- Department of Neurosurgery, University of Kansas School of Medicine, Kansas City, United States
- Department of Neurosurgery, University of Kansas Medical Center, Kansas City, United States.
Correspondence Address:
Cody Heskett, Department of Neurosurgery, University of Kansas School of Medicine, Kansas City, United States.
DOI:10.25259/SNI_1137_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Cody Heskett1, Jean-Luc Kabangu2, Adip Bhargav2, Roukoz Chamoun2, Ifije Ohiorhenuan2. Metastatic esthesioneuroblastoma with widespread recurrence to the central nervous system. 03-Mar-2023;14:77
How to cite this URL: Cody Heskett1, Jean-Luc Kabangu2, Adip Bhargav2, Roukoz Chamoun2, Ifije Ohiorhenuan2. Metastatic esthesioneuroblastoma with widespread recurrence to the central nervous system. 03-Mar-2023;14:77. Available from: https://surgicalneurologyint.com/surgicalint-articles/12181/
Abstract
Background: Esthesioneuroblastomas (ENBs) are rare malignancies of the upper digestive tract, often demonstrating local metastasis to the intracranial space through the cribriform plate. These tumors show high rates of recurrence locally following treatment. Here, we report a patient with advanced recurrent ENB 2 years following initial treatment, affecting both the spine and intracranial space without evidence of local recurrence or contiguous extension from the initial tumor site.
Case Description: A 32-year-old male presents with a 2 month history of neurological symptoms 2 years following treatment of Kadish C/AJCC stage IVB (T4a, N3, M0) ENB. No evidence of locoregional recurrent disease was observed prior with intermittent imaging. Imaging revealed a large ventral epidural tumor invading multiple levels of the thoracic spine as well as a ring enhancing lesion in the right parietal lobe. The patient was treated surgically with debridement, decompression, and posterior stabilization of the thoracic spine followed by radiotherapy to the spinal and parietal lesions. Chemotherapy was also initiated. Despite treatment, the patient passed away 6 months after surgery.
Conclusion: We report a case of delayed recurrent ENB with widespread metastases to the central nervous system without evidence of local disease or contiguous extension from initial tumor site. This represents a highly aggressive form of this tumor as recurrences are primarily locoregional. In follow-up of ENB treatment, clinicians must be cognizant of these tumors demonstrated ability to spread to distal regions. All new onset neurological symptoms should be investigated fully even if no local recurrence is observed.
Keywords: Esthesioneuroblastoma, Neuro-oncology, Olfactory neuroblastoma, Spinal metastasis
INTRODUCTION
Esthesioneuroblastoma (ENB) or olfactory neuroblastoma is a rare malignant tumor arising from olfactory neuroepithelium, accounting for approximately 3% of all sinonasal malignancies and 0.3% of upper digestive tract malignancies.[
ENB commonly metastasizes to the cervical lymph nodes; however, researchers have also described metastasis to the pelvis, breast, lung, abdominal viscera, long bones, and spine.[
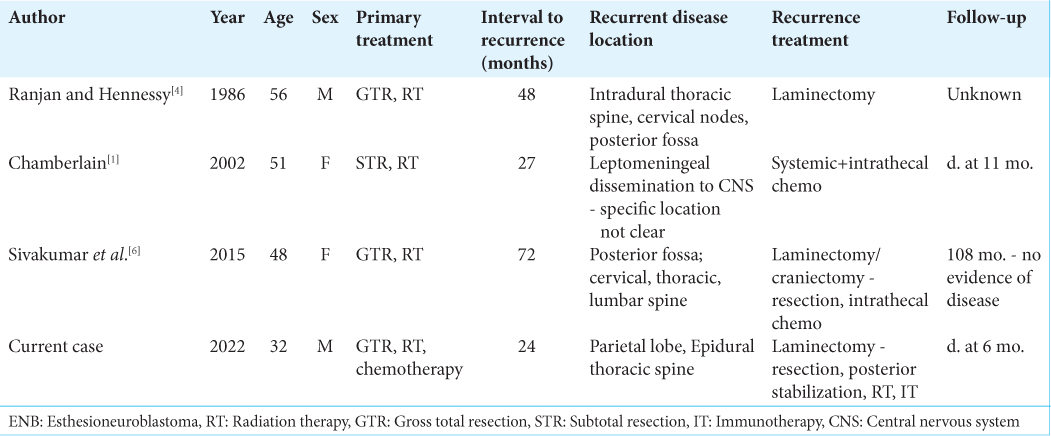
Central nervous system (CNS) recurrence is common, but widespread dissemination involving both the intracranial space and spine without evidence of local recurrence is exceedingly rare, seen <5 times in literature.[
Here, we present a case of highly aggressive recurrent ENB presenting 2 years following initial treatment, with widespread CNS involvement including a large mass of the thoracic spine and noncontiguous intracranial parietal lesions without local recurrence.
CASE REPORT
History
A 32-year-old male presented 2 years after treatment for a Kadish C/AJCC stage IVB (T4a, N3, M0) ENB involving the left nasal cavity, anterior cranial fossa, and retropharyngeal lymph nodes. Initial treatment involved intracranial and intranasal tumor resection, radical left neck dissection, cisplatin therapy, and radiation. Radiation therapy was directed both at the primary tumor bed in the superior sinonasal area as well as the bilateral neck area following the radical neck dissection. He presented to the emergency department (ED) following a 2-month duration of left upper back pain radiating to the scapula. Multiple physicians had attributed this pain to a nerve injury sustained during the initial surgical treatment of his ENB, as it had spread to the cervical lymphatics requiring left neck dissection. In the week before his ED visit, the patient began to develop bilateral lower extremity weakness and loss of balance with the left side worse than the right. Decreased sensation was reported in the left leg including the left lower abdomen to the level of the umbilicus.
Physical examination
Examination revealed diffuse 4/5 strength in all left lower extremity muscle groups and 5/5 strength in all other tested muscle groups. Sensation was decreased in the lower extremities and trunk to approximately the level of T4 with the left side worse than the right. Reflexes were 2+ throughout and plantar response demonstrated down-going toes bilaterally. His gait was unsteady. All cranial nerves were intact. Pulmonary exam revealed no respiratory distress, lungs clear to auscultation bilaterally, and normal breath sounds. He had a regular heart rate and rhythm without evidence of murmur or gallop. No visible masses were observed on the neck or trunk. The remainder of the physical examination was unremarkable.
Investigations
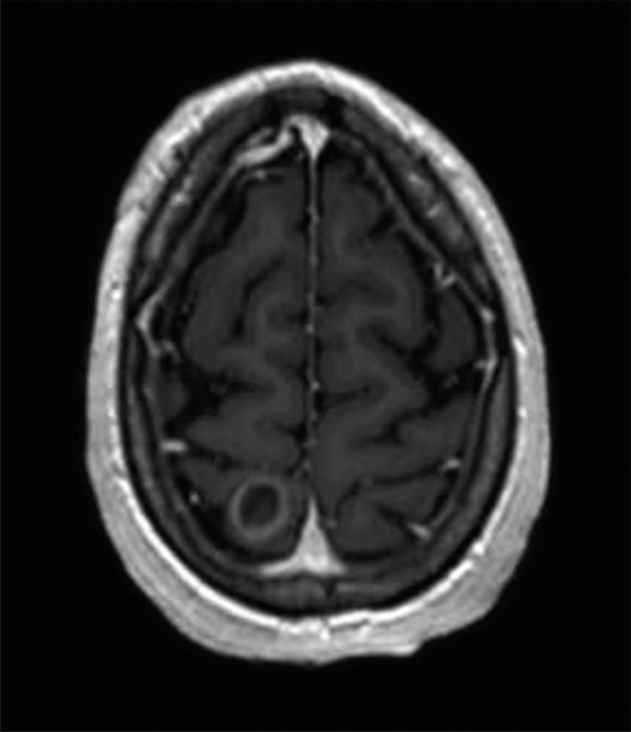
Magnetic resonance imaging (MRI) of the head revealed a ring enhancing lesion in the right medial parietal lobe consistent with noncontiguous intracranial ENB recurrence [
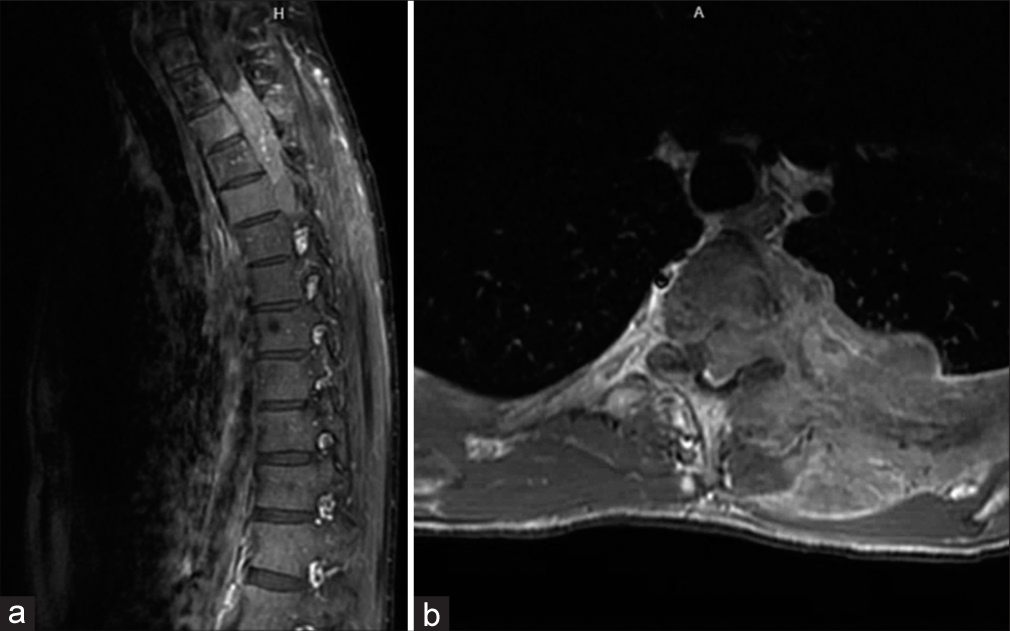
Figure 2:
(a) Contrast-enhanced sagittal T1-weighted magnetic resonance imaging (MRI) image of the thoracic spine demonstrating a large mass extending from multiple neural foramina at the level of approximately T3-T5. Multiple areas of abnormal signal intensity are seen in the thoracic vertebral bodies likely representing significant marrow replacement by infiltrating tumor. (b) Contrast enhanced axial T1-weighted MRI image at the level of thoracic spine demonstrating a ventral epidural mass causing severe canal stenosis and right lateral displacement of the spinal cord. The mass extends through the neural foramen to the dorsal paraspinous soft tissues and the left pleural area.
Surgery
Due to the patient’s declining neurological function from the spinal mass and risk for instability from T3 to T5 vertebral body marrow replacement and adjuvant radiation therapy, a decompression and fusion procedure was recommended. The patient was taken to surgery and placed prone on a Wilson frame. Post-positioning neuromonitoring revealed decline in left-side motor evoked potentials. Incision was made over the upper thoracic area and subcutaneous dissection was taken to the level of the spinous processes. Subperiosteal dissection was performed over the lamina and spinous processes of T1-T7. Neuronavigation was used to place screws bilaterally at the T1-T7 levels. Laminectomy and wide foraminotomies were performed at levels T3-T5. The epidural tumor was identified and debulked. The T3 and T4 nerve roots were identified and ligated to allow for decompression of the tumor in the canal and epidural space. Following decompression, motor potentials had improved on the left and remained stable on the right. Frozen sections taken intraoperatively indicated a diagnosis of ENB, later confirmed with immunohistochemistry.
Post-operative course
The patient did well in the early postoperative period. He was discharged to an acute inpatient rehabilitation facility on post-operative day 7, where he had improvement in his lower extremity weakness and was sent home with ongoing outpatient physical and occupational therapy after 14 days. The new intracranial metastasis and the residual spine/ pleural mass were treated with radiation postoperatively. He also participated in a clinical trial investigating the use of immunotherapy including anti PD-1 and anti CTLA-4 agents. Unfortunately, the patient passed away as a result of his disease burden 6 months after surgery.
DISCUSSION
A salient feature of our case is the presence of a non-contiguous intracranial lesion occurring concurrently to a spinal lesion, likely representing a rare example of widespread leptomeningeal dissemination, occurring outside of the primary area previously treated by radiation and resection. Only one prior case of widespread CNS recurrence involving both the spine and brain reports long-term treatment success.[
Early workup of unusual symptoms following ENB treatment should be pursued to limit advanced presentation of recurrent disease. While local surveillance is often performed, clinicians must be cognizant that ENB has demonstrated the potential for widespread CNS dissemination without evidence of recurrent local disease. Our patient had been receiving routine surveillance imaging of the head and neck with both computed tomography (CT) and MRI in the 2 years between primary treatment and recurrence. This also included a CT of the chest approximately 1 year before recurrence that showed no abnormalities, begging the question if more frequent and wider surveillance imaging should be performed in patients following treatment of ENB. Inability to distinguish new onset neurological symptoms from tumor burden rather than iatrogenic injury from prior surgery contributed to delayed diagnosis at an advanced stage of disease. Unfortunately, our patient’s spine tumor was not amenable to complete resection due to ventral extension and intricate involvement of exiting nerve roots. Decompression and stabilization were performed to slow further neurologic decline, while chemoradiation was used in attempts to control tumor burden.
No such treatment paradigm exists specifically for recurrent ENB. Tumors are treated in similar methods to primary occurrence. The role of surgical resection should always be assessed in recurrent disease as an adjunct to chemo and radiation therapy, which have been reported to improve survivability. Radiotherapy at a minimum should be provided with additional chemotherapy also conferring potential survival benefits.[
CONCLUSION
Here, we report a rare case of ENB initially treated using a combination of resection, chemotherapy, and radiation with recurrent widespread metastasis to the CNS without local recurrence. Clinicians evaluating patients with previously diagnosed ENB should entertain suspicion for metastatic spread to the distal CNS and intracranial space. We advocate for a more thorough evaluation of the CNS due to the potential for widespread CNS dissemination. For that rare form of disease progression, we advocate for multimodal therapy.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chamberlain MC. Treatment of intracranial metastatic esthesioneuroblastoma. Cancer. 2002. 95: 243-8
2. Fiani B, Quadri SA, Cathel A, Farooqui M, Ramachandran A, Siddiqi I. Esthesioneuroblastoma: A comprehensive review of diagnosis, management, and current treatment options. World Neurosurg. 2019. 126: 194-211
3. Packer RJ, Sutton LN, Goldwein JW, Perilongo G, Bunin G, Ryan J. Improved survival with the use of adjuvant chemotherapy in the treatment of medulloblastoma. J Neurosurg. 1991. 74: 433-40
4. Ranjan D, Hennessy RG. Esthesioneuroblastoma: Cerebral and spinal metastases without direct cranial invasion. J Neurooncol. 1986. 4: 71-4
5. Shaari CM, Catalano PJ, Sen C, Post K. Central nervous system metastases from esthesioneuroblastoma. Otolaryngol Head Neck Surg. 1996. 114: 808-12
6. Sivakumar W, Oh N, Cutler A, Colman H, Couldwell WT. Cranial and spinal leptomeningeal dissemination in esthesioneuroblastoma: Two reports of distant central nervous system metastasis and rationale for treatment. Surg Neurol Int. 2015. 6: S628-32
7. Zanation AM, Ferlito A, Rinaldo A, Gore MR, Lund VJ, McKinney KA. When, how and why to treat the neck in patients with esthesioneuroblastoma: A review. Eur Arch Otorhinolaryngol. 2010. 267: 1667-71