- Department of Neurosurgery, Center for Research and Training in Neurosurgery, Samaritana University Hospital, Rosario University School of Medicine, Bogotu, Colombia.
DOI:10.25259/SNI_357_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Francisco Perez-Pinto, Juan Felipe Abaunza-Camacho, David Vergara-Garcia, Camilo Benavides, William Mauricio Riveros, Leonardo Laverde. Management of recurrent schwannoma of the cauda equina: A case report. 28-Jun-2021;12:312
How to cite this URL: Francisco Perez-Pinto, Juan Felipe Abaunza-Camacho, David Vergara-Garcia, Camilo Benavides, William Mauricio Riveros, Leonardo Laverde. Management of recurrent schwannoma of the cauda equina: A case report. 28-Jun-2021;12:312. Available from: https://surgicalneurologyint.com/surgicalint-articles/10924/
Abstract
Background: Schwannomas of the cauda equina are rare intradural primary spinal tumors. Many of these patients initially present with cauda equina syndromes, and only 2.2% demonstrate clinical recurrence. Gross total excision is the procedure of choice.
Case Description: A 62-year-old female had undergone resection of a cauda equina schwannoma 5 years previously. She newly presented with cauda equina symptoms attributed to a recurrent schwannoma. Following gross total secondary tumor resection, the patient’s preoperative deficits fully resolved, and the tumor never recurred.
Conclusion: Secondary gross total excision of schwannomas of the cauda equina is critical to avoid further tumor recurrence.
Keywords: Cauda equine, Gross total excision, Intradural tumor, Schwannoma, Tumor recurrence
INTRODUCTION
Spinal schwannomas represent 20% of primary tumors of the spinal cord.[
CASE REPORT
A 62-year-old female who had undergone prior subtotal resection of a schwannoma of the cauda equina (5 years ago) newly presented with a 3-month history of low-back pain/dysesthesias radiating into her right lower extremity, anesthesia in her perineal region, and urinary retention. Her lower extremity examination revealed a partial paresis (4/5), hyporeflexia, and hypoesthesia of the lower limbs and perineal region.
Magnetic resonance (MR) study
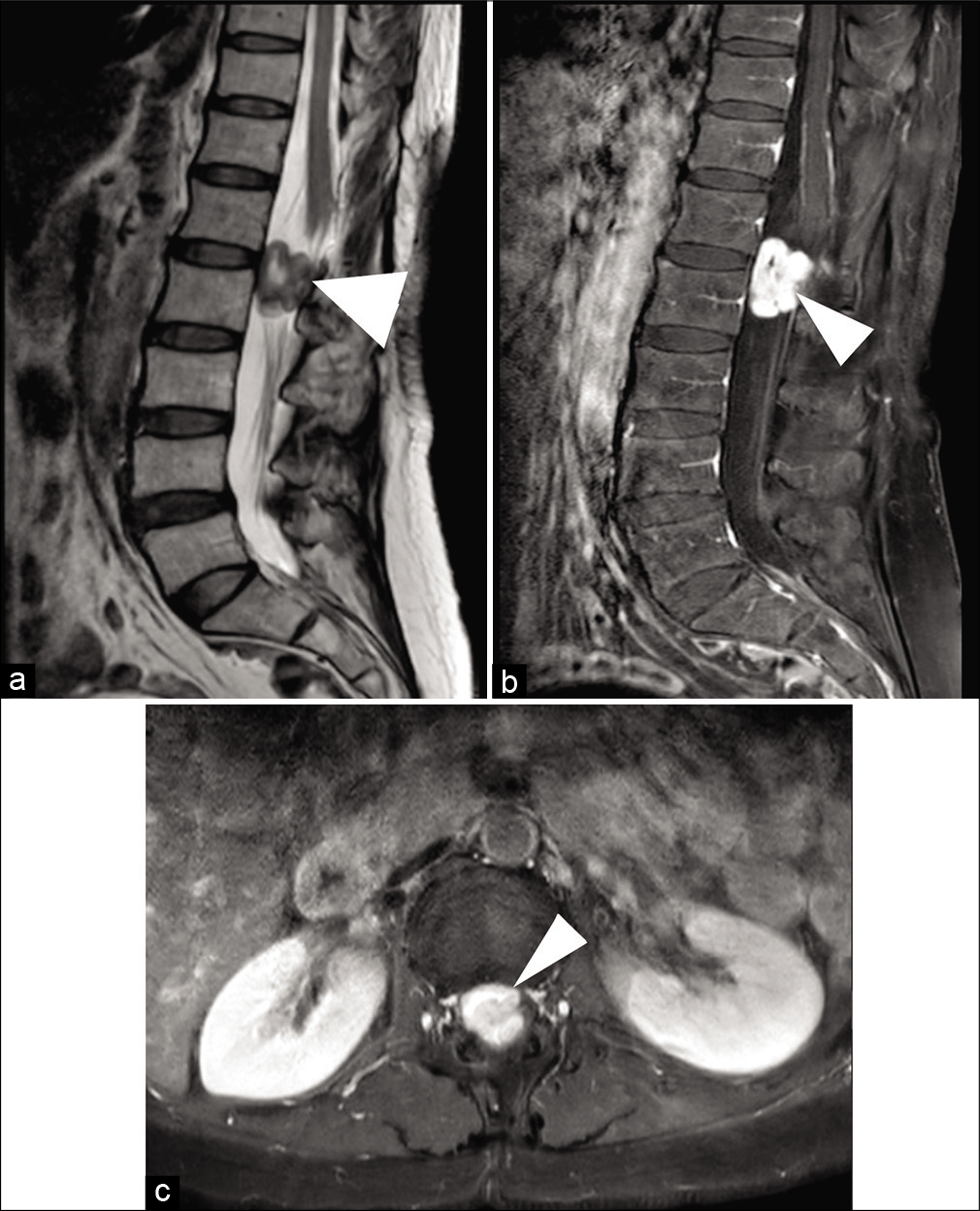
A gadolinium-enhanced MR imaging (MRI) documented an intradural extramedullary solid lesion with marked gadolinium enhancement extending from L1 to L2, resulting in anterior compression/displacement of the cauda equina/ conus medullaris [
Figure 1:
(a and b) Midsagittal view of a T2-weighted (a) and a contrast-enhanced T1-weighted (b) magnetic resonance imaging (MRI) of the lumbar spine demonstrating an intradural extramedullary spinal lesion (white arrowhead) from L1 to L2 with avid contrast enhancement. (c) Axial view of a contrast-enhanced T1-weighted MRI of the lumbar spine demonstrating high-grade compression of conus medullaris and cauda equina from an intradural extramedullary lesion (white arrowhead).
She underwent bilateral laminectomies of L1-L2; following the durotomy, a well-defined (14 × 20 × 22 mm) solid yellowish lesion was visualized adjacent to the filum terminale; it was completely resected. Neuromonitoring potentials and electromyography remained unchanged. Next, a T11-L3 transpedicular screw-rod system was used to prevent mechanical instability in the thoracolumbar junction because of the multiple laminectomies performed at this level.
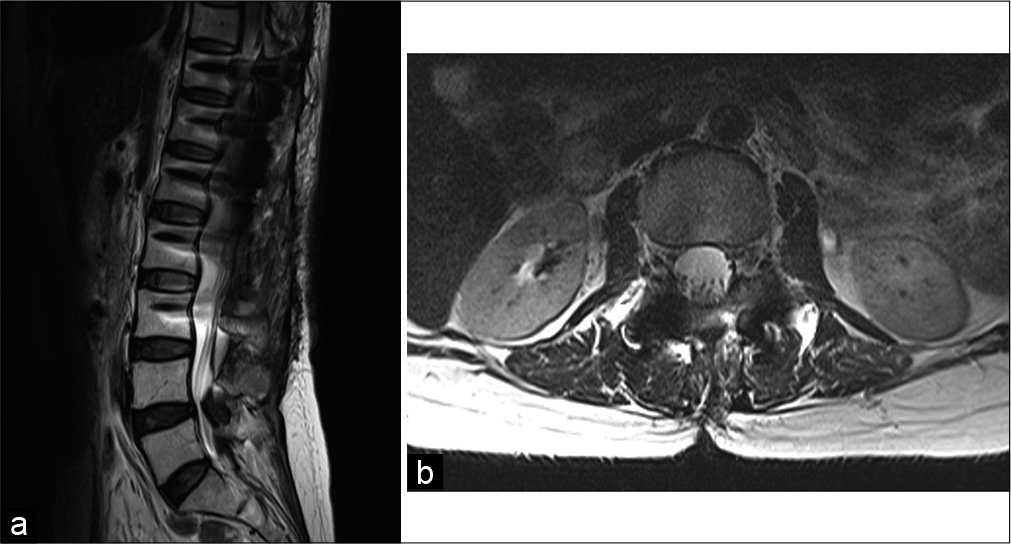
She was discharged three days postoperatively, having regained full neurological function except for residual hypoesthesia in the perineal region. In addition, the postoperative MRI scans confirmed complete tumor removal [
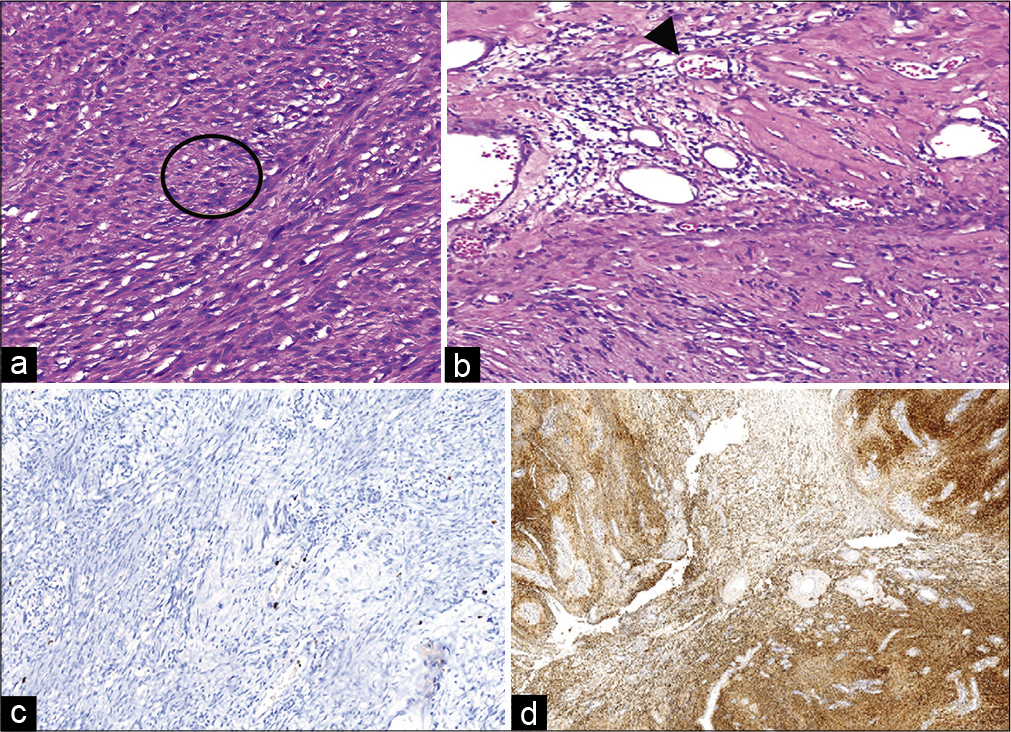
Pathology
Pathology revealed a fusocellular tumor that was compatible with the diagnosis of a schwannoma of the cauda equina [
DISCUSSION
Primary tumors from the spinal cord, spinal meninges, and cauda equina account for only 4.5% of all primary central nervous system tumors; the cauda equina is involved in 5.3% of these lesions.[
MRI findings on T1 and T2-weighted MRI comprise T2 heterogeneous hypointensity, T1 heterogeneous hyperintensity, and marked contrast enhancement of the lesion.[
The main goal of treatment for schwannomas is complete surgical resection of the lesion. However, subtotal resection is obtained in one-fifth of the cases.[
CONCLUSION
Primary and recurrent schwannomas of the cauda equina should optimally undergo gross total excision to prevent tumor recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asazuma T, Toyama Y, Watanabe M, Suzuki N, Fujimura Y, Hirabayashi K. Clinical features associated with recurrence of tumours of the spinal cord and cauda equina. Spinal Cord. 2003. 41: 85-9
2. Chin AL, Fujimoto D, Kumar KA, Tupper L, Mansour S, Chang SD. Long-term update of stereotactic radiosurgery for benign spinal tumors. Clin Neurosurg. 2019. 85: 708-16
3. Engelhard HH, Villano JL, Porter KR, Stewart AK, Barua M, Barker FG. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equina: Clinical article. J Neurosurg Spine. 2010. 13: 67-77
4. Fujii K, Abe T, Koda M, Funayama T, Noguchi H, Miura K. Cauda equina schwannoma with concomitant intervertebral disc herniation: A case report and review of literature. J Clin Neurosci. 2019. 62: 229-31
5. Kagaya H, Abe E, Sato K, Shimada Y, Atushi KM. Giant cauda equina schwannoma. Encycl Neurol Sci. 2014. 25: 613-3
6. Kimura R, Miyakoshi N, Suzuki T, Kido T, Chiba M, Kobayashi T. Traumatic intratumoral hemorrhage of schwannoma of the cauda equina: A report of two cases. J Orthop Sci. 2018. 23: 1105-9
7. Piek J. Giant schwannoma of the cauda equina without neurological deficits case report and review of the literature. Wien Klin Wochenschr. 2010. 122: 645-8
8. Wager M, Lapierre F, Blanc JL, Listrat A, Bataille B. Cauda equina tumors: A French multicenter retrospective review of 231 adult cases and review of the literature. Neurosurg Rev. 2000. 23: 119-29