- Department of Neurosurgery, University at Buffalo, Buffalo, New York, United States.
DOI:10.25259/SNI_71_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Steven B. Housley, Kunal Vakharia, Muhammad Waqas, Jason M. Davies, Adnan H. Siddiqui. Mechanical venous thrombectomy and prolonged infusion of tissue plasminogen activator for cerebral venous sinus thrombosis: Video case report. 18-Jul-2020;11:193
How to cite this URL: Steven B. Housley, Kunal Vakharia, Muhammad Waqas, Jason M. Davies, Adnan H. Siddiqui. Mechanical venous thrombectomy and prolonged infusion of tissue plasminogen activator for cerebral venous sinus thrombosis: Video case report. 18-Jul-2020;11:193. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10137
Abstract
Background: Cerebral venous sinus thrombosis (CVST) is a rare and often misdiagnosed condition with mortality rates ranging from 6 to 10%. Diagnosis and monitoring are typically achieved through noninvasive imaging, including computed tomography or magnetic resonance venography. The current standard of treatment is systemic anticoagulation. However, in patients who continue to decline neurologically or do not show sufficient response to or have absolute contraindications to systemic anticoagulation, endovascular treatments are an alternative. Endovascular options are poorly studied and specific devices have not been developed, partially due to the rare nature of the disease. Here, we present a case report detailing the treatment of extensive CVST from the vein of Galen to the sigmoid sinus using mechanical thrombectomy and local infusions of unfractionated heparin (UFH) and tissue plasminogen activator.
Case Description: A 53-year-old man presented and was found to have extensive CVST extending from the vein of Galen to the left sigmoid sinus. Systemic UFH was begun; however, his condition continued to decline, and he was taken for endovascular intervention, wherein mechanical thrombectomy was undertaken using combinations of stent retrievers and balloon catheters, which provided acceptable revascularization. Unfortunately, his hospital course was further complicated by a cerebellar hematoma that was surgically evacuated and reocclusion of the sinus for which a microcatheter was placed for infusion of UFH and tissue plasminogen activator.
Conclusion: Complicated CVST may require aggressive endovascular management. Local infusions of heparin and thrombolytic agents as well as mechanical thrombectomy are safe alternative options.
Keywords: Cerebral venous sinus thrombosis, Endovascular therapy, Heparin, Mechanical venous thrombectomy, Tissue plasminogen activator
Annotations
0:30 – Presenting images 0:55 – Dual solitaire (Medtronic) technique 4:00 – Fogarty maneuver 6:22 – Velocity microcatheter (Penumbra) located in the vein of Galen and internal cerebral vein 6:26 – Posttreatment imaging.
INTRODUCTION
Cerebral venous sinus thrombosis (CVST) is a rare condition that accounts for approximately 1% of all strokes.[
CVST is diagnosed with computed tomography (CT) or magnetic resonance imaging (MRI) and best appreciated with venography. Cerebral digital subtraction angiography can be a useful confirmatory modality. Lee et al. published an algorithm that effectively outlines the diagnosis and management of suspected CVST.[
CASE DESCRIPTION
The patient’s family gave informed consent for treatment and video recording. The Institutional Review Board approval was deemed unnecessary.
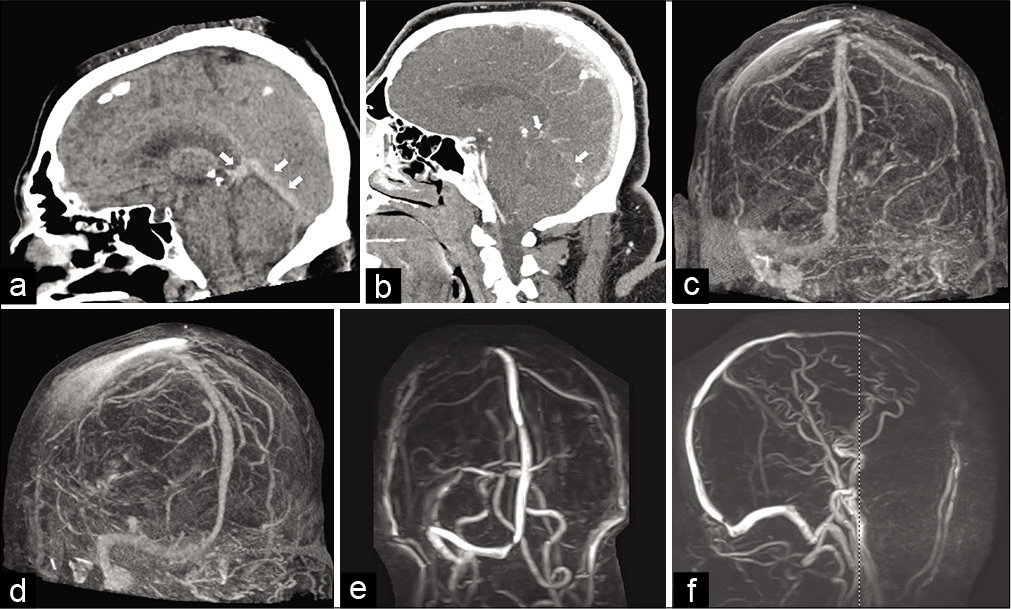
A 53-year-old man placed on aspirin (81 mg, daily) for cardioprotection presented from an outside facility secondary to concerns for a traumatic subarachnoid hemorrhage. He had been experiencing headaches, nausea, and vomiting for 3 days before falling backward from a chair and striking his head against the floor. The following morning, he was found with a subtle dysphasia and intermittent confusion by his family and taken to an outside facility for evaluation. Noncontrast-enhanced head CT scan revealed a hyperdense streak along the left transverse sinus, initially thought to represent subarachnoid hemorrhage. Upon arrival at our facility, the neurosurgery service found that the patient mildly disoriented with a subtle expressive aphasia. Noninvasive imaging, including a CT stroke study, CT angiography (CTA), CT venography (CTV), MRI, and MR venography, revealed near-complete occlusion from the vein of Galen through the left sigmoid sinus [
Figure 1:
(a) Mid sagittal computed tomography (CT) section of the head showing hyperdense thrombus in the straight sinus and vein of Galen (arrows). (b) Contrast-enhanced head CT scan showing opacification of the superior sagittal sinus. There is a lack of opacification of the straight sinus, vein of Galen, and deep veins. (c) CT angiogram (CTA). Occlusion of the left transverse and sigmoid sinuses cannot be seen. (d) Oblique CTA shows occlusion of the straight sinus and vein of Galen. (e) Anteroposterior magnetic resonance venogram shows occlusion of the left transverse and sigmoid sinuses. (f) Lateral magnetic resonance angiogram. The straight sinus and vein of Galen cannot be visualized.
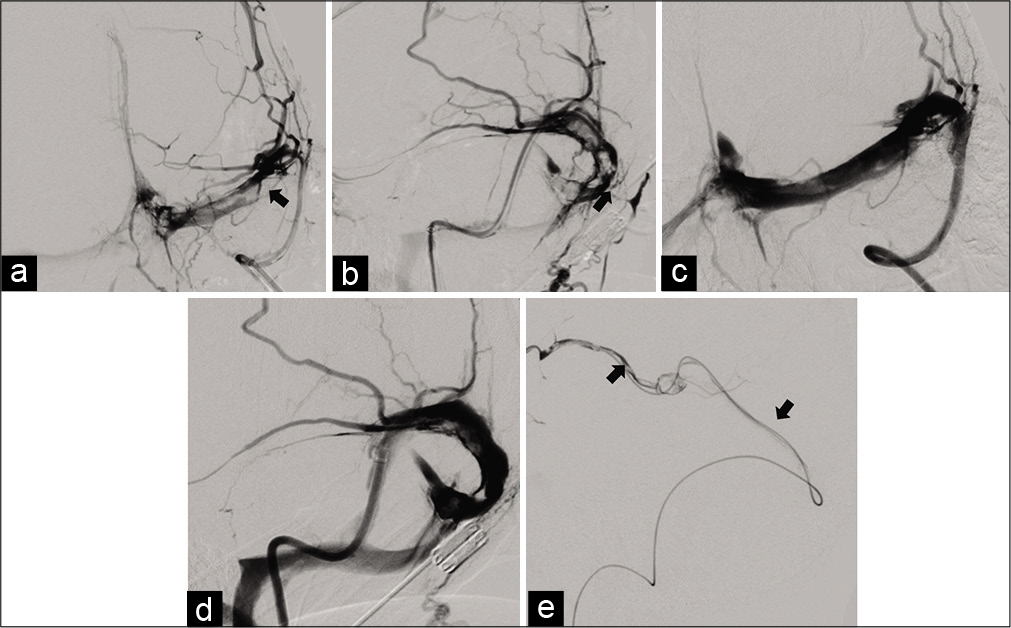
Over the next 48 h, the patient remained stable until his neurological status rapidly declined overnight with rightward gaze deviation, localization to noxious stimuli on the right side, and extensor posturing on the left side. He was then taken emergently to the neuroendovascular suite on hospital day 2 where extensive thrombosis was confirmed [
Figure 2:
(a) Anteroposterior angiogram shows left transverse sinus thrombosis (arrow). (b) Lateral angiogram showing thrombus in the left sigmoid sinus (arrow). (c) Anteroposterior angiogram showing left transverse sinus following thrombectomy. (d) Lateral angiogram shows left sigmoid sinus following thrombectomy. (e) Velocity microcatheter in place (arrows).
The first attempt at crossing the thrombus using a soft tipped, 0.014 inch wire to minimize the risk of venous perforation was unsuccessful as a sufficient channel could not be located. At this point, an 8-French NeuronMax guide catheter (Penumbra, Alameda, CA) was placed into the jugular bulb, and a thrombectomy was performed from the left vein of Galen to the sigmoid sinus. A dual solitaire stent retriever (Medtronic, Dublin, Ireland) technique[
Video 1:
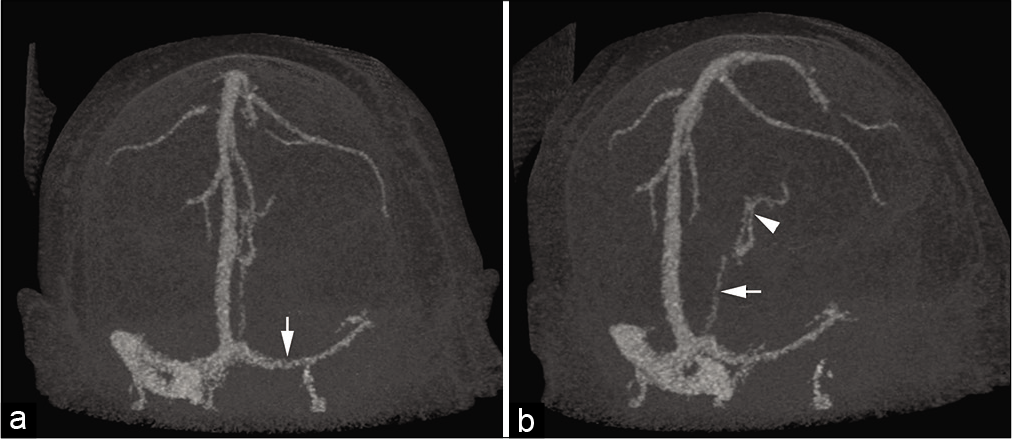
Clot burden was monitored with serial CTA and CTV; and on hospital day 5, tPA was begun, infusing through the microcatheter at a rate of 1 mg/h.[
Following extubation on hospital day 9, the patient was oriented with hypophonic speech and was antigravity in all four extremities. He remained on intravenous UFH through hospital day 11, when this therapy was converted to intravenous argatroban (Pfizer, New York, NY) (0.5–2.5 mcg/kg/min, monitored by aPTT) secondary to heparin-induced thrombocytopenia. On hospital day 15, he was transferred to a medical rehabilitation unit. Systemic heparin therapy was bridged to sodium warfarin on hospital day 18. Intensive rehabilitation resulted in his sole remaining deficit being 4/5 strength in the right hip flexors. He was discharged home with family care and to follow-up with neurologists and neurosurgeons close to his home.
DISCUSSION
Advancements in neuroendovascular technologies have made it possible to mitigate the systemic risks of anticoagulation and provide local effects of anticoagulation and thrombolysis directly to the site of thrombosis. Here, we report on a patient with thrombosis extending from the left vein of Galen into the sigmoid sinus whose condition declined rapidly despite systemic anticoagulation. He was subsequently taken for endovascular thrombectomy and administered local anticoagulation and thrombolysis with good results despite the development of an intraparenchymal hemorrhage that required surgical evacuation and delayed administration of local thrombolytics. Anticoagulation and thrombolysis carry risk, especially in the face of an intraparenchymal hemorrhage, so managing therapeutic options to allow for the shortest window to surgery given the half-lives of thrombolytic agents versus novel anticoagulants play a crucial role in early medical decision-making for these patients.
CONCLUSION
This report illustrates the potential for advancements in the treatment of CVST that is not responsive to traditional therapies or in patients who may have contraindications to systemic anticoagulation. Further investigation into endovascular therapies for CVST is necessary; however, given the low incidence of the disease, case reports help to provide ideas and evidence that aid in providing better and more effective treatment. Here, we show that endovascular thrombectomy followed by local infusion of tPA is safe and feasible. Nonetheless, more research is needed to help elucidate new frontiers in the treatment of a potentially devastating disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Videos available on:
www.surgicalneurologyint.com
Acknowledgments
The authors thank Paul H. Dressel BFA for preparation of the illustrations and Debra J Zimmer for editorial assistance.
References
1. Bousser MG, Ferro JM. Cerebral venous thrombosis: An update. Lancet Neurol. 2007. 6: 162-70
2. Coutinho JM, Stam J. How to treat cerebral venous and sinus thrombosis. J Thromb Haemost. 2010. 8: 877-83
3. Guo XB, Guan S, Fan Y, Song LJ. Local thrombolysis for severe cerebral venous sinus thrombosis. AJNR Am J Neuroradiol. 2012. 33: 1187-90
4. Haghighi AB, Mahmoodi M, Edgell RC, Cruz-Flores S, Ghanaati H, Jamshidi M. Mechanical thrombectomy for cerebral venous sinus thrombosis: A comprehensive literature review. Clin Appl Thromb Hemost. 2014. 20: 507-15
5. Karanam LS, Baddam SR, Pamidimukkala V, Vemuri R, Byrapaneni S, Polavarapu R. Local intrasinus thrombolysis for cerebral venous sinus thrombosis. J Vasc Interv Neurol. 2016. 9: 49-54
6. Klisch J, Sychra V, Strasilla C, Taschner CA, Reinhard M, Urbach H. Double solitaire mechanical thrombectomy in acute stroke: Effective rescue strategy for refractory artery occlusions?. AJNR Am J Neuroradiol. 2015. 36: 552-6
7. Lee SK, Mokin M, Hetts SW, Fifi JT, Bousser MG, Fraser JF. Current endovascular strategies for cerebral venous thrombosis: Report of the SNIS standards and guidelines committee. J Neurointerv Surg. 2018. 10: 803-10
8. Masuhr F, Mehraein S, Einhaupl K. Cerebral venous and sinus thrombosis. J Neurol. 2004. 251: 11-23
9. Qureshi AI, Grigoryan M, Saleem MA, Aytac E, Wallery SS, Rodriguez GJ. Prolonged microcatheter-based local thrombolytic infusion as a salvage treatment after failed endovascular treatment for cerebral venous thrombosis: A multicenter experience. Neurocrit Care. 2018. 29: 54-61
10. Roh D, Carroll J, Melmed K, Elkind MS, Eisenberger A, Francis R. Endovascular treatment of cerebral venous sinus thrombosis and insights into intracranial coagulopathy. J Stroke Cerebrovasc Dis. 2019. 28: e7-9
11. Yamini B, Macdonald RL, Rosenblum J. Treatment of deep cerebral venous thrombosis by local infusion of tissue plasminogen activator. Surg Neurol. 2001. 55: 340-6