- Department of Neurosurgery, University of Rochester, Rochester, New York, United States.
Correspondence Address:
Derek David George, Department of Neurosurgery, University of Rochester, Rochester, New York, United States.
DOI:10.25259/SNI_390_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Derek David George, Clifton Houk, Thomas Allyn Pieters, James E. Towner, Jonathan J. Stone. Meningitis due to intra-abdominal cerebrospinal fluid fistula following gunshot wound successfully treated with antibiotics and blood patch: A case report and literature review. 15-Jul-2022;13:308
How to cite this URL: Derek David George, Clifton Houk, Thomas Allyn Pieters, James E. Towner, Jonathan J. Stone. Meningitis due to intra-abdominal cerebrospinal fluid fistula following gunshot wound successfully treated with antibiotics and blood patch: A case report and literature review. 15-Jul-2022;13:308. Available from: https://surgicalneurologyint.com/surgicalint-articles/11716/
Abstract
Background: Penetrating spinal cord injury (PSCI) represents an average of 5.5% of all SCIs among civilians in the United States. The formation of a cerebrospinal fluid (CSF) fistula following PSCI occurs in approximately 9% of cases. Intra-abdominal CSF fistulae are rarely reported.
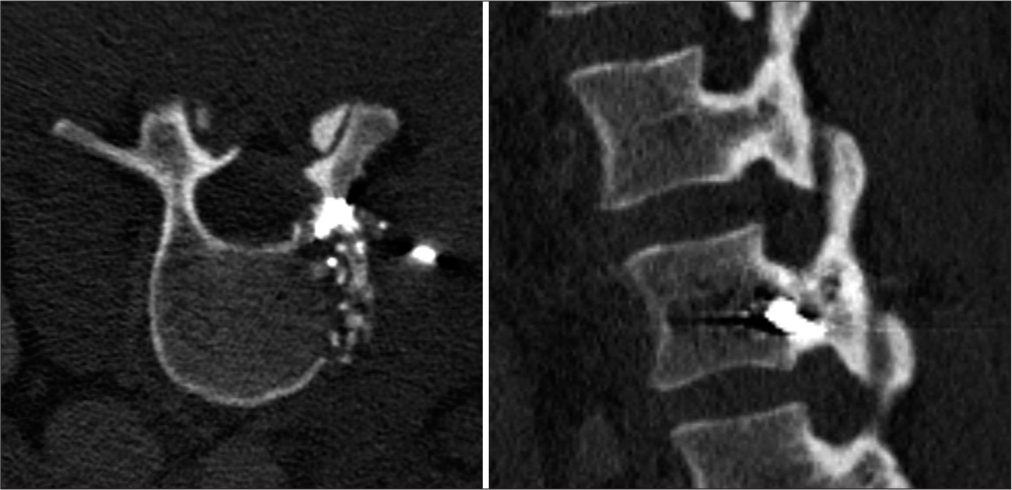
Case Description: We present the case of a 28-year-old Caucasian female who suffered a single gunshot wound to the abdomen with a missile fragment lodged within the left L2 pedicle and transverse process without obvious canal compromise. The patient developed bacterial meningitis 13 days after the initial injury, treated with IV antibiotics. CT myelogram demonstrated intra-abdominal ventral CSF fistula from the left L2–L3 neuroforamen. The patient was successfully treated with fluoroscopy-guided dorsal autologous blood patch graft.
Conclusion: This case highlights a rare complication of PSCI successfully managed with the use of a blood patch graft.
Keywords: Cerebrospinal fluid fistula, Epidural blood patch, Meningitis, Spinal gunshot wound, Trauma
INTRODUCTION
Penetrating spinal cord injury (PSCI) represents an average of 5.5% of all SCIs among civilians in the United States.[
CASE REPORT
We present the case of a 28-year-old Caucasian female who sustained a single abdominal gunshot wound (GSW). She underwent emergent laparotomy where a proximal jejunum perforation was discovered and repaired. Postoperative computed tomography (CT) imaging showed bullet fragments in and adjacent to the left L2 pedicle, without obvious spinal canal compromise [
The patient then returned to the emergency department at our center postinjury day 13 with headache, photophobia, and nausea. On examination, she was found to be febrile to 38.6 Celsius, lethargic with meningismus, but fully oriented with an otherwise nonfocal neurologic examination. Contrasted CT of the abdomen was unremarkable. CSF studies were obtained through lumbar puncture which revealed cloudy CSF with elevated nucleated cells (7925 cells/μL) and red blood cells (168 cells/μL), low glucose (<5 mg/dL), and elevated CSF protein (318 mg/dL) suggestive of bacterial meningitis. Gram stain revealed >25 polymorphonuclear cells per low-power field, but revealed no organisms, and aerobic and anaerobic culture did not identify causal organisms. Her intra-abdominal drain contents were sampled and negative for β2-transferrin. A pyelogram revealed a persistent ureteral leak, for which the patient received a ureteral stent. Empiric IV antibiotic therapy with vancomycin, cefepime, and metronidazole was initiated for the treatment of meningitis and sustained for 14 days. A lumbar CT myelogram was obtained, revealing an area of contrast leakage ventrally into the retroperitoneum in the area of the left L2–L3 neuroforamen without myelographic block [
DISCUSSION
Within the United States, PSCI represents 5.5% of all SCIs among civilians.[
Due to the abdomen and pelvis being common regions of firearm injuries, the incidence of concomitant abdominal or pelvic organ injury is high, with studies estimating abdominal viscus injury occurring in 57–69% of cases.[
CSF fistula is an uncommon complication of firearm-associated PSCI, occurring in approximately 9% of cases.[
At present, there are no guidelines for the management of CSF fistulae from traumatic missile injuries to the spine.[
In the cases that spontaneous resolution of CSF fistula does not result, CSF diversion may be attempted. For example, fistulae isolated to the thoracolumbar spine may benefit from placement of a lumbar drain.[
CONCLUSION
Intra-abdominal CSF fistula secondary to projectile missile injury represents an uncommon manifestation of penetrating vertebral column injuries. Such fistulae are associated with higher rates of meningitis or other nervous system infections. Various treatment modalities have been described; however, there are no guidelines for the treatment of these fistulae. In our case, the patient presented with a single projectile missile wound to the abdomen with an involvement of the left L2 pedicle and L2–L3 neuroforamen. Our patient presented in a slightly delayed fashion with meningitis, and intraperitoneal CSF fistula was confirmed on CT myelogram. She was treated with empiric antibiotic therapy and dorsal epidural blood patch grafting, with resolution of meningitis and without development of intracranial hypotension symptoms. Our case demonstrates the successful treatment of this rare clinical entity with a minimally invasive approach.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alakaya M, Arslankoylu AE, Danaci EV, Ozalp H, Ozgur A, Ispir C. A rare cause of pleural effusion; cerebrospinal fluid leakage. J Pediatr Neurosci. 2017. 12: 117-8
2. Amrhein TJ, Befera NT, Gray L, Kranz PG. CT fluoroscopy-guided blood patching of ventral CSF leaks by direct needle placement in the ventral epidural space using a transforaminal approach. AJNR Am J Neuroradiol. 2016. 37: 1951-6
3. Avila MJ, Martirosyan NL, Hurlbert RJ, Dumont TM. Penetrating spinal cord injury in civilians: Analysis of a national database. World Neurosurg. 2021. 146: e985-92
4. Bourghli A, Abouhashem S, Abo Wali R, Obeid I, Boissiere L, Vital JM. Management of a posterior gunshot injury with a floating pedicle and cerebrospinal fluid leak. Eur Spine J. 2018. 27: 1681-7
5. Couture D, Branch CL. Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus. 2003. 15: E6
6. Crutcher CL 2nd, Wilson JM, Morrow KD, Shields JA, Lasseigne LM, Culicchia F. Management of cerebrospinal fluid leak from cervical gunshot wounds with external ventricular drainage: A small case series. J Surg Case Rep. 2020. 2020: rjaa484
7. de Barros Filho TE, Cristante AF, Marcon RM, Ono A, Bilhar R. Gunshot injuries in the spine. Spinal Cord. 2014. 52: 504-10
8. Duffy PJ, Crosby ET. The epidural blood patch. Resolving the controversies. Can J Anaesth. 1999. 46: 878-86
9. Hadley MN, Walters BC. Introduction to the guidelines for the management of acute cervical spine and spinal cord injuries. Neurosurgery. 2013. 72: 5-16
10. Kahraman S, Gonul E, Kayali H, Sirin S, Duz B, Beduk A. Retrospective analysis of spinal missile injuries. Neurosurg Rev. 2004. 27: 42-5
11. Kırık A, Yaşar S. The efficacy of continuous lumbar drainage in post-traumatic cerebrospinal fluid fistulas. Ulus Travma Acil Cerrahi Derg. 2020. 26: 784-8
12. Kumar A, Wood GW 2nd, Whittle AP. Low-velocity gunshot injuries of the spine with abdominal viscus trauma. J Orthop Trauma. 1998. 12: 514-7
13. Lemole GMHenn JSZabramski JMSonntag VK. The Management of Cranial and Spinal CSF Leaks. Available from: https://www.barrowneuro.org/for-physicians-researchers/education/grand-rounds-publications-media/barrow-quarterly/volume-17-no-4-2001/the-management-ofcranial-and-spinal-csf-leaks [Last accessed on 2022 Apr 25].
14. Lin SS, Vaccaro AR, Reisch S, Devine M, Cotler JM. Low-velocity gunshot wounds to the spine with an associated transperitoneal injury. J Spinal Disord. 1995. 8: 136-44
15. Loder RT, Mishra A, Atoa B, Young A. Spinal injury associated with firearm use. Cureus. 2021. 13: e13918
16. Morrow KD, Podet AG, Spinelli CP, Lasseigne LM, Crutcher CL, Wilson JD. A case series of penetrating spinal trauma: Comparisons to blunt trauma, surgical indications, and outcomes. Neurosurg Focus. 2019. 46: E4
17. Ohry A, Zeilig G. Traumatic spinal cord injury followed by cerebrospinal fluid complications. Spinal Cord. 1990. 28: 208-11
18. Pasupuleti LV, Sifri ZC, Mohr AM. Is extended antibiotic prophylaxis necessary after penetrating trauma to the thoracolumbar spine with concomitant intraperitoneal injuries?. Surg Infect (Larchmt). 2014. 15: 8-13
19. Quigley KJ, Place HM. The role of debridement and antibiotics in gunshot wounds to the spine. J Trauma. 2006. 60: 814-9
20. Roffi RP, Waters RL, Adkins RH. Gunshot wounds to the spine associated with a perforated viscus. Spine (Phila Pa 1976). 1989. 14: 808-11
21. Romanick PC, Smith TK, Kopaniky DR, Oldfield D. Infection about the spine associated with low-velocity-missile injury to the abdomen. J Bone Joint Surg Am. 1985. 67: 1195-201
22. Schwed AC, Plurad DS, Bricker S, Neville A, Bongard F, Putnam B. Abdominal hollow viscus injuries are associated with spine and neurologic infections after penetrating spinal cord injuries. Am Surg. 2014. 80: 966-9
23. Sencakova D, Mokri B, McClelland RL. The efficacy of epidural blood patch in spontaneous CSF leaks. Neurology. 2001. 57: 1921-3
24. Shannon N, Kendall B, Thomas D, Baker H. Subarachnoidpleural fistula case report and review of literature. J Neurol Neurosurg Psychiatry. 1982. 45: 457-60
25. Spanos A, Harrell FE, Durack DT. Differential diagnosis of acute meningitis. An analysis of the predictive value of initial observations. JAMA. 1989. 262: 2700-7
26. Styliaras JC, Dalyai R, Amgad H, Sharan A, Harrop J. Cerebrospinal fluid leaks from penetrating injuries: Diagnosis and treatment. Argo Spine News J. 2012. 24: 183-7
27. Wilson TH. Penetrating trauma of colon, cava, and cord. J Trauma. 1976. 16: 411-3
28. Zilkha A, Reiss J, Shulman K, Schechter MM. Traumatic subarachnoid-mediastinal fistula; case report. J Neurosurg. 1970. 32: 473-5