- Department of Neurosurgery, Saiseikai Noe Hospital, Osaka, Japan
- Department of Neurosurgery, Hyogo Medical University, Nishinomiya, Japan.
Correspondence Address:
Takuto Kuwajima, Department of Neurosurgery, Saiseikai Noe Hospital, Osaka, Japan.
DOI:10.25259/SNI_265_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takuto Kuwajima1,2, Mikiya Beppu1,2, Shinichi Yoshimura2. Minimally invasive craniotomy for putaminal hemorrhage using a tubular retractor: A technical note. 31-May-2024;15:183
How to cite this URL: Takuto Kuwajima1,2, Mikiya Beppu1,2, Shinichi Yoshimura2. Minimally invasive craniotomy for putaminal hemorrhage using a tubular retractor: A technical note. 31-May-2024;15:183. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12916
Abstract
Background: Minimally invasive endoscopic and stereotactic surgery have been established as surgical treatments for putaminal hemorrhage. However, facilities that do not have equipment for endoscopic or stereotactic surgery will likely have to perform conventional craniotomy. Using a tubular retractor, we were able to perform minimally invasive surgery, such as endoscopic surgery.
Methods: A craniotomy was performed for left putaminal hemorrhage after cerebral infarction treatment. A 3–4 cm craniotomy centered at Kocher’s point was performed under general anesthesia. A 2 cm incision was made in the cortex, and a tubular retractor was inserted under a microscope. The hematoma was reached at a position 4–5 cm from the cortex.
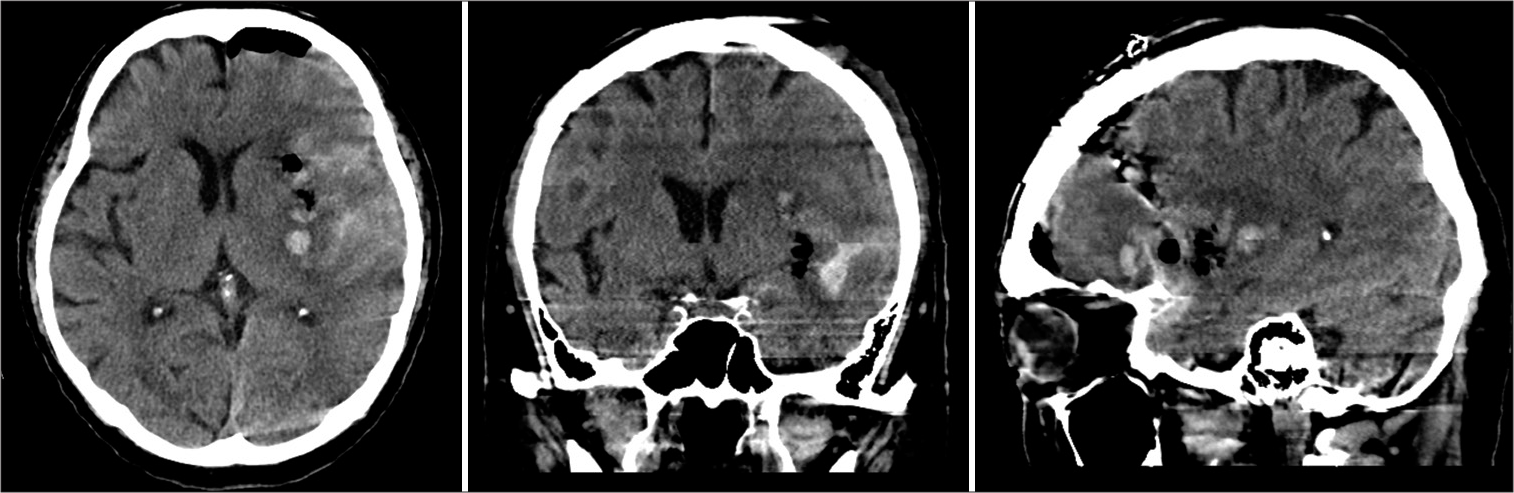
Results: Thanks to the tubular retractor, it was relatively easy to observe the hematoma, and it was possible to remove it and confirm hemostasis without difficulty. Brain injury caused by the retractor insertion cavity was small, and no hemostasis was required. The surgery was completed by dura mater closure, bone flap fixation, and wound closure as per the standard. Most of the putaminal hemorrhage could be removed, and there was no rebleeding after the operation. The patient is still undergoing rehabilitation because of aphasia and muscle weakness. Manual Muscle Testing was at three points in the upper limb, and four points in the lower limb remained.
Conclusion: For putaminal hemorrhage, microscopic craniotomy was performed using a tubular retractor and an approach such as endoscopic surgery. Craniotomy, hematoma removal, and hemostasis operations are also considered to be minimally invasive surgeries.
Keywords: Craniotomy surgery, Minimally invasive surgery, Putaminal hemorrhage, Removal of hematoma, Tubular retractor, Craniotomy
INTRODUCTION
Minimally invasive endoscopic surgery and stereotactic surgery have been established as surgical treatments for putaminal hemorrhage.[
ILLUSTRATIVE CASE
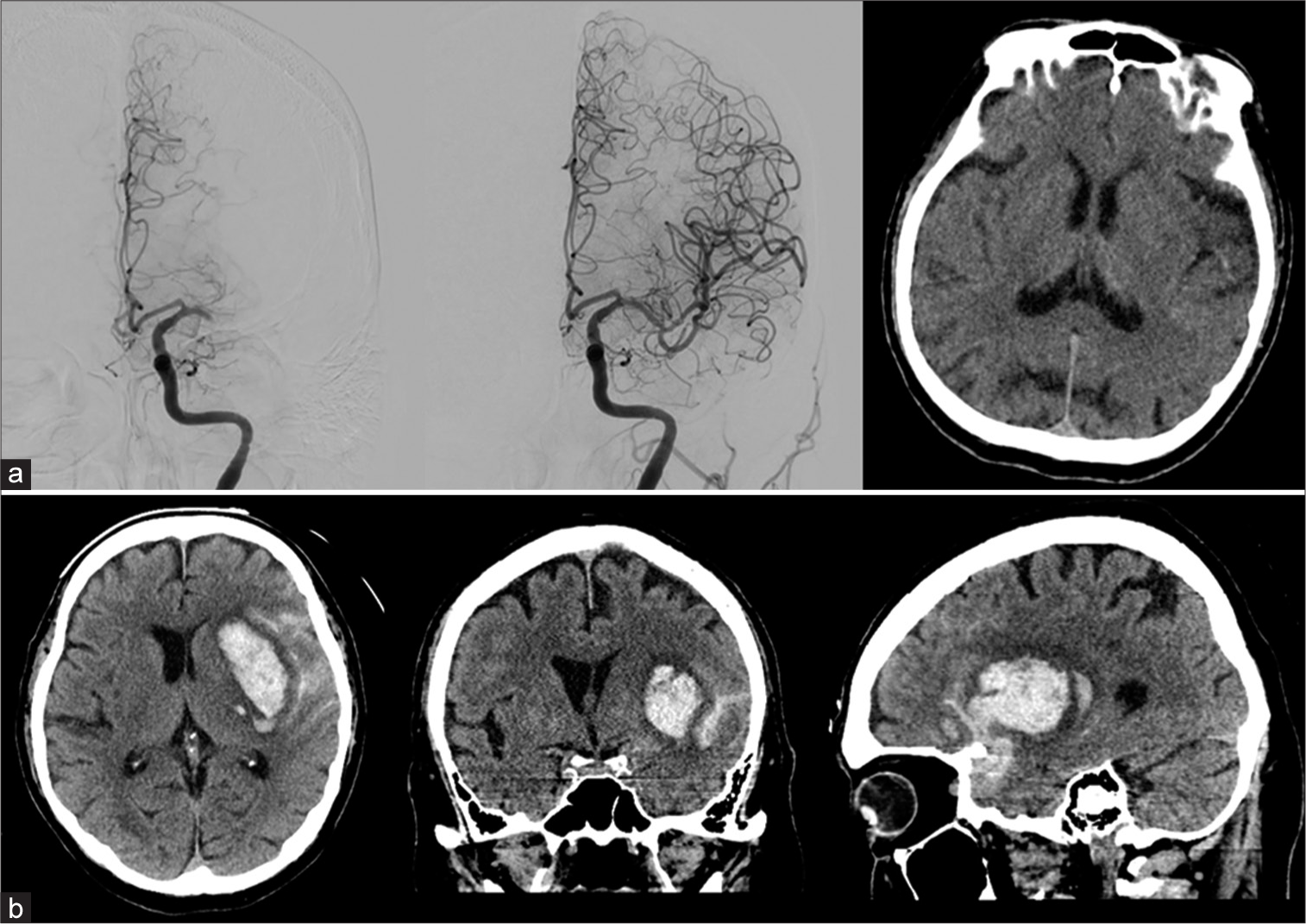
A 73-year-old man underwent tissue plasminogen activator intravenous therapy and thrombectomy for the left middle cerebral artery (MCA) occlusion due to cardiogenic embolism, resulting in total recanalization. There was no postoperative bleeding [
METHODS
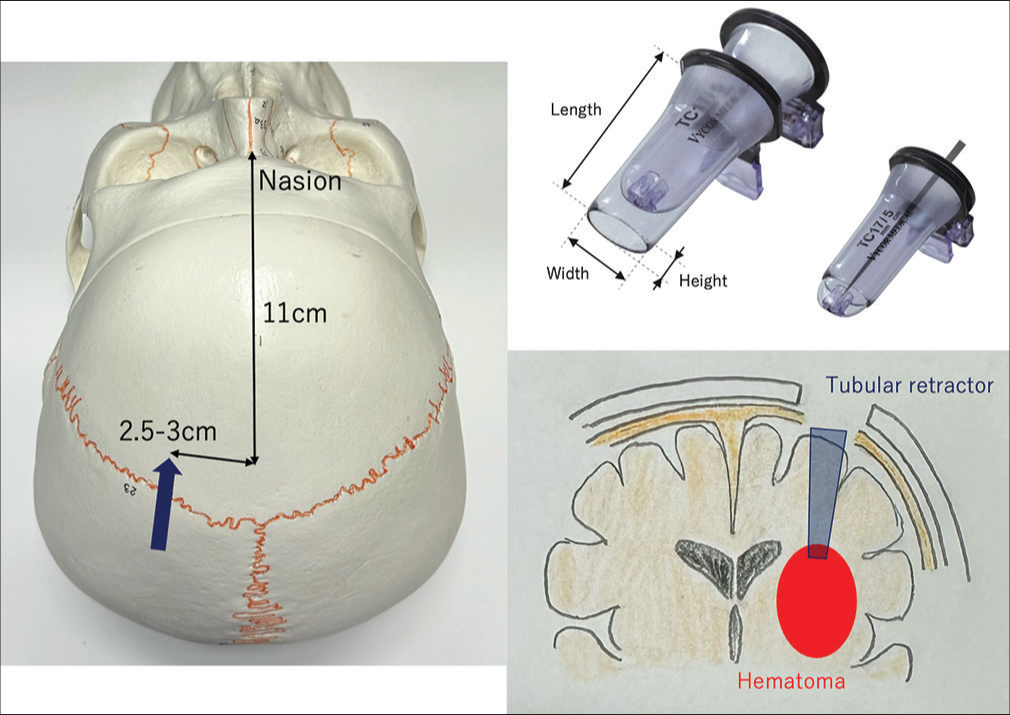
We usually perform craniotomy and removal of hematoma using a transsylvian approach for putaminal hemorrhage. In this case, it was thought that the Sylvian fissure would be difficult to remove due to SAH. In addition, although the bleeding was counterbalanced, he was taking anticoagulants and wanted to keep the bleeding as small as possible. Therefore, we devised craniotomy with an endoscopic approach in mind and planned to perform the surgery by inserting a tubular retractor through Kocher’s point [
Video 1
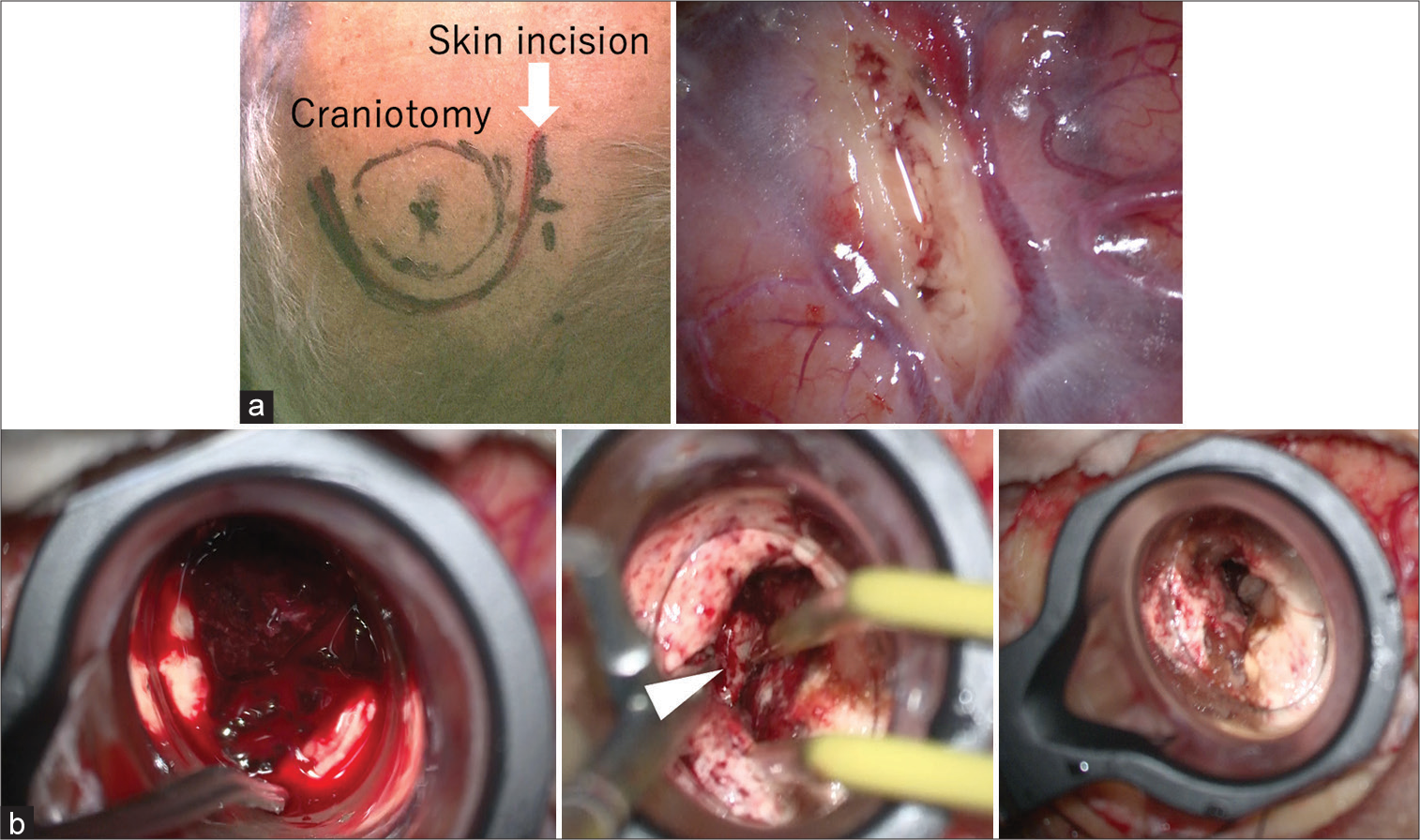
A 3–4 cm craniotomy centered at Kocher’s point [
RESULTS
Thanks to the tubular retractor, it was simple to observe the hematoma cavity, and it was possible to remove the hematoma and confirm hemostasis without difficulty [
DISCUSSION
Endoscopic surgery and stereotactic surgery have been established as minimally invasive surgery for putaminal hemorrhage.[
Since this approach imitates the approach of endoscopic removal of hematoma, it is extremely mini-invasive, even though it is a craniotomy. Normally, craniotomy can be performed centered on Kocher’s point (11 cm behind the nasion, 2.5–3 cm lateral to the midline), but this may vary depending on the location and direction of the hematoma, so measurements using preoperative images are required. In this case, surgery was performed after confirming the location of the hematoma directly below the Kocher’s point using preoperative CT.
There are many reports of surgeries using tubular retractors, such as ViewSite, for intraventricular approaches and deep brain tumors.[
ViewSite has an oval cavity that reduces the injury by insertion. The transparent design allows for clear visibility and makes it easy to check for bleeding within the tract. There are variations in size (12 mm × 8 mm, 17 mm × 11 mm, 21 mm × 15 mm, 28 mm × 20 mm) and length (3, 5, 7 cm), and in this case, 21 mm × 15 mm × 7 cm was selected. The distance from the brain surface to the hematoma was about 5 cm, but since it is necessary to thoroughly observe the depths of the hematoma cavity, especially when stopping bleeding, we think that it is better to choose a longer retractor. Because the field of view is wider than that of an endoscope, the inside of the hematoma cavity can be observed very clearly, and hemostasis can be performed without difficulty.
Points to note are that a corticotomy large enough to insert this retractor is required, and the cortical incision and tract width are larger than in endoscopic or stereotactic surgery. After the hematoma was removed, no active bleeding was observed within the tract, but some contusion was still observed. Therefore, it appears that the injury to the cavity was minimal. There should be no problem if the retractor is inserted directly below the hematoma, but if it becomes displaced, complications due to injury to anatomically important fibers may occur. These fibers include the coronal radiata, internal capsule, arcuate fasciculus, superior longitudinal fasciculus, superior occipitofrontal fasciculus, and projection fibers. Since the surgical field is deep, longer bipolar forceps and suction tubes may be required, which may make it more difficult for surgeons who are not accustomed to operating in deep fields. In addition, this approach is considered unsuitable when the hematoma is in a posterior position, such as when it extends to the thalamus.
In previous reports, the operating times for endoscopic surgery and craniotomy for intracerebral hemorrhage were 1.6 ± 0.7 h and 5.2 ± 1.8 h,[
Limitation
This is the author’s first attempt at this surgical method, and it is necessary to accumulate more cases in the future to examine the surgical outcomes. Furthermore, although the hematoma in this case was associated with SAH, its shape was not complicated, and removal was not difficult. Future studies will also be needed to determine whether it is effective against large or complex hematoma.
CONCLUSION
For putaminal hemorrhage, craniotomy was performed using a tubular retractor and an approach such as endoscopic surgery. This method is considered to be extremely minimally invasive in terms of craniotomy, removal of hematoma, and hemostasis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Capitanio JF, Donofrio CA, Panni P, Barzaghi LR, Bailo M, Gagliardi F. Microsurgical endoportal MRI/US-navigated approach for the resection of large intraventricular tumours: A 20-consecutive patients case series. Br J Neurosurg. 2021. 35: 570-7
2. Coscarella E, Vishteh AG, Spetzler RF, Seoane E, Zabramski JM. Subfascial and submuscular methods of temporal muscle dissection and their relationship to the frontal branch of the facial nerve. Technical note. J Neurosurg. 2000. 92: 877-80
3. Cuellar-Hernandez JJ, Lopez-Gonzalez MA, Olivas-Campos JR, Tabera-Tarello PM, Seanez-Prieto C, Eastin TM. The use of exoscope combined with tubular retractor system for minimally invasive transsulcal resection of an ventricular atrium atypical choroid plexus papilloma: Three-dimensional operative video. Surg Neurol Int. 2021. 12: 444
4. Fayad PB, Awad IA. Surgery for intracerebral hemorrhage. Neurology. 1998. 51: S69-73
5. Ibrahim N, Scullen T, Tucci M, Delashaw J, Khan P, Dumont A. Minimally invasive hematoma evacuation using the mindseye expandable tubular retractor: A technical note. World Neurosurg. 2023. 176: 162-7
6. Katsuki M, Kakizawa Y, Nishikawa A, Yamamoto Y, Uchiyama T. Endoscopic hematoma removal of supratentorial intracerebral hemorrhage under local anesthesia reduces operative time compared to craniotomy. Sci Rep. 2020. 10: 10389
7. Li B, Kim MG, Dominguez J, Feldstein E, Kleinman G, Hanft S. Intraventricular choroid plexus cavernoma resection using tubular retractor system and exoscope visualization: A technical case report. Oper Neurosurg (Hagerstown). 2022. 22: e134-7
8. Li Y, Yang R, Li Z, Yang Y, Tian B, Zhang X. Surgical evacuation of spontaneous supratentorial lobar intracerebral hemorrhage: Comparison of safety and efficacy of stereotactic aspiration, endoscopic surgery, and craniotomy. World Neurosurg. 2017. 105: 332-40
9. Marenco-Hillembrand L, Prevatt C, Suarez-Meade P, Ruiz-Garcia H, Quinones-Hinojosa A, Chaichana KL. Minimally invasive surgical outcomes for deep-seated brain lesions treated with different tubular retraction systems: A systematic review and meta-analysis. World Neurosurg. 2020. 143: 537-45.e3
10. Nishihara T, Teraoka A, Morita A, Ueki K, Takai K, Kirino T. A transparent sheath for endoscopic surgery and its application in surgical evacuation of spontaneous intracerebral hematomas. Technical note. J Neurosurg. 2000. 92: 1053-5
11. Okasha M, Ineson G, Pesic-Smith J, Surash S. Transcortical approach to deep-seated intraventricular and intra-axial tumors using a tubular retractor system: A technical note and review of the literature. J Neurol Surg A Cent Eur Neurosurg. 2021. 82: 270-7
12. Piloni M, Gagliardi F, Bailo M, Barzaghi LR, Caputy AJ, Mortini P. Endoscope-assisted neuroportal transcerebellar approach to the fourth ventricle: An anatomical study. J Neurol Surg A Cent Eur Neurosurg. 2021. 82: 248-56
13. Tanriover N, Rhoton AL, Kawashima M, Ulm AJ, Yasuda A. Microsurgical anatomy of the insula and the sylvian fissure. J Neurosurg. 2004. 100: 891-922
14. Valarezo-Chuchuca A, Morejón-Hasing L, Wong-Achi X, Egas M. Minimally invasive surgery with tubular retractor system for deep-seated or intraventricular brain tumors: Report of 13 cases and technique description. Interdisciplin Neurosurg. 2021. 25: 101260
15. Wang WH, Hung YC, Hsu SP, Lin CF, Chen HH, Shih YH. Endoscopic hematoma evacuation in patients with spontaneous supratentorial intracerebral hemorrhage. J Chin Med Assoc. 2015. 78: 101-7
16. Xu X, Chen X, Li F, Zheng X, Wang Q, Sun G. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage: A comparison with craniotomy. J Neurosurg. 2018. 128: 553-9
17. Zabramski JM, Kiris T, Sankhla SK, Cabiol J, Spetzler RF. Orbitozygomatic craniotomy. Technical note. J Neurosurg. 1998. 89: 336-41







Donald Ross
Posted June 4, 2024, 7:43 am
You did not cite my paper and description of a tubular brain retractor more than 30 years ago, nor Dr. Patrick Kelly’s seminal work on tubular retractors in the 1980’s as well. Credit should be given, as these systems are not new or novel at this point.
See Ross DA: A simple stereotactic retractor for use with the Leksell stereotactic apparatus. Neurosurgery 32:475-476, 1993 PMID 8455778