- Division of Neurosurgery, Department of Neurosciences, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_290_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Turki Elarjani, Meshari Alhuthayl, Maher Hassounah. Massive Secondary Cutaneous Meningioma with Extension to the Face. 25-Jul-2020;11:209
How to cite this URL: Turki Elarjani, Meshari Alhuthayl, Maher Hassounah. Massive Secondary Cutaneous Meningioma with Extension to the Face. 25-Jul-2020;11:209. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10156
Abstract
Background: Cutaneous meningioma is a very uncommon pathologic entity that can be divided into primary and secondary types. Secondary cutaneous meningioma arises from an intracranial meningioma through metastasis, seeding during surgery, or direct bone invasion. There are limited published case reports correlating the development of cutaneous meningioma to high-grade convexity meningioma.
Case Description: A 63-year-old man underwent total resection of a right frontal convexity meningioma, World Health Organization Grade I in 2001. He presented in 2016 with a small frontal cutaneous mass over the craniotomy site. Computed tomography showed extracranial and intracranial components of the meningioma. The patient declined surgical intervention and lost to follow. One and half years later, he underwent resection of the growing ulcerating cutaneous component in an outside hospital. The pathological diagnosis was Grade 3 meningioma. Six months later, he presented to us with a massive cutaneous meningioma and large intracranial component. Surgical resection and multidisciplinary management were planned. The patient was very hesitant to have surgery but settled for receiving radiation. Seven months after radiation, he presented with a decreased level of consciousness and skin necrosis with maggot infestation. His code status was changed to “do not attempt resuscitation,” and he died 3 days later in December 2019.
Conclusion: Large intracranial meningiomas with massive transosseous extension to the scalp pose a significant challenge to the treating team. Proper planning and a multidisciplinary approach are essential. However, prognosis remains generally poor.
Keywords: Cutaneous meningioma, Extracranial meningioma, Secondary scalp meningioma
INTRODUCTION
Meningioma is a tumor arising from arachnoid cap cells of the meninges and usually has a dural base. According to the World Health Organization (WHO,) meningiomas are classified into three grades: Grade I is benign, Grade II is atypical, and Grade III is malignant. Extracranial cutaneous meningioma is a rare entity and can be divided into primary and secondary.[
CASE DESCRIPTION
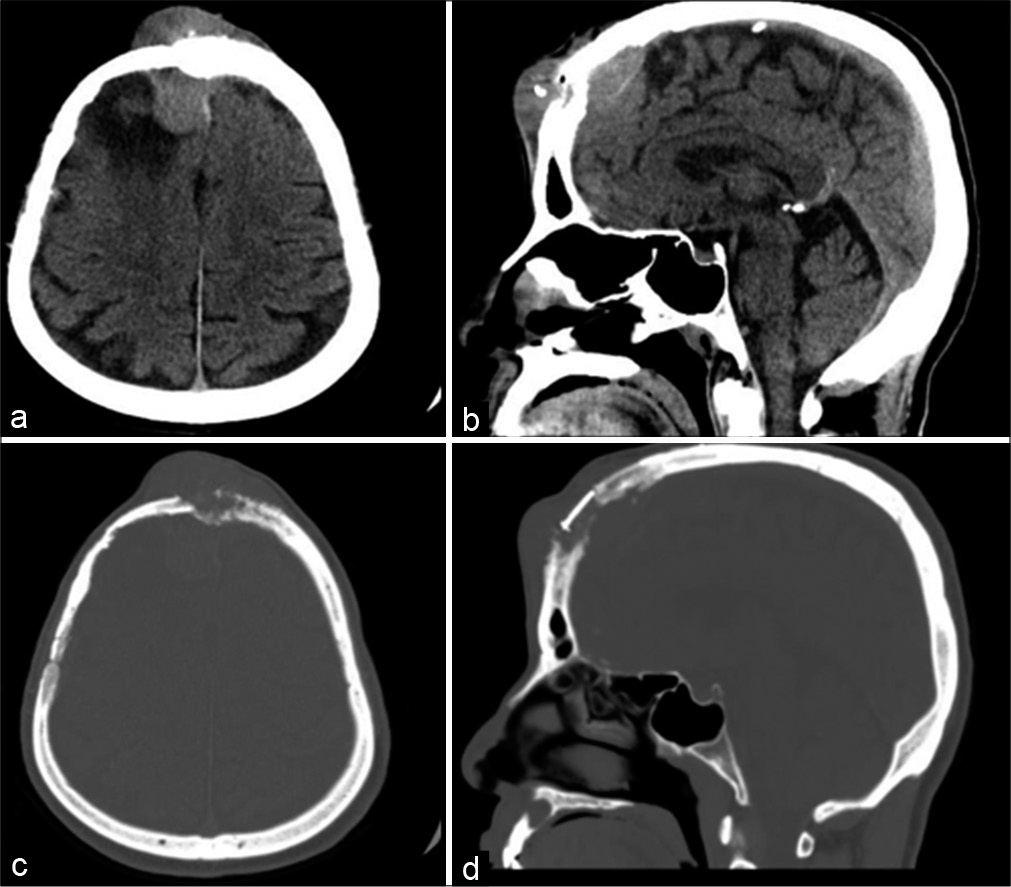
The patient is a 63-year-old man who underwent total resection of a 4.6 cm×4.6 cm×5.5 cm right frontal convexity meningioma in 2001. The tumor showed multiple calcified nodules, and there was focal erosion of the inner table of the skull. There were no surrounding edema and no sinus invasion. The pathology was meningothelial meningioma WHO Grade I. He was followed for 30 months with no tumor recurrence, then he lost to follow up until he presented to our clinic in 2016 with a 2-month history of mid-forehead swelling measuring 5 cm × 5 cm in that was hard and firm. Computed tomography (CT) showed midline and right frontal recurrence of intracranial meningioma with a cutaneous component eroding the craniotomy flap and extending to the scalp [
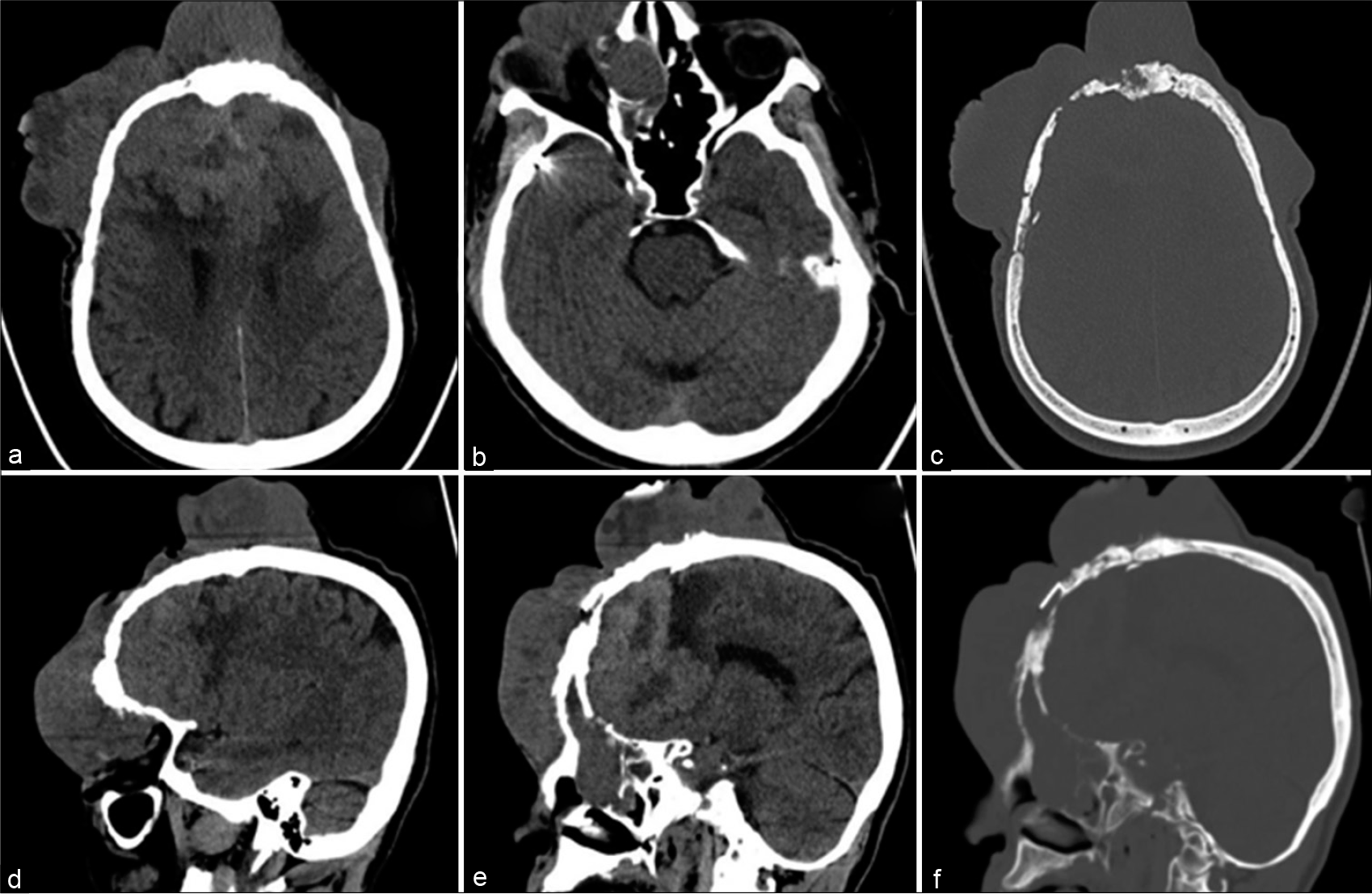
In 2018, the patient presented to a local hospital with a large ulcerating scalp tumor. He underwent surgical excision of the extracranial tumor component that showed WHO Grade III meningioma. The patient refused resection of the intracranial component and radiation therapy thereafter. Six months later, he presented to our emergency department with a massive face and bifrontal cutaneous mass that displaced his right eye inferiorly and laterally [
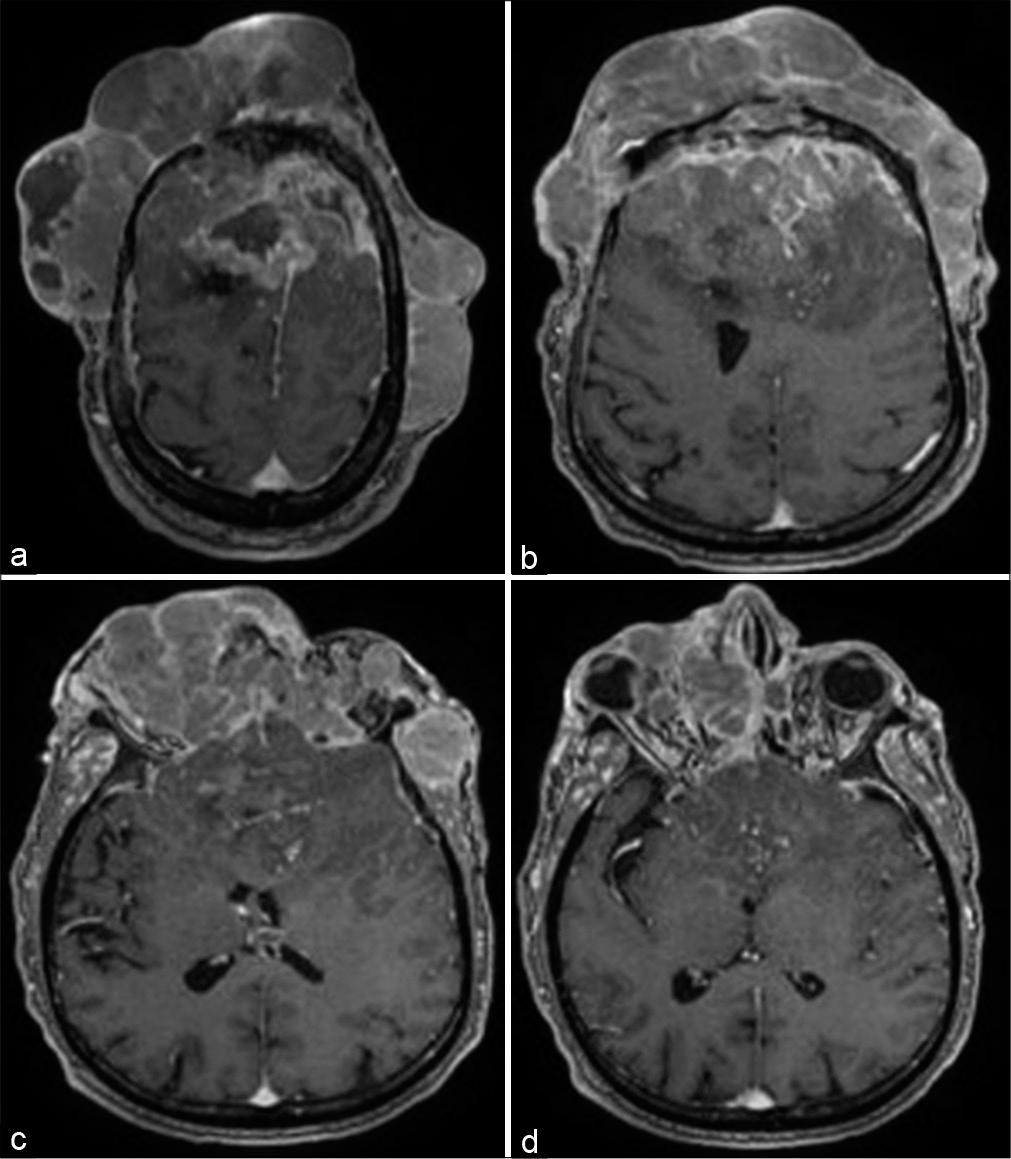
Figure 4:
(a-c) Axial magnetic resonance imaging with contrast from the vertex till the basal ganglia showing significant intracranial component with bilateral frontal dural attachment and severe mass effect on the frontal lobes and lateral ventricles bilaterally. The right superomedial invasion of the orbital cavity is appreciated (d).
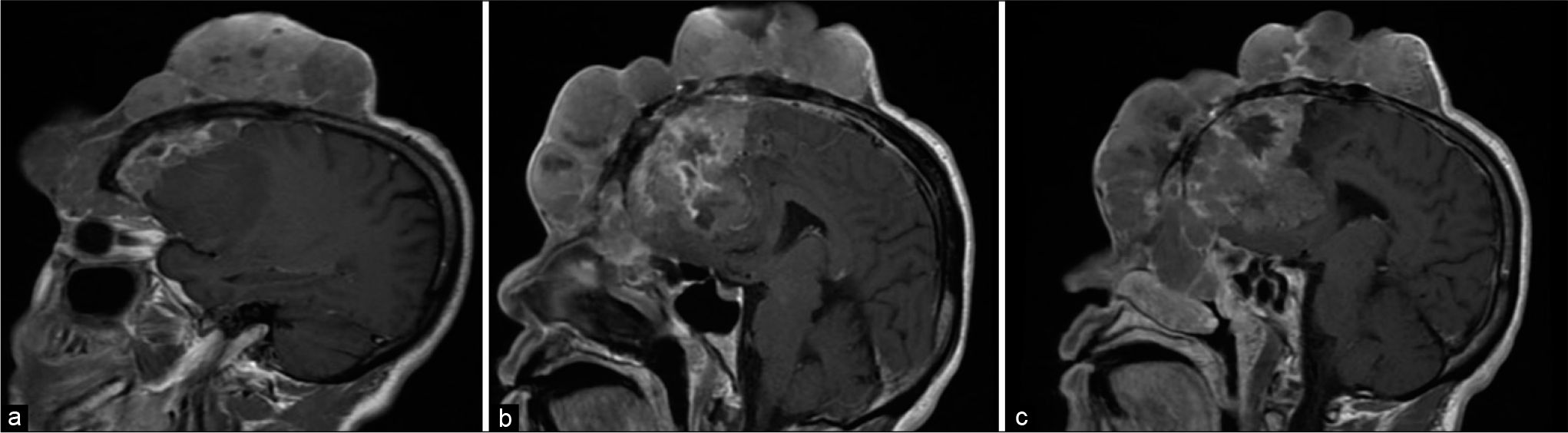
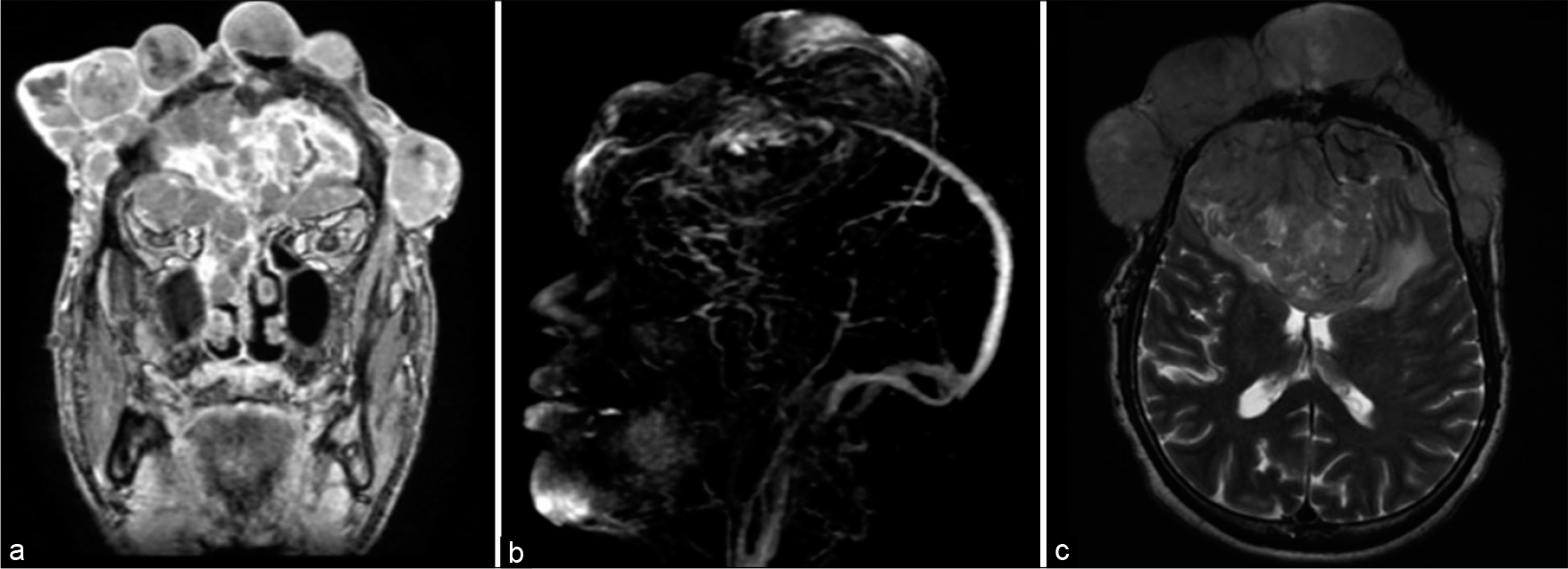
Figure 6:
Coronal magnetic resonance imaging with contrast showing the lateral extent of the cutaneous component (a). Magnetic resonance venography showing complete occlusion of the anterior and middle thirds of the superior sagittal sinus (b). Axial T2 image showing the vasogenic edema surrounding the intracranial component (c).
Plastic surgery, maxillofacial surgery, ophthalmology, and radiation oncology teams were consulted. The plan was to resect the intracranial and extracranial parts of the tumor then reconstruct the anterior skull base and calvarium. The major challenge was the skin coverage after resection. The patient and his family were unwilling to undergo major surgery, but they accepted receiving radiation therapy. He received 54 Grays in 30 fractions. Moderate shrinkage of the tumor was observed after the conclusion of radiation. He missed his follow-up appointments, then he showed 7 months later in our emergency room with a decreased level of consciousness for 5 days with a Glasgow Coma Scale of 9/15 (motor 5, eye 2, and verbal 2). In addition, there were multiple scalp ulcerations with maggot infestation of the wound. The wound was debrided and cleaned. The patient’s code status was changed to do not attempt resuscitation, and he passed away 3 days later in December 2019.
DISCUSSION
Secondary cutaneous or scalp meningioma is an uncommon entity related to metastasis, seeding during surgical resection of intracranial meningioma, or extension of an intracranial component.[
The reported incidence in the literature ranges from 1.21% to 3%.[
There are 15 reported cases with secondary cutaneous meningioma in the literature.[
Multiple risk factors were hypothesized based on a literature review article. Multiple reoperations, radiation therapy, wound complication, immune suppression, higher histological grade, and cerebrospinal fluid fistula are risk factors in developing secondary cutaneous meningioma.[
Our patient possibly had a higher grade meningioma when he first noticed a small frontal lump on the craniotomy site. Radiation therapy is known to interfere with wound healing and causes skin atrophy; our patient had skin necrosis with maggot infestation 7 months after radiation therapy. In general, the management of cutaneous meningioma is complete surgical resection of the cutaneous and intracranial component, with the removal of the affected bone and adjacent normal bone to lower the recurrence rate.[
CONCLUSION
Secondary cutaneous meningioma is a rare pathological entity that is mostly associated with Grade II or Grade III meningiomas. Complex cases should undergo proper planning and management by different disciplines. Complete excision of both intracranial and extracranial components and cranial reconstruction are the mainstays of management. Precautionary measures should be taken at the offset to minimize the risk of the development of secondary cutaneous meningioma.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Avecillas-Chasin JM, Saceda-Gutierrez J, Alonso-Lera P, Garcia-Pumarino R, Issa S, Lopez E. Scalp metastases of recurrent meningiomas: Aggressive behavior or surgical seeding?. World Neurosurg. 2015. 84: 121-31
2. Fulkerson DH, Horner TG, Hattab EM. Histologically benign intraventricular meningioma with concurrent pulmonary metastasis: Case report and review of the literature. Clin Neurol Neurosurg. 2008. 110: 416-9
3. Güngör S, Gökdemir G, Tarıkçı N, Sayılgan T, Bek S. Intracranial anaplastic meningioma presenting as a cutaneous lesion: A case report of a cutaneous meningioma. Dermatol Online J. 2012. 18: 6-
4. Hayhurst C, McMurtrie A, Brydon HL. Cutaneous meningioma of the scalp. Acta Neurochir (Wien). 2004. 146: 1383-4
5. Iaconetta G, Santella A, Friscia M, Abbate V, Califano L. Extracranial primary and secondary meningiomas. Int J Oral Maxillofac Surg. 2012. 41: 211-7
6. Miller DC, Ojemann RG, Proppe KH, McGinnis BD, Grillo HC. Benign metastasizing meningioma. Case report. J Neurosurg. 1985. 62: 763-6
7. Pasquier D, Bijmolt S, Veninga T, Rezvoy N, Villa S, Krengli M. Atypical and malignant meningioma: Outcome and prognostic factors in 119 irradiated patients. A multicenter, retrospective study of the rare cancer network. Int J Radiat Oncol Biol Phys. 2008. 71: 1388-93