- Department of Neurosurgery, Barrow Neurological Institute, St. Joseph's Hospital and Medical Center, Phoenix, Arizona, USA
Correspondence Address:
Felipe C. Albuquerque
Department of Neurosurgery, Barrow Neurological Institute, St. Joseph's Hospital and Medical Center, Phoenix, Arizona, USA
DOI:10.4103/2152-7806.179575
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Almefty RO, S. Kalani MY, Ducruet AF, Crowley RW, McDougall CG, Albuquerque FC. Middle meningeal arteriovenous fistulas: A rare and potentially high-risk dural arteriovenous fistula. Surg Neurol Int 01-Apr-2016;7:
How to cite this URL: Almefty RO, S. Kalani MY, Ducruet AF, Crowley RW, McDougall CG, Albuquerque FC. Middle meningeal arteriovenous fistulas: A rare and potentially high-risk dural arteriovenous fistula. Surg Neurol Int 01-Apr-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/middle-meningeal-arteriovenous-fistulas-a-rare-and-potentially-high%e2%80%91risk-dural-arteriovenous-fistula/
Abstract
Background:Middle meningeal arteriovenous fistulas (MMAVFs) are rare lesions with a poorly established natural history. We report our experience with patients with MMAVFs who presented with intracranial hemorrhage.
Methods:We reviewed our prospectively maintained endovascular database for patients with MMAVFs, who were treated by embolization during a 15-year period. Hospital and outpatient medical records and imaging studies were reviewed.
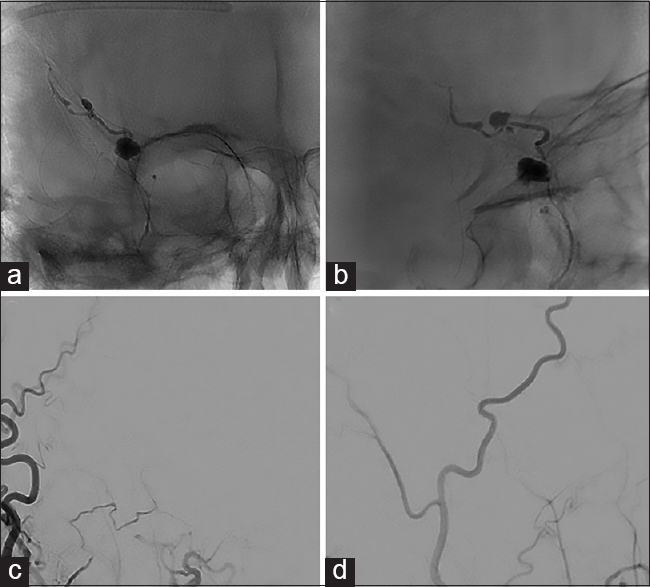
Results:Nine patients with MMAVFs, who presented with intracranial hemorrhage, underwent embolization (mean age 60.3 years, range 21–76; four male and five female). Four patients presented after trauma and five after spontaneous hemorrhage. All nine patients were angiographically cured after embolization of the fistula with liquid embolic agents (n = 8) or coils (n = 1). There were no procedure-related complications.
Conclusion:MMAVFs represent a rarely reported class of vascular lesions. They are typically associated with trauma, but also develop spontaneously, and may be associated with intracranial hemorrhage, which warrants classification of these lesions as high risk. Endovascular treatment is safe and effective and should be considered for these patients, particularly for those who have lesions with intracranial venous drainage.
Keywords: Arteriovenous, embolization, fistula, hemorrhage, meningeal, vascular
INTRODUCTION
Middle meningeal arteriovenous fistulas (MMAVFs) occur between the middle meningeal artery and neighboring veins or dural venous sinuses and are rare lesions that have largely been the subject of single case reports.[
METHODS
We searched our prospectively maintained endovascular treatment database for patients with MMAVFs, who were treated by embolization. Only those cases in which a fistula existed between the middle meningeal artery and neighboring veins or dural sinuses were included. Cases in which the middle meningeal artery contributed to dural arteriovenous fistulas of the major venous sinuses were not included. Hospital and outpatient medical records and imaging studies were reviewed for patients who met the inclusion criteria.
RESULTS
Nine patients (five female and four male) with MMAVFs [
Case Illustration
A middle-aged patient was admitted to our service after being involved in a serious accident. On presentation to the trauma bay, the patient's Glasgow Coma Scale score was 9. Given this poor score and respiratory distress, the patient was intubated. Imaging revealed traumatic SAH [
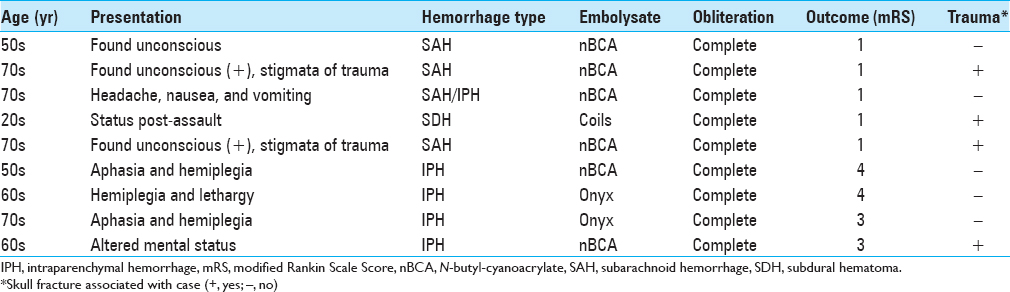
Figure 1
Initial diagnostic tests after trauma. (a) Axial computed tomographic scan shows thick, diffuse subarachnoid hemorrhage. (b) Computed tomographic angiogram shows left internal carotid artery aneurysm. Anteroposterior (c) and lateral (d) angiograms show a middle meningeal artery-to-vein fistula. Used with permission from Barrow Neurological Institute, Phoenix, AZ, USA
As a part of routine work-up for cases of traumatic brain injury, computed tomography angiography of the head was ordered. Review of this study suggested the presence of a small aneurysm arising from the left internal carotid artery [
Formal cerebral angiography, including selective injections of the bilateral internal and external carotid arteries and the vertebrobasilar system, was performed. The patient was noted to indeed have a small 2-mm aneurysm of the left internal carotid artery arising from the cavernous segment (not shown). The patient was also noted to have a traumatic arteriovenous fistula of the middle meningeal artery [Figure
Ultimately, the patient's neurological status remained poor with the patient spontaneously moving the right upper extremity and flexing the bilateral lower extremities (confounded by the presence of bilateral orthopedic injuries), and was flaccid in his left upper extremity.
Sixteen days after the initial trauma, the patient was noted to be less responsive, and a new computed tomography study revealed a new IPH [
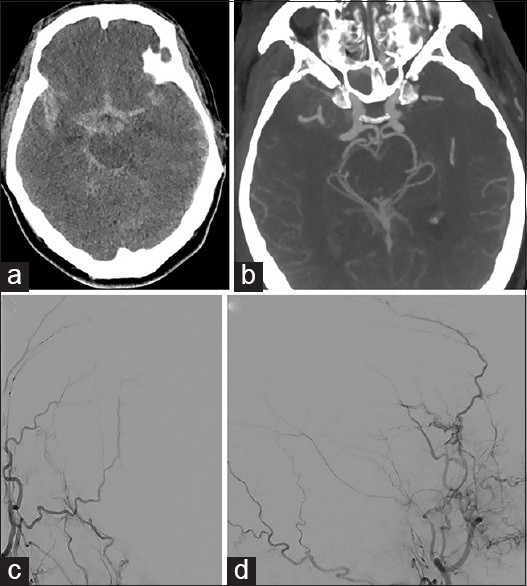
Figure 2
Imaging performed 16 days posttrauma after the patient experienced neurological decline. (a) Axial computed tomographic scan shows a new right temporal intraparenchymal hemorrhage. (b) Computed tomographic angiogram shows vasospasm in the right middle cerebral artery distribution and an abnormal dilation in a vessel adjacent to the hematoma. (c and d) Selective middle meningeal artery injections show newly developed pseudoaneurysms associated with the previously detected fistula. Used with permission from Barrow Neurological Institute, Phoenix, AZ, USA
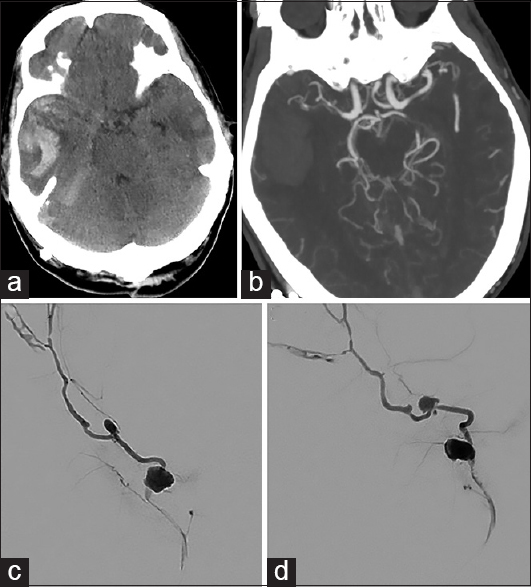
Figure 3
Imaging performed after embolization of the middle meningeal arteriovenous fistula with N-butyl-cyanoacrylate glue. (a and b) Unsubtracted views show glue cast in the fistula. Anteroposterior (c) and lateral (d) angiograms after embolization show no residual fistula. Used with permission from Barrow Neurological Institute, Phoenix, AZ, USA
DISCUSSION
Nine patients with MMAVFs and intracranial hemorrhage underwent endovascular fistula embolization. The cohort includes patients with fistulas of traumatic etiology and patients who presented with spontaneous intracranial hemorrhage and were found to have an MMAVF. Five of the 9 patients (63%) had no history of trauma – 1 patient presented with SAH, 3 had an IPH, and 1 presented with both SAH and IPH. It is well known that traumatic MMAVFs occur although the true incidence is unclear given that many patients may go undiagnosed. MMAVFs in patients presenting with spontaneous hemorrhage have only rarely been reported. Although the etiology of traumatic and spontaneous MMAVFs is different, we grouped them together because of their shared anatomical features, hemorrhagic potential, and treatment.
In the largest reported series to date, Freckmann et al. reviewed the angiograms of 446 head trauma patients and found eight cases of MMAVFs, for a rate of 1.8%.[
Although the majority of MMAVFs occur after traumatic injury, some develop spontaneously. More importantly, as we observed in our patients without a prior history of trauma, these lesions pose a risk of intracranial hemorrhage, regardless of their etiology. As a result, the presence of an MMAVF may explain some cases of nonaneurysmal SAH and thus a complete work-up for SAH requires 6-vessel angiography.
Although MMAVFs have been rarely reported in the literature, the hemorrhagic potential of these lesions was clearly demonstrated by Sakata et al.[
Our experience certainly indicates that these lesions warrant consideration as high risk, particularly those with cortical venous drainage. We do not have a cohort of untreated MMAVF patients whom we have followed, which would give us a better sense of the natural history of these lesions. However, our series does demonstrate the hemorrhagic potential of MMAVFs as well as the ability to safely access and obliterate these lesions through an endovascular approach. On the basis of these findings, we believe that treatment of MMAVFs should be considered.[
In our series, all fistulas were completely embolized without complications. Liquid embolic agents were primarily used given the small size and distal location of these fistulas. Although we have recently favored Onyx for transarterial embolization of dural arteriovenous fistulas, in cases where distal navigation of the microcatheter is limited by vessel tortuosity, we have found that a dilute mixture of nBCA may be more likely to effectively penetrate the fistula to achieve a definitive cure.
CONCLUSION
MMAVFs are rare and likely underreported vascular lesions. They are typically associated with trauma, but also develop spontaneously, and may lead to intracranial hemorrhage. They should be regarded as high-risk lesions and treatment should be considered, particularly for those lesions with intracranial venous drainage. Early treatment results for endovascular embolization are encouraging.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank the Neuroscience Publications Office at Barrow Neurological Institute for support.
References
1. Chandrashekar HS, Nagarajan K, Srikanth SG, Jayakumar PN, Vasudev MK, Pandey P. Middle meningeal arteriovenous fistula and its spontaneous closure. A case report and review of the literature. Interv Neuroradiol. 2007. 13: 173-8
2. Fincher EF. Arteriovenous fistula between the middle meningeal artery and the greater petrosal sinus; case report. Ann Surg. 1951. 133: 886-8
3. Freckmann N, Sartor K, Herrmann HD. Traumatic arteriovenous fistulae of the middle meningeal artery and neighbouring veins or dural sinuses. Acta Neurochir (Wien). 1981. 55: 273-81
4. Ishii R, Ueki K, Ito J. Traumatic fistula between a lacerated middle meningeal artery and a diploic vein; case report. J Neurosurg. 1976. 44: 241-4
5. Liu Ah, Lv X, Li Y, Lv M, Wu Z. Traumatic middle meningeal artery and fistula formation with the cavernous sinus: Case report. Surg Neurol. 2008. 70: 660-3
6. Markham JW. Arteriovenous fistula of the middle meningeal artery and the greater petrosal sinus. J Neurosurg. 1961. 18: 847-8
7. Nakamura K, Tsugane R, Ito H, Obata H, Narita H. Traumatic arterio-venous fistula of the middle meningeal vessels. J Neurosurg. 1966. 25: 424-9
8. Pakarinen S. Arteriovenous fistula between the middle meningeal artery and the sphenoparietal sinus. A case report. J Neurosurg. 1965. 23: 438-9
9. Roski RA, Owen M, White RJ, Takaoka Y, Bellon EM. Middle meningeal artery trauma. Surg Neurol. 1982. 17: 200-3
10. Sakata H, Nishimura S, Mino M, Hori E, Fujita T, Midorikawa H. Serial angiography of dynamic changes of traumatic middle meningeal arteriovenous fistula: Case report. Neurol Med Chir (Tokyo). 2009. 49: 462-4
11. Sicat LC, Brinker RA, Abad RM, Rovit RL. Traumatic pseudoaneurysm and arteriovenous fistula involving the middle meningeal artery. Surg Neurol. 1975. 3: 97-103
12. Smith JE, Epps J, Press HC, Adair LB. Traumatic arteriovenous fistula between the middle meningeal artery and the sphenoparietal sinus: A case report and review of the world literature. J Natl Med Assoc. 1981. 73: 274-8
13. Tsutsumi M, Kazekawa K, Tanaka A, Ueno Y, Nomoto Y, Nii K. Traumatic middle meningeal artery pseudoaneurysm and subsequent fistula formation with the cavernous sinus: Case report. Surg Neurol. 2002. 58: 325-8
14. Unterhofer C, Chemelli A, Waldenberger P, Bauer R, Ortler M. Traumatic fistula between the middle meningeal artery and the sphenoparietal sinus. Acta Neurochir (Wien). 2009. 151: 1301-4
15. Watanabe T, Matsumaru Y, Sonobe M, Asahi T, Onitsuka K, Sugita K. Multiple dural arteriovenous fistulae involving the cavernous and sphenoparietal sinuses. Neuroradiology. 2000. 42: 771-4
16. Wilson CB, Cronic F. Traumatic arteriovenous fistulas involving middle meningeal vessels. JAMA. 1964. 188: 953-7