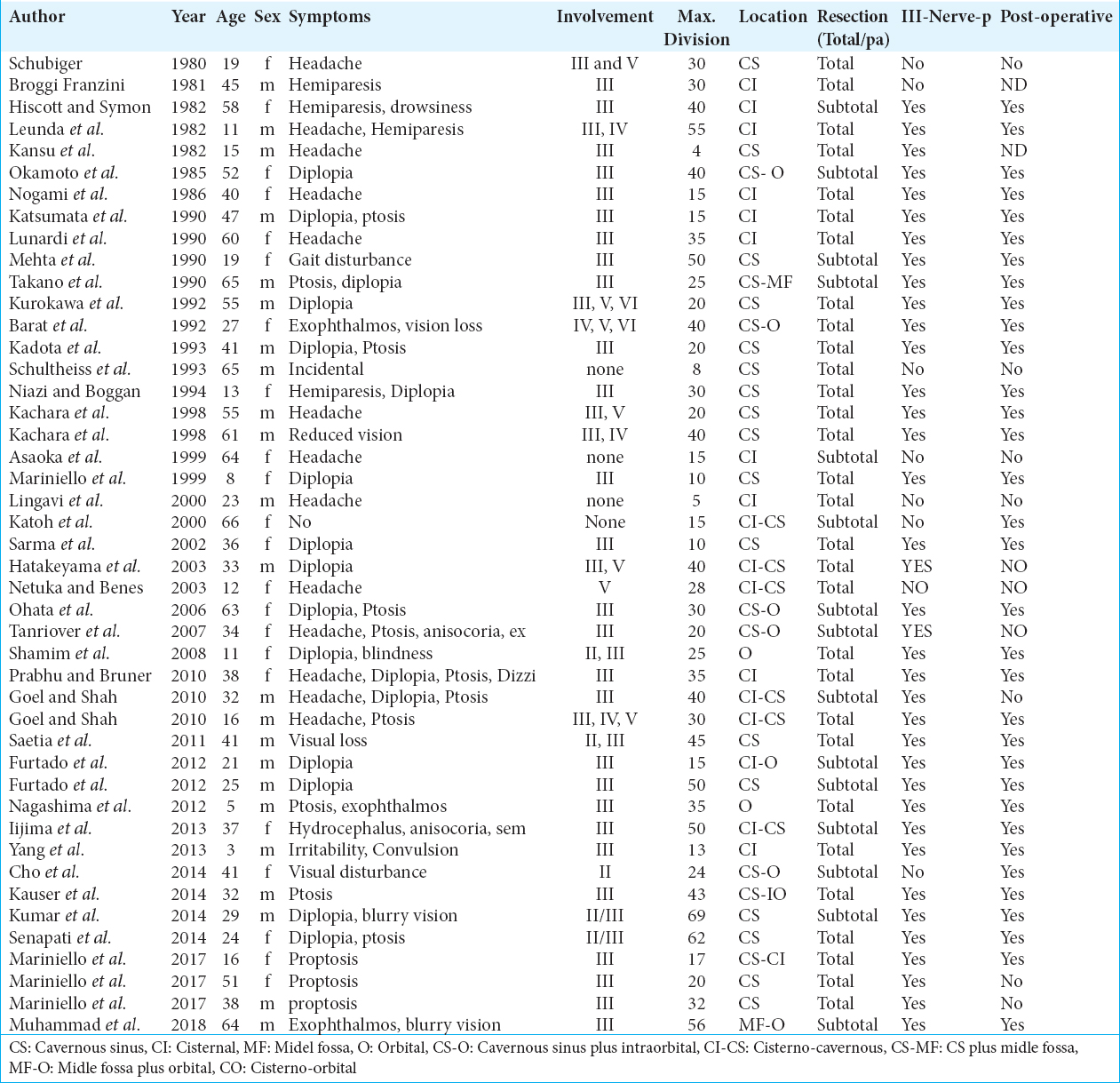
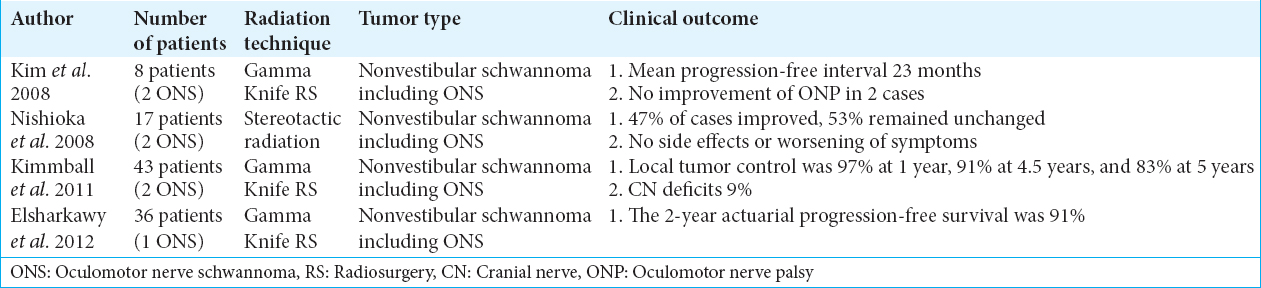
Results: Till date, there are 60 reported cases of ONS (45 treated surgically and seven radiosurgically) with the dominance of female gender (53%) and mean age of 35.2 years (Range 1–66). In 8% of the cases, there was no involvement of cranial nerve (CN) III and 92% of the cases CN III alone or together with CN II, IV, V, and VI. In 67% of the cases a complete resection and 33% a partial resection performed. In 73% of the cases, postoperative third nerve palsy was documented, 22% improved after surgery and in around 5% of cases, the outcome was not described. In the radiosurgically treated cases of nonvestibular schwannoma including ONS, the progression-free interval of approximately 2 years was above 90%.
Conclusion: Due to the high rate of postoperative complete oculomotor nerve palsy, a subtotal resection avoiding the nerve injury seems to be a feasible option. Radiosurgery is another option to treat small size schwannoma. A combined treatment with microsurgery followed by radiosurgery may allow effective treatment for large size oculomotor schwannoma.
Keywords: Clinical outcome, microsurgery, oculomotor nerve schwannoma, radiosurgery
INTRODUCTION
Intracranial schwannoma accounts for around 7% of all intracranial tumors.[
Till date, around five dozens of cases of ONS have been reported in literature. Most of the cases reported in the literature have been treated surgically with a very high rate of complete third nerve palsy that adds significant morbidity. Although radiosurgery could be an alternative, only a few successfully treated cases with radiosurgery have been reported in literature.[
Hence, we review surgically and radiosurgically treated cases and morbidity reported in these cases and discusses alternative options to treat these tumors. Furthermore, we present an illustrative case of ONS treated surgically in our department.
MATERIALS AND METHODS
Case report
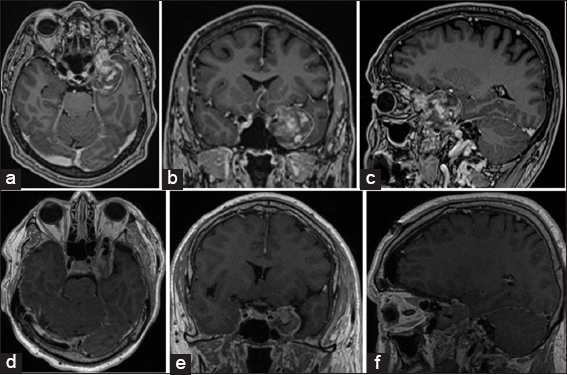
A 64-years-old male presented with a history of exophthalmos and blurry vision on the left side for 3 years. On examination, the patient was alert and oriented to all qualities. Visual field was intact and pupil size was normal and reactive to light. The patient showed a slight restriction of ocular movements as a sign of partial oculomotor palsy. Magnetic resonance imaging (MRI) scan showed a 5.6 cm contrast enhancing lesion on the left orbital apex with extension in the middle fossa [
LITERATURE REVIEW
Review of literature for cases of ONS that were treated with surgery was performed using PubMed, Ovid Medline, and Scopus database. We used the PRISMA checklist as a guide to achieve accepted standards for reporting system reviews. The first author performed all steps and discussed with senior author.
We used keywords “oculomotor nerve” in combination with “schwannoma” and “surgery” or “radiosurgery.” A total of 141 related articles were yielded. Articles in nonEnglish language were excluded. The articles without any kind of treatment were also excluded. Finally, 60 articles were considered suitable for review.
RESULTS
Surgical resection and operative findings
After exclusion of irrelevant articles according to above-mentioned exclusion criteria, 60 articles were considered to be included in our analysis. We analyzed age, size, location of schwannoma, involvement of CNs, extent of surgical resection, and the third nerve palsy after surgery. The analysis of data from included articles showed that oculomotor schwannoma is slightly more in female gender (53%) and mean age of 35.2 years (standard deviation = 19.5, range 1–66). In 8% of the cases there was no involvement of CN III and 92% of the cases there was either CN III alone or together with CN II, IV, V, and VI affected [
Postoperative outcome
Postoperatively patient developed complete oculomotor nerve palsy with ptosis and dilated the fixed pupil. On discharge from the hospital a slight recovery with almost normalized pupil size was observed. In the short-term follow-up of 3 months the partial recovery with normalized and to the light reactive pupil and a partial recovery of ptosis (could open the eye around 1 cm) was documented.
DISCUSSION
ONSs are slow growing rare tumors. There is no standard treatment strategy for such a tumor. Hence, we reviewed the existing literature for treatment modality and reported the outcome. ONS is located at the course of nerve either in cisternal (CI) space, cisterno-cavernous region, orbital apex and rarely in the orbita [
Due to benign nature of the tumor, a maximum resection of the tumor is the surgical goal. However, the oculomotor nerve is very fragile and can be easily injured in an attempt to complete tumor removal. Most of the surgically treated cases showed postoperative complete third nerve palsy [
CONCLUSION
Due to the high rate of postoperative complete oculomotor nerve palsy, a subtotal resection avoiding the nerve injury seems to be a feasible option. Radiosurgery is another option to treat small size schwannoma. A combined treatment with microsurgery followed by radiosurgery may allow effective treatment for large size oculomotor schwannoma.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the Ethical Standards of the Research Committee of University of Helsinki and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
We are thankful to Ehrnrooth Foundation for the Funding to SM for a clinical vascular and skull base fellowship at the Department of Neurosurgery in Helsinki.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge the support from Ehrnrooth Foundation for the clinical fellowship to Dr. S.Muhammad.
References
1. Asaoka K, Sawamura Y, Murai H, Satoh M. Schwannoma of the oculomotor nerve: A case report with consideration of the surgical treatment. Neurosurgery. 1999. 45: 630-3
2. Cho YH, Sung KS, Song YJ, Kim DC, Choi S, Kim KU. Oculomotor nerve schwannoma: A case report. Brain Tumor Res Treat. 2014. 2: 43-7
3. Elsharkawy M, Xu Z, Schlesinger D, Sheehan JP. Gamma knife surgery for nonvestibular schwannomas: Radiological and clinical outcomes. J Neurosurg. 2012. 116: 66-72
4. Iijima K, Tosaka M, Nagano T, Yaoita H, Matsumura N, Nakazato Y. Oculomotor nerve schwannoma associated with acute hydrocephalus: Case report. Neurol Med Chir (Tokyo). 2014. 54: 654-8
5. Katoh M, Kawamoto T, Ohnishi K, Sawamura Y, Abe H. Asymptomatic schwannoma of the oculomotor nerve: Case report. J Clin Neurosci. 2000. 7: 458-60
6. Kim IY, Kondziolka D, Niranjan A, Flickinger JC, Lunsford LD. Gamma knife surgery for schwannomas originating from cranial nerves III, IV, and VI. J Neurosurg. 2008. 109: 149-53
7. Kimball MM, Foote KD, Bova FJ, Chi YY, Friedman WA. Linear accelerator radiosurgery for nonvestibular schwannomas. Neurosurgery. 2011. 68: 974-84
8. Mariniello G, Horvat A, Dolenc VV. En bloc resection of an intracavernous oculomotor nerve schwannoma and grafting of the oculomotor nerve with sural nerve. Case report and review of the literature. J Neurosurg. 1999. 91: 1045-9
9. Newton HB. Primary brain tumors: Review of etiology, diagnosis and treatment. Am Fam Physician. 1994. 49: 787-97
10. Nishioka K, Abo D, Aoyama H, Furuta Y, Onimaru R, Onodera S. Stereotactic radiotherapy for intracranial nonacoustic schwannomas including facial nerve schwannoma. Int J Radiat Oncol Biol Phys. 2009. 75: 1415-9
11. Sarma S, Sekhar LN, Schessel DA. Nonvestibular schwannomas of the brain: A 7-year experience. Neurosurgery. 2002. 50: 437-48
12. Tanriover N, Kemerdere R, Kafadar AM, Muhammedrezai S, Akar Z. Oculomotor nerve schwannoma located in the oculomotor cistern. Surg Neurol. 2007. 67: 83-8