- Department of Neurosurgery, University of Tsukuba, Tsukuba, Ibaraki, Japan.
DOI:10.25259/SNI_94_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Satoshi Miyamoto, Masahide Matsuda, Eiichi Ishikawa, Akira Matsumura. Microvascular decompression for abducens nerve palsy due to neurovascular compression from both the vertebral artery and anterior inferior cerebellar artery: A case report. 15-Aug-2020;11:242
How to cite this URL: Satoshi Miyamoto, Masahide Matsuda, Eiichi Ishikawa, Akira Matsumura. Microvascular decompression for abducens nerve palsy due to neurovascular compression from both the vertebral artery and anterior inferior cerebellar artery: A case report. 15-Aug-2020;11:242. Available from: https://surgicalneurologyint.com/surgicalint-articles/10215/
Abstract
Background: Neurovascular compression is an extremely rare etiology of isolated abducens nerve palsy. We describe a successfully treated case of isolated abducens nerve palsy due to sandwich-type compression by the vertebral artery (VA) and anterior inferior cerebellar artery (AICA).
Case Description: A 30-year-old man presented with a 6-month history of horizontal diplopia without other symptoms. Magnetic resonance imaging (MRI) demonstrated pinching of the left abducens nerve between the elongated left VA and left AICA. MRI showed no abnormal findings in the brainstem, cavernous sinus, or orbit. Surgery was performed using a standard lateral suboccipital approach. The abducens nerve was found to be severely compressed from both sides by the VA and AICA, with marked indentation. First, the VA was transposed and fixed to the dura mater of the petrous bone using a Teflon sling with the dripping of fibrin glue. Next, because of limited mobilization due to penetration of the AICA into the nerve, the AICA transfixing the nerve was attached to the pons with Teflon felt and fibrin glue to move the AICA away from the main trunk of the abducens nerve. The abducens nerve palsy gradually improved and eventually resolved by 4 months after the operation.
Conclusion: When an elongated vertebrobasilar artery is identified as the offending vessel on high-resolution MRI, microvascular decompression can be carefully considered as a treatment option for patients with isolated abducens nerve palsy.
Keywords: Abducens nerve palsy, Anterior inferior cerebellar artery, Microvascular decompression, Neurovascular compression, Vertebral artery
INTRODUCTION
Isolated abducens nerve palsy is the most common ocular motor cranial neuropathy.[
Here, we present a case of isolated abducens nerve palsy due to sandwich-type neurovascular compression by the vertebral artery (VA) and AICA, which was successfully treated with microvascular decompression (MVD). In this report, we discuss the surgical indication and strategy for abducens nerve palsy due to neurovascular compression.
CASE REPORT
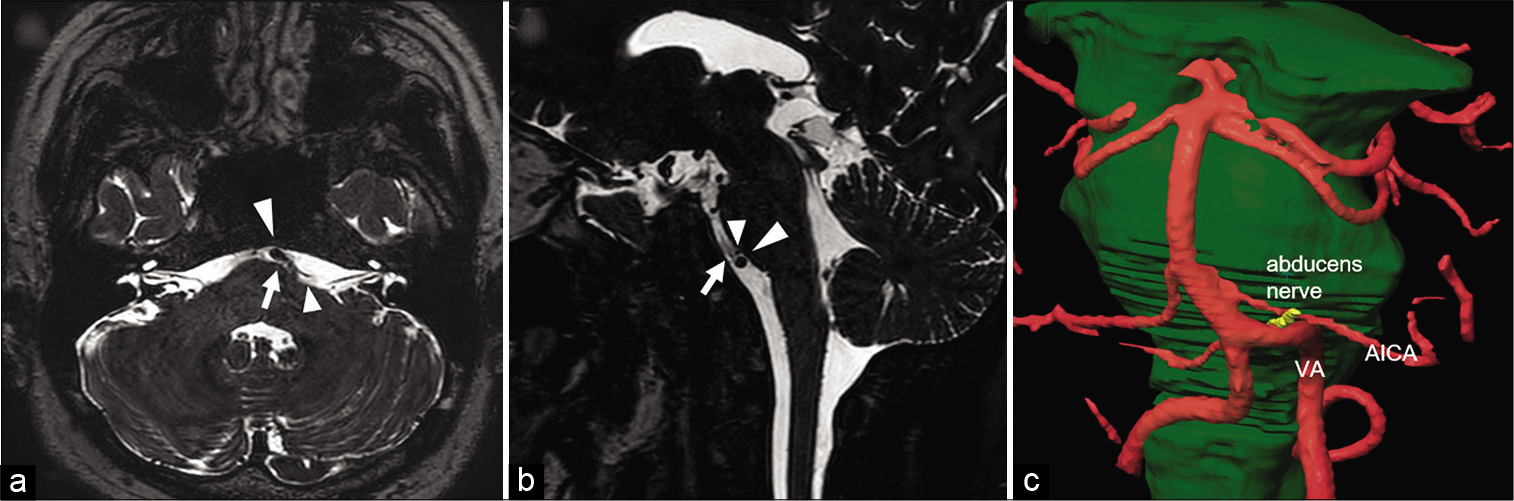
A 30-year-old man presented with a 6-month history of horizontal diplopia without other symptoms. He was diagnosed with left-sided abducens nerve palsy by an ophthalmologist and referred to our hospital for further investigation. Other than bronchial asthma, his medical history was not significant. Neurological examination revealed left abducens nerve palsy without signs of impairment of any other cerebral nerves. His visual acuity was 1.2 on the right side and 1.0 on the left side. Laboratory test results, including HbA1c, C-reactive protein, and erythrocyte sedimentation rate, were normal. MRI with high-resolution T2-weighted imaging driven equilibrium radiofrequency reset pulse (T2WI-DRIVE) sequence showed pinching of the left abducens nerve between the elongated left VA and left AICA [
Figure 1:
Preoperative magnetic resonance imaging. Preoperative axial T2-weighted imaging driven equilibrium radiofrequency reset pulse (T2WI-DRIVE) (a) and sagittal T2WI-DRIVE (b) demonstrate sandwich-type neurovascular compression of the abducens nerve by the vertebral artery (VA) and anterior inferior cerebellar artery (AICA). A three-dimensional (3D) MR fusion image (c) shows pinching of the abducens nerve between the elongated VA and AICA. Arrows indicate the abducens nerve. Large arrowheads indicate the VA. Small arrowheads indicate the AICA.
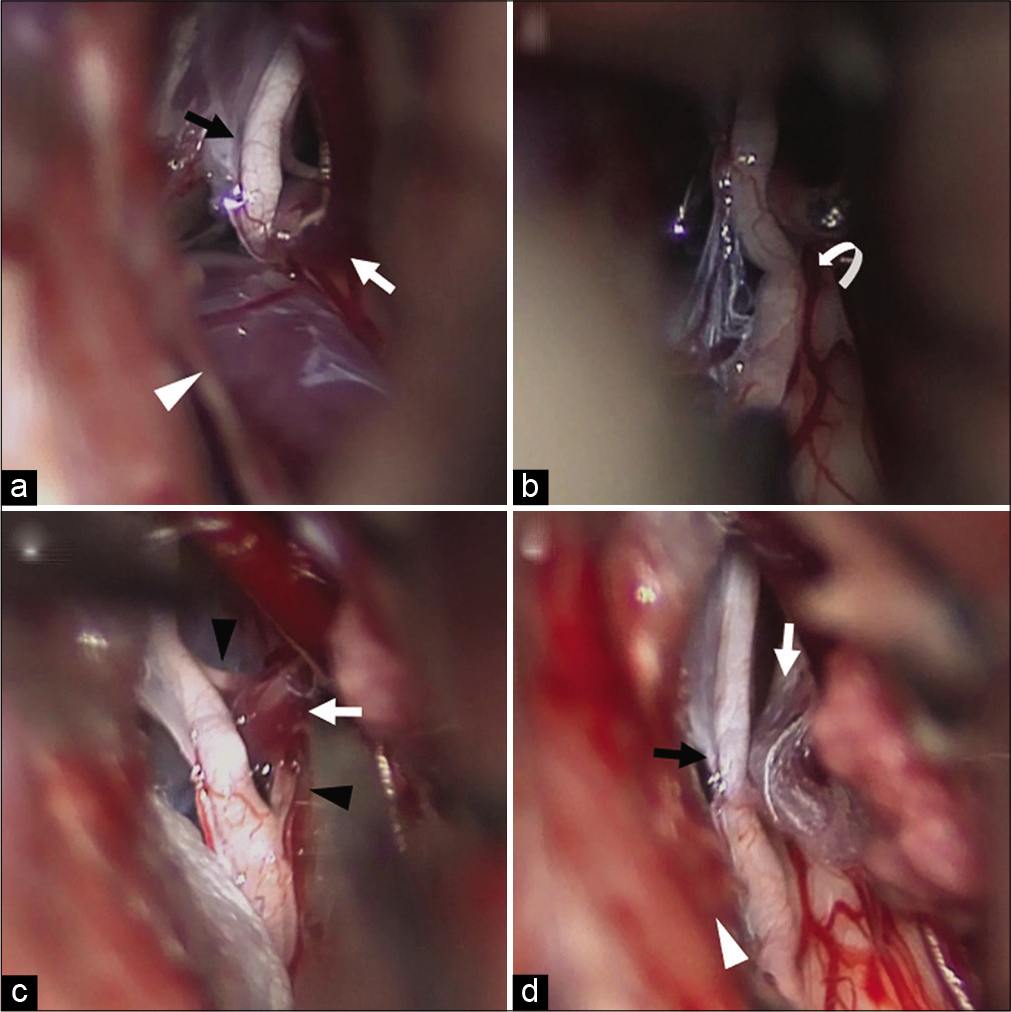
Because his symptoms did not improve spontaneously in 6 months, we decided to perform MVD for this patient. Surgery was performed using a standard lateral suboccipital approach. After the dural incision, the cerebellomedullary cistern was opened to release cerebrospinal fluid and allow sufficient cerebellar relaxation. The arachnoid membrane just above the lower cranial nerves was dissected. The lower cranial nerves were further dissected free from the choroid plexus to enable a clear view of the abducens nerve. The abducens nerve was found to be severely compressed from both sides by the VA and AICA [
Figure 2:
Intraoperative photograph. (a) An intraoperative photograph reveals that the abducens nerve was pinched between the VA and AICA. (b) An intraoperative photograph shows a severe indentation of the abducens nerve. (c) An intraoperative photograph demonstrates penetration of the abducens nerve by the AICA. (d) An intraoperative photograph shows that the abducens nerve was released from neurovascular compression by the VA and AICA. Black arrows indicate the main trunk of the abducens nerve. White arrowheads indicate the VA. White arrows indicate the AICA. The white curved arrow indicates the indentation of the abducens nerve. Black arrowheads indicate the small nerve fiber of the abducens nerve.
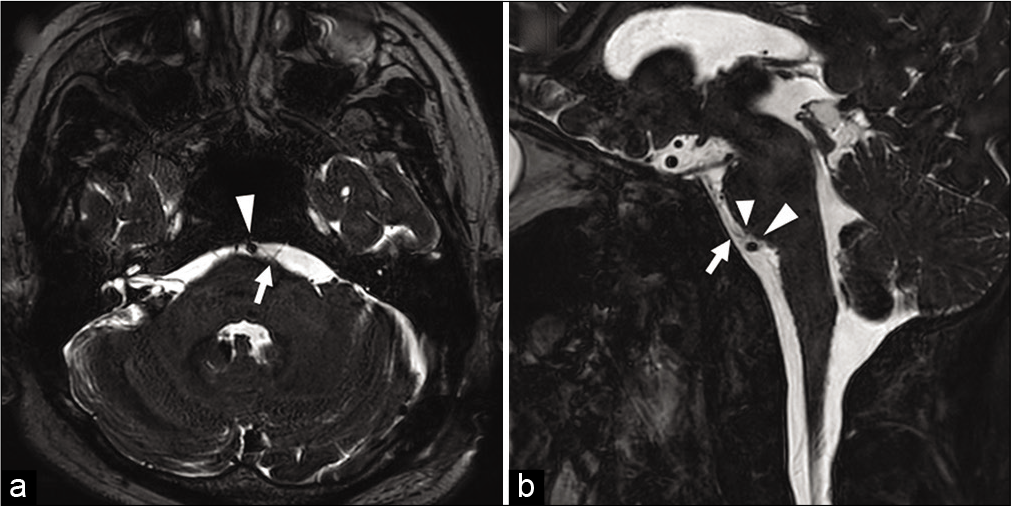
Postoperatively, the patient presented transient dysphagia, presumably due to intraoperative retraction of the lower cranial nerves, which recovered after a few weeks. MRI demonstrated the disappearance of the neurovascular conflict of the abducens nerve with the VA and AICA [
Figure 3:
Postoperative magnetic resonance imaging. Postoperative axial T2-weighted imaging driven equilibrium radiofrequency reset pulse (T2WI-DRIVE) (a) and sagittal T2WI-DRIVE (b) show disappearance of neurovascular compression of the abducens nerve by the VA and AICA. Arrows indicate the abducens nerve. Large arrowheads indicate the VA. Small arrowhead indicates the AICA.
DISCUSSION
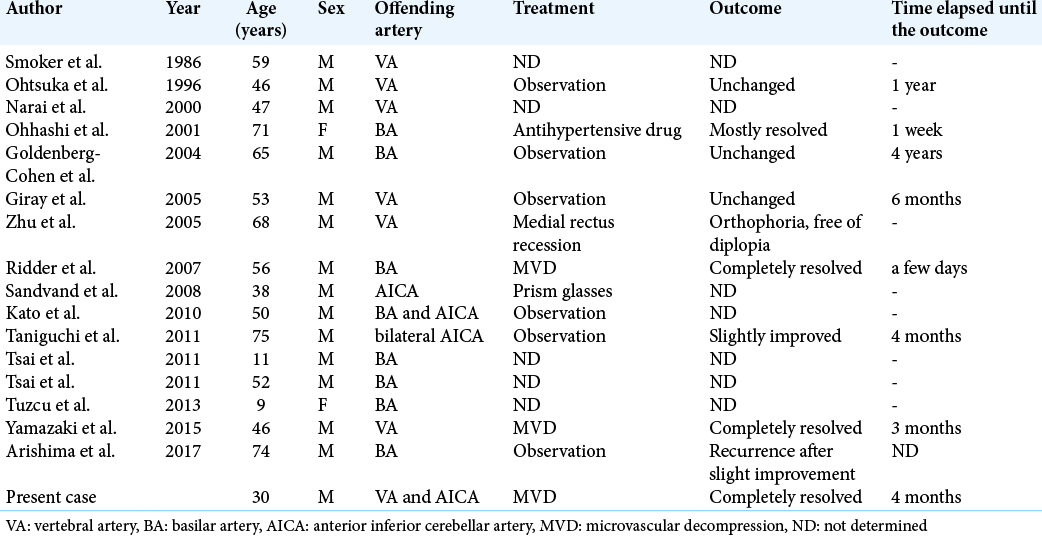
Offending arteries and outcome of treatments
To the best of our knowledge, 15 reports (16 cases) of isolated abducens nerve palsy due to neurovascular compression have been described in the literature [
Surgical indication
Due to the small number of reported cases of isolated abducens nerve palsy, particularly in surgically treated cases, determining the surgical indication is difficult. For isolated abducens nerve palsy of unknown origin, the spontaneous recovery rate was about 74% by 6 months.[
Neurovascular compression observed on MRI does not always cause symptoms. A previous study using detailed MRI revealed that the abducens nerve contacts the AICA in 76.6% of asymptomatic people.[
Operation
The abducens nerve emerges near the midline at the pontomedullary junction. The nerve then ascends in a rostral and lateral direction toward the clivus through the most caudomedial part of the cerebellopontine cistern[
In the present case, the AICA penetrated the abducens nerve, which made mobilization of the AICA away from the abducens nerve difficult. The previous anatomical studies have revealed that the AICA or its main branches pierce the abducens nerve in 11.4–25.0% of cases.[
CONCLUSION
Neurovascular compression, although rare, should be considered a possible underlying cause of isolated abducens nerve palsy. When an elongated vertebrobasilar artery is identified as the offending vessel on high-resolution MRI in a patient whose isolated abducens nerve palsy does not spontaneously recover, MVD can be carefully considered as one of the treatment options.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arishima H, Kikuta KI. Magnetic resonance imaging findings of isolated abducent nerve palsy induced by vascular compression of vertebrobasilar dolichoectasia. J Neurosci Rural Pract. 2017. 8: 124-7
2. De Ridder D, Menovsky T. Neurovascular compression of the abducent nerve causing abducent palsy treated by microvascular decompression. Case report. J Neurosurg. 2007. 107: 1231-4
3. Elder C, Hainline C, Galetta SL, Balcer LJ, Rucker JC. Isolated abducens nerve palsy: Update on evaluation and diagnosis. Curr Neurol Neurosci Rep. 2016. 16: 69
4. Esmer AF, Sen T, Bilecenoglu B, Tuccar E, Uz A, Karahan ST. Neurovascular relationship between abducens nerve and anterior inferior cerebellar artery. Folia Morphol (Warsz). 2010. 69: 201-3
5. Feng BH, Zheng XS, Wang XH, Ying TT, Yang M, Tang YD. Management of vessels passing through the facial nerve in the treatment of hemifacial spasm. Acta Neurochir (Wien). 2015. 157: 1935-40
6. Giray S, Pelit A, Kizilkilic O, Karatas M. Isolated abducens nerve palsy caused by contralateral vertebral artery dolichoectasia. Neurol India. 2005. 53: 246-7
7. Goldenberg-Cohen N, Miller NR. Noninvasive neuroimaging of basilar artery dolichoectasia in a patient with an isolated abducens nerve paresis. Am J Ophthalmol. 2004. 137: 365-7
8. Kato H, Nakajima M, Ohnaka Y, Ishihara K, Kawamura M. Recurrent abducens nerve palsy associated with neurovascular compression. J Neurol Sci. 2010. 295: 135-6
9. King AJ, Stacey E, Stephenson G, Trimble RB. Spontaneous recovery rates for unilateral sixth nerve palsies. Eye (Lond). 1995. 9: 476-8
10. Marinkovic SV, Gibo H, Stimec B. The neurovascular relationships and the blood supply of the abducent nerve: Surgical anatomy of its cisternal segment. Neurosurgery. 1994. 34: 1017-26
11. Na BS, Cho JW, Park K, Kwon S, Kim YS, Kim JS. Severe hemifacial spasm is a predictor of severe indentation and facial palsy after microdecompression surgery. J Clin Neurol. 2018. 14: 303-9
12. Narai H, Manabe Y, Deguchi K, Iwatsuki K, Sakai K, Abe K. Isolated abducens nerve palsy caused by vascular compression. Neurology. 2000. 55: 453-4
13. Ohhashi G, Irie K, Tani S, Ogawa T, Abe T, Hata Y. Isolated abducens nerve palsy caused by the compression of the basilar artery: A case report. No To Shinkei. 2001. 53: 69-72
14. Ohtsuka K, Sone A, Igarashi Y, Akiba H, Sakata M. Vascular compressive abducens nerve palsy disclosed by magnetic resonance imaging. Am J Ophthalmol. 1996. 122: 416-9
15. Sandvand KA, Ringstad G, Kerty E. Periodic abducens nerve palsy in adults caused by neurovascular compression. J Neurol Neurosurg Psychiatry. 2008. 79: 100-2
16. Smoker WR, Corbett JJ, Gentry LR, Keyes WD, Price MJ, McKusker S. High-resolution computed tomography of the basilar artery: 2. Vertebrobasilar dolichoectasia: Clinical-pathologic correlation and review. AJNR Am J Neuroradiol. 1986. 7: 61-72
17. Taniguchi A, Ii Y, Kobayashi H, Maeda M, Tomimoto H. Bilateral abducens nerve palsy by compression from bilateral anterior inferior cerebellar artery. J Neurol. 2011. 258: 2271-3
18. Tashiro H, Kondo A, Aoyama I, Nin K, Shimotake K, Nishioka T. Trigeminal neuralgia caused by compression from arteries transfixing the nerve. Report of three cases. J Neurosurg. 1991. 75: 783-6
19. Tsai TH, Demer JL. Nonaneurysmal cranial nerve compression as cause of neuropathic strabismus: Evidence from high-resolution magnetic resonance imaging. Am J Ophthalmol. 2011. 152: 1067-73.e2
20. Tuzcu EA, Bayarogullari H, Coskun M, Yilmaz C, Ilhan N, Daglioglu MC. Bilateral abducens paralysis secondary to compression of abducens nerve roots by vertebrobasilar dolichoectasia. Neuroophthalmology. 2013. 37: 254-6
21. Umansky F, Valarezo A, Elidan J. The microsurgical anatomy of the abducens nerve in its intracranial course. Laryngoscope. 1992. 102: 1285-92
22. Yamazaki T, Yamamoto T, Hatayama T, Zaboronok A, Ishikawa E, Akutsu H. Abducent nerve palsy treated by microvascular decompression: A case report and review of the literature. Acta Neurochir (Wien). 2015. 157: 1801-5
23. Yousry I, Camelio S, Wiesmann M, Schmid UD, Moriggl B, Bruckmann H. Detailed magnetic resonance imaging anatomy of the cisternal segment of the abducent nerve: Dorello’s canal and neurovascular relationships and landmarks. J Neurosurg. 1999. 91: 276-83
24. Zhu Y, Thulborn K, Curnyn K, Goodwin J. Sixth cranial nerve palsy caused by compression from a dolichoectatic vertebral artery. J Neuroophthalmol. 2005. 25: 134-5