- Department of Neurosurgery, Hospital e Maternidade Celso Pierro, PUC-Campinas, São Paulo, Brazil
Correspondence Address:
Telmo Augusto Barba Belsuzarri
Department of Neurosurgery, Hospital e Maternidade Celso Pierro, PUC-Campinas, São Paulo, Brazil
DOI:10.4103/2152-7806.178567
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Barba Belsuzarri TA, João Flavio Mattos Araujo, Morassi Melro CA, Fernandes Neves MW, Navarro JN, Brito LG, Carneiro Pontelli LO, Abreu Mattos LG d, Tiago Fernandes Gonçales, Zeviani WM. McCune–Albright syndrome with craniofacial dysplasia: Clinical review and surgical management. Surg Neurol Int 11-Mar-2016;7:
How to cite this URL: Barba Belsuzarri TA, João Flavio Mattos Araujo, Morassi Melro CA, Fernandes Neves MW, Navarro JN, Brito LG, Carneiro Pontelli LO, Abreu Mattos LG d, Tiago Fernandes Gonçales, Zeviani WM. McCune–Albright syndrome with craniofacial dysplasia: Clinical review and surgical management. Surg Neurol Int 11-Mar-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/mccune-albright-syndrome-with-craniofacial-dysplasia-clinical-review-and-surgical-management/
Abstract
Background:Fibrous dysplasia (FD) is a benign fibro-osseous lesion related to an abnormal bone development and replacement by fibrous tissue. FD has three clinical patterns namely monostotic, polyostotic, and the McCune–Albright syndrome (MAS). MAS is a rare genetic disorder (about 3% of all FD's) that comprises a triad of polyostotic FD, café-au-lait skin macules, and precocious puberty. MAS can involve the orbit region and cause stenosis in the optic canal, leading the patient to a progressive visual loss.
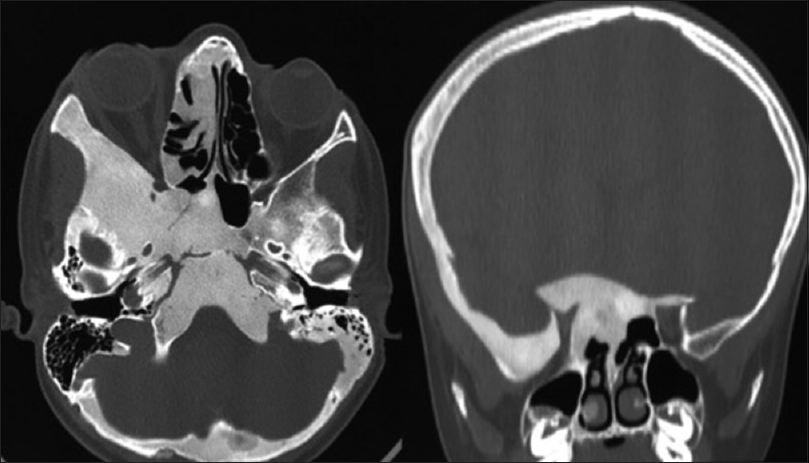
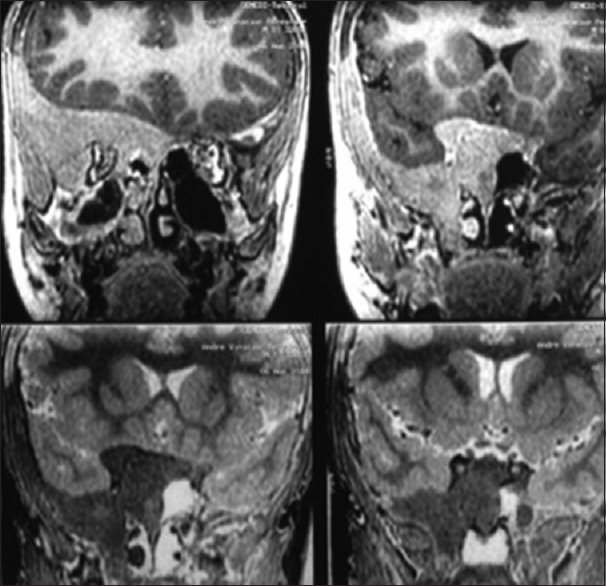
Methods:We reported a case of craniofacial FD in MAS in a 9-year-old male with progressive visual loss, submitted to optic nerve decompression by fronto-orbito-zygomatic approach, with total recovery. A research was made at Bireme, PubMed, Cochrane, LILACS, and MEDLINE with the keywords: FD/craniofacial/McCune–Albright/Optic compression for the clinical review.
Results:A clinical review of the disease was made, the multiple, clinical, and surgical management options were presented, and the case report was reported.
Conclusion:MAS is a rare disease with a progressive polyostotic FD. Whenever it affects the orbit region, the optic canal, and it is associated with a progressive visual loss, the urgent optic nerve decompression is mandatory, either manually or with a rapid drill. It is known that aggressive approach is associated with less recurrence; it is also associated with worsening of the visual loss in optic nerve decompression. In MAS cases, multiple and less aggressive surgeries seem to be more suitable.
Keywords: Craniofacial dysplasia, fibrous dysplasia, McCune–Albright syndrome, orbit fibrous dysplasia, visual loss
INTRODUCTION
Fibrous dysplasia (FD) is a benign intramedullary fibro-osseous lesion related to an abnormal bone development and replacement of bone and marrow bone by fibrous tissue. FD has three clinical patterns namely monostotic, polyostotic, and the McCune–Albright Syndrome (MAS). MAS is a rare sporadic genetic disorder (about 3% of all FD's) that comprises a triad of polyostotic FD, café-au-lait skin macules, precocious puberty, and it is a subtype of the general FD.
CASE REPORT
Male, 9 years old, had a femur bone fracture while running; an orthopedic surgery was performed and referred to the Endocrinology Department [
DISCUSSION
FD is a benign lesion wherein normal bone is replaced by fibrous tissue and immature bone due to a defect on osteoblastic differentiation and maturation.
There are three subtypes of FD: (1) Monostotic, with one bone involvement and the most common subtype. (2) Polyostotic, with multiple bones involvement. (3) MAS which combines polyostotic FD, endocrinopathy, and café-au-lait spots.[
The genetic mutation is located in the chromosome 20q13 in the GNAS locus. The substitution of arginine for cysteine or histidine leads to a hyperactivation of the GSα−cyclic AMP. The overproduction and increased concentration of cAMP in bones over activate the proliferation and abnormal differentiation.[
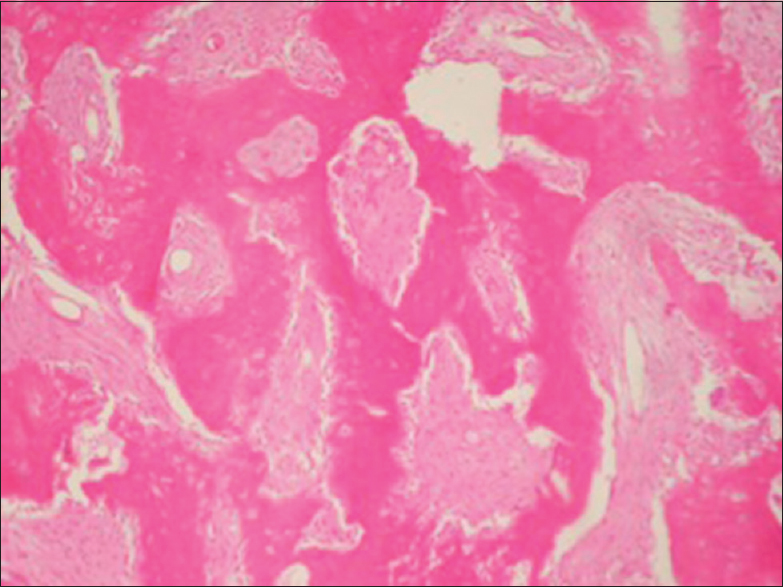
The macroscopic white and brown aspect is typical, and microscopically there is a replace of marrow space by soft fibrous tissue composed of bland spindle cells and abnormal osseous component with irregular trabeculae.
Radiological findings are typical but not pathognomonic and can be divided into three groups:
During investigation, three differential diagnosis can be considered in skull lesions: Osteosarcoma, en plaque meningioma, and osteitis.[
When limited to the craniofacial region, it is considered to be the monostotic form, even if more than one bone is affected, because it is one focus of the disease.[
Malignant transformation in FD is very rare (about 0.4–4%) and more common in the polyostotic disease and the histological types such as osteosarcoma, fibrosarcoma, and chondrosarcoma.[
Recent studies show that the narrowing of the optic canal is not directly correlated to visual loss,[
Visual loss tends to be chronic and acute visual loss is related to aneurysmal bone cysts and mucoceles. Despite the low plasticity of the nerve, urgent decompression of the optic nerve can reverse it.[
The operative management of craniofacial dysplasia in MAS is not well-established because it is a rare syndrome with few case reports in long-term follow-up, with variable outcomes and timing of intervention.[
Surgical technique of decompression can be divided into two subtypes: Conservative decompression and radical surgery. The conservative surgery consists in shaping the dysplastic bone, and it is often repeated over time with the objective of postponing the radical surgery, if needed. The radical approach consists in the radical removal of dysplastic bone and reconstruction with autologous bone graft.[
Postoperative complications occur in 50% of patients and include infections, binocular diplopia, cranial nerve palsy, pain, epistaxis, and ectropion.[
CONCLUSION
MAS is a rare subtype of FD with endocrinopathy. The FD of the orbital region can lead to optic nerve compression and possibly to visual loss. Nowadays, there are no evidences that support the benefits of prophylactic surgery in children with normal visual fields and optic canal narrowing, shown by the CT or MRI, and there is no method to predict which child will stabilize or deteriorate the visual loss. The cystic degenerations can lead to sudden visual loss and is the only possible indication for prophylactic surgery, but the risk of nerve damage should be considered and well-explained. In all other cases of normal visual fields and CT/MRI optic canal narrowing, prophylactic surgery is not indicated, and follow-up should be done. On the other hand, early decompression of symptomatic children is a great standard for a better chance of visual loss reverse.
The surgical technique is not well-established and depends on the case and surgeon expertise, but the conservative approach seems to be more adequate and multiple interventions might be required, especially in McCune–Albright and polyostotic lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abe T, Sato K, Otsuka T, Kawamura N, Shimazu M, Izumiyama H. Optic nerve decompression for orbitofrontal fibrous dysplasia. Skull Base. 2002. 12: 145-52
2. Abe T, Satoh K, Wada A. Optic nerve decompression for orbitofrontal fibrous dysplasia: Recent development of surgical technique and equipment. Skull Base. 2006. 16: 145-55
3. Albright F, Butler A, Hampton A, Smith P. Syndrome characterized by osteitis fibrosa disseminata, areas of pigmentation and endocrine dysfunction, with precocious puberty in females: Report of five cases. N Engl J Med. 1937. 216: 727-46
4. Bousson V, Rey-Jouvin C, Laredo JD, Le Merrer M, Martin-Duverneuil N, Feydy A. Fibrous dysplasia and McCune–Albright syndrome: Imaging for positive and differential diagnoses, prognosis, and follow-up guidelines. Eur J Radiol. 2014. 83: 1828-42
5. Boyce AM, Kelly MH, Brillante BA, Kushner H, Wientroub S, Riminucci M. A randomized, double blind, placebo-controlled trial of alendronate treatment for fibrous dysplasia of bone. J Clin Endocrinol Metab. 2014. 99: 4133-40
6. Chen YR, Breidahl A, Chang CN, Kurimoto M, Endo S, Onizuka K. Extradural optic nerve decompression for fibrous dysplasia with a favourable visual outcome. Neurol Med Chir (Tokyo). 1996. 36: 102-5
7. Chen YR, Noordhoff MS. Treatment of craniomaxillofacial fibrous dysplasia: How early and how extensive?. Plast Reconstr Surg. 1990. 86: 835-42
8. Clifford-Jones RE, Landon DN, McDonald WI. Remyelination during optic nerve compression. J Neurol Sci. 1980. 46: 239-43
9. Cruz AA, Constanzi M, de Castro FA, dos Santos AC. Apical involvement with fibrous dysplasia: Implications for vision. Ophthal Plast Reconstr Surg. 2007. 23: 450-4
10. DiCaprio MR, Enneking WF. Fibrous dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint Surg Am. 2005. 87: 1848-64
11. Dumitrescu CE, Collins MT. McCune-Albright syndrome. Orphanet J Rare Dis. 2008. 3: 12-
12. Hanifi B, Samil KS, Yasar C, Cengiz C, Ercan A, Ramazan D. Craniofacial fibrous dysplasia. Clin Imaging. 2013. 37: 1109-15
13. Harris WH, Dudley HR, Barry RJ. The natural history of fibrous dysplasia, an orthopaedic, pathological and roentgenographic study. Am J Orthop. 1962. 44: 207-33
14. Lee JS, FitzGibbon E, Butman JA, Dufresne CR, Kushner H, Wientroub S. Normal vision despite narrowing of the optic canal in fibrous dysplasia. N Engl J Med. 2002. 347: 1670-6
15. McCarthy EF. Fibro-osseous lesions of the maxillofacial bones. Head Neck Pathol. 2013. 7: 5-10
16. McCune DJ. Osteita fibrosa cystica: The case of nine-year-old girl who also exhibits precocious puberty, multiple pigmentation of the skin and hyperthyroidism. Am J Dis Child. 1936. 52: 743-4
17. McDonald WI. The symptomatology of tumours of the anterior visual pathways. Can J Neurol Sci. 1982. 9: 381-90
18. Pollandt K, Engels C, Kaiser E, Werner M, Delling G. Gsalpha gene mutations in monostotic fibrous dysplasia of bone and fibrous dysplasia-like low-grade central osteosarcoma. Virchows Arch. 2001. 439: 170-5
19. Rahman AM, Madge SN, Billing K, Anderson PJ, Leibovitch I, Selva D. Craniofacial fibrous dysplasia: Clinical characteristics and long-term outcomes. Eye (Lond). 2009. 23: 2175-81
20. Riminucci M, Fisher LW, Shenker A, Spiegel AM, Bianco P, Gehron Robey P. Fibrous dysplasia of bone in the McCune-Albright syndrome: Abnormalities in bone formation. Am J Pathol. 1997. 151: 1587-600
21. Sammut SJ, Kandasamy J, Newman W, Sinha A, Ross J, Blair JC. Relief of severe retro-orbital pain and vision improvement after optic-nerve decompression in polyostotic fibrous dysplasia: Case report and review of the literature. Childs Nerv Syst. 2008. 24: 515-20
22. Siegal G, Dal Cin P, Araujo ES, Fletucher DM, Unni KK, Mertens F.editors. Fibrous dysplasia. WHO Classification of Tumors of Soft Tissue and Bone. Lyon: IARC Press; 2002. p. 341-2
23. Vasilev V, Daly AF, Thiry A, Petrossians P, Fina F, Rostomyan L. McCune-Albright syndrome: A detailed pathological and genetic analysis of disease effects in an adult patient. J Clin Endocrinol Metab. 2014. 99: E2029-38
24. Wu H, Yang L, Li S, Jin X, Xu J, Lu J. Clinical characteristics of craniomaxillofacial fibrous dysplasia. J Craniomaxillofac Surg. 2014. 42: 1450-5
25. Yamamoto T, Ozono K, Kasayama S, Yoh K, Hiroshima K, Takagi M. Increased IL-6-production by cells isolated from the fibrous bone dysplasia tissues in patients with McCune-Albright syndrome. J Clin Invest. 1996. 98: 30-5