- Departments of Neurosurgery, Sydney Childrens Hospital, Randwick, New South Wales, Australia.
- Departments of Interventional Neuroradiology, Sydney Childrens Hospital, Randwick, New South Wales, Australia.
Correspondence Address:
Jeremy Rajadurai
Departments of Interventional Neuroradiology, Sydney Childrens Hospital, Randwick, New South Wales, Australia.
DOI:10.25259/SNI_33_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jeremy Rajadurai, Saeed Kohan, Jason Wenderoth. Management of spinal dural arteriovenous fistula in a child with myelopathy. 02-May-2020;11:91
How to cite this URL: Jeremy Rajadurai, Saeed Kohan, Jason Wenderoth. Management of spinal dural arteriovenous fistula in a child with myelopathy. 02-May-2020;11:91. Available from: https://surgicalneurologyint.com/surgicalint-articles/9990/
Abstract
Background: Spinal dural arteriovenous fistulas (DAVF) are rare intradural spinal lesions. Patients with DAVF are typically in the 40’s or 50’s, and classically present with acute neurological deterioration. Notably, these lesions are exceedingly rare in the pediatric age group.
Case Description: A 2-year-old child presented with the sudden onset of lethargy, and 4/5 weakness of the left lower extremity with accompanying ataxia. The cervicothoracic MR scan revealed central cord edema from C5 to T4. A DAVF was diagnosed based on the multiple dilated intradural perimedullary veins. Following endovascular treatment, the child markedly recovered and remained stable 2 years later.
Conclusion: DAVFs are treatable lesions that rarely occur in the pediatric age group. They are associated with serious neurological morbidity. When suspected, they should be immediately diagnosed with magnetic resonance imaging/magnetic resonance angiography, and formal angiography. Prompt neurosurgical and neuroradiological/ endovascular opinions and intervention should be sought to provide and the best treatment strategy.
Keywords: Dural arteriovenous fistula pediatric, Dural arteriovenous malformation paediatric, Spinal myelopathy
INTRODUCTION
Spinal vascular malformations comprise 3–4% of all intradural lesions.[
CASE REPORT
Clinical presentation with cervical and thoracic MR/magnetic resonance angiography
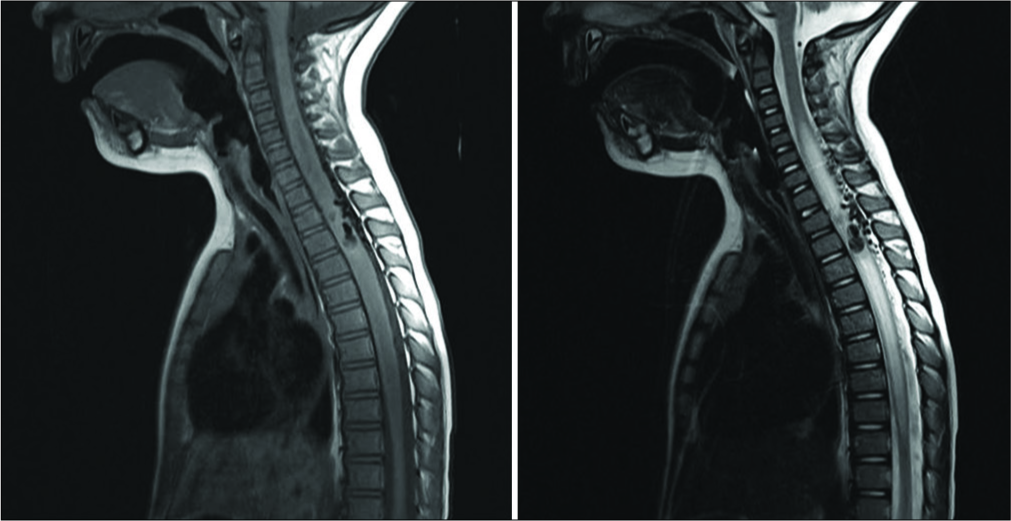
A 2-year-old female presented with the sudden onset of lethargy, gait ataxia, and paresis in the left leg. On examination, she exhibited focal 4/5 motor weakness in the left lower extremity. The cervical and thoracic MR studies revealed a vascular malformation with venous congestion and central cord edema extending from C5 to T4. There were multiple accompanying dilated intradural perimedullary veins [
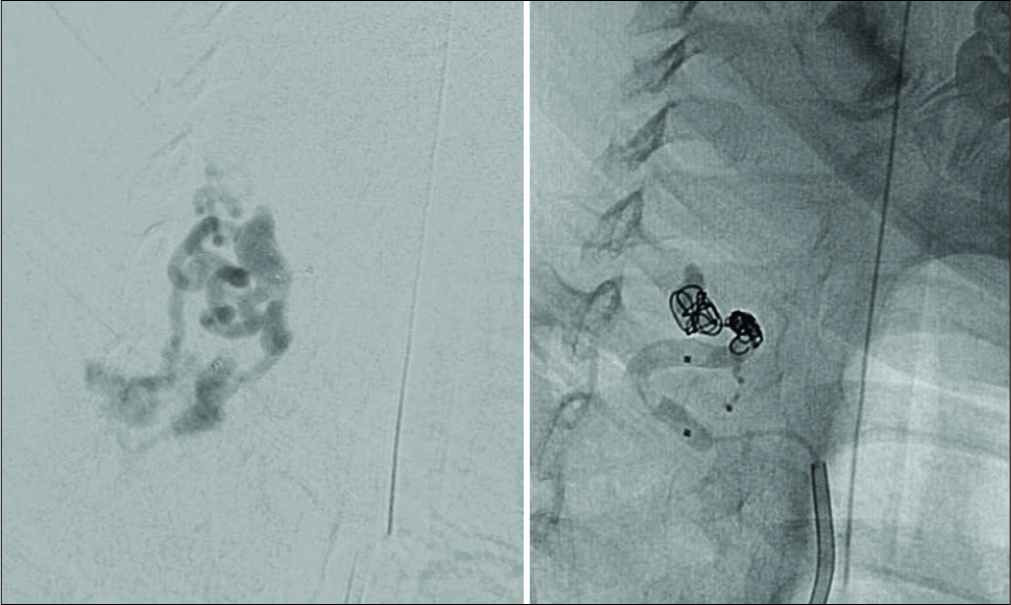
Digital subtraction angiography (DSA) and coiling/ embolization of DAVF
DSA showed a large feeding vessel on the left at the T6 level; this was supplied by a single “hole fistula” extending through the left T3/4 foramen and was accompanied by a venous “side” aneurysm [
2-year follow-up
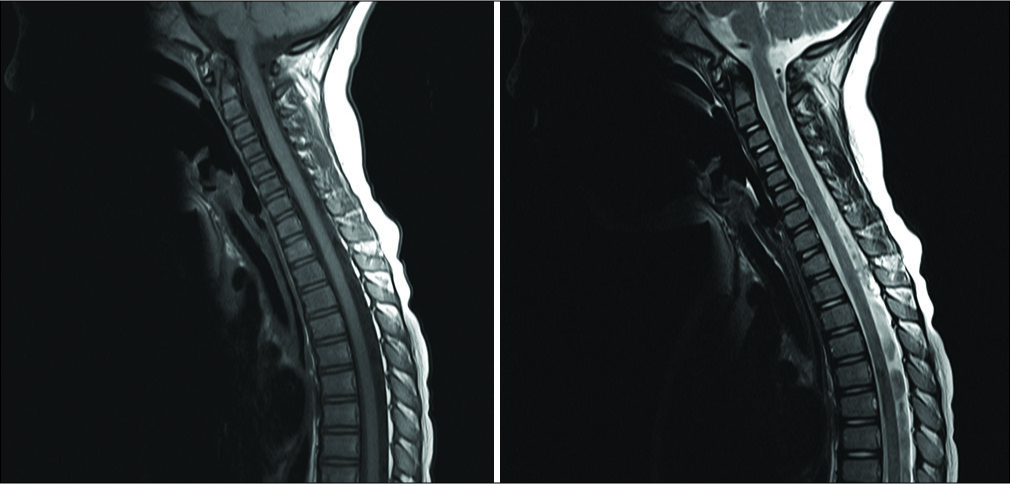
Two years following embolization, the child was mobilizing independently and had a normal neurological examination. The subsequent DSA 12 months later showed no residual DAVF. Further, the magnetic resonance imaging (MRI) showed no recurrence, and the resolution of cord edema [
DISCUSSION
Historical and clinical presentation of pediatric spinal DAVF
Spinal DAVFs differ in their anatomical location, size, and etiology. Intradural DAVFs usually affect the spinal cord, nerve roots or filum terminale, and typically link dural branches of radicular arteries with radiculomedullary veins.[
History of DAVF’s
There is currently limited literature regarding the natural history of spinal DAVFs in children.[
MR identification of spinal DAVF
Pediatric spinal DAVFs are easily identifiable on MRI scans. They typically show resultant cord edema intrinsic cord signal changes over multiple levels[
Use of DSA (angiography) for diagnosis/documentation of DAVF
DSA remains the gold standard for DAVF imaging. Classically, intradural DAVFs show dilated perimedullary or intramedullary vasculature with deformation of the cord. Angiography also facilitates the reconstruction of these lesions for treatment planning, along with the identification of critical vessels such as the artery of Adamkiewicz.[
Endovascular versus surgical treatment of DAVF
DAVFs can be treated endovascularly or surgically. Endovascular treatment may involve embolization with coils in conjunction with utilization of liquid embolic agents. Where endovascular treatment has failed, surgery may be warranted to close the shunt (e.g., by clipping, coagulating, and securing the exit intradural vein).[
Genetic predisposition
As spinal DAVFs can be associated with inherited and/or genetic disorders, referral to geneticists should be discussed with the child’s parents or caregivers.[
CONCLUSION
Spinal DAVFs are rare and are often difficult to diagnose in the pediatric population. Notably, DAVF’s should be considered when children exhibit acute neurological deterioration. MRI and DSA should be performed with careful attention given to discerning whether these lesions can be embolized/coiled versus surgically managed.
Statement of ethics
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The parent of the subject presented has given their written consent to publish this case (including images).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Berenstein A.editors. Spinal Cord Arteriovenous Malformations. New York: Springer Verlag; 1992. p.
2. Du J, Ling F, Chen M, Zhang H. Clinical characteristic of spinal vascular malformation in pediatric patients. Childs Nerv Syst. 2009. 25: 473-8
3. Flores BC, Klinger DR, White JA, Batjer HH. Spinal vascular malformations: Treatment strategies and outcome. Neurosurg Rev. 2017. 40: 15-28
4. Hurst RW, Kenyon LC, Lavi E, Raps EC, Marcotte P. Spinal dural arteriovenous fistula: The pathology of venous hypertensive myelopathy. Neurology. 1995. 45: 1309-13
5. Hurth MH, Djindjina R, Rey A, Djindjian M. Arteriovenous malformations of the spinal cord. Clinical, anatomical and therapeutic considerations: A series of 150 cases5. Progr Neurol Surg. 1978. 9: 238-66
6. Jeng Y, Chen DY, Hsu HL, Huang YL, Chen CJ, Tseng YC. Spinal dural arteriovenous fistula: Imaging features and its mimics. Korean J Radiol. 2015. 16: 1119-31
7. Miyasaka K, Asano T, Ushikoshi S, Hida K, Koyanagi I. Vascular anatomy of the spinal cord and classification of spinal arteriovenous malformations. Interv Neuroradiol. 2000. 6: 195-8
8. Morris JM. Imaging of dural arteriovenous fistula. Radiol Clin North Am. 2012. 50: 823-39
9. Niimi Y, Berenstein A, Setton A, Neophytides A. Embolization of spinal dural arteriovenous fistulae: Results and follow-up. Neurosurgery. 1997. 40: 675-82
10. Rangel-Castilla L, Russin JJ, Zaidi HA, Martinez-Del-Campo E, Park MS, Albuquerque FC. Contemporary management of spinal AVFs and AVMs: Lessons learned from 110 cases. Neurosurg Focus. 2014. 37: E14-
11. Rodesch GH, Alvarez H, Ducot B, Tadie M, Lasjaunias P. Angio-architecture of spinal cord arteriovenous shunts at presentation. Clinical correlations in adults and children. Acta Neurochirur. 2004. 146: 217-27
12. Rodesch G, Lasjaunias P. Spinal cord arteriovenous shunts: From imaging to management. Eur J Radiol. 2003. 46: 221-32
13. Van Dijk JM, TerBrugge KG, Willinsky RA, Farb RI, Wallace MC. Multidisciplinary management of spinal dural arteriovenous fistulas: Clinical presentation and long-term follow-up in 49 patients. Stroke. 2002. 33: 1578-83
14. Willinsky R, Lasjaunias P, Terbrugge K, Hurth M. Angiography in the investigation of spinal dural arteriovenous fistula. A protocol with application of the venous phase. Neuroradiology. 1990. 32: 114-6