- Department of Neurosurgery, University Hospital of Wales, Cardiff, South Wales, United Kingdom.
- Department of Neurology, University Hospital of Wales, Cardiff, South Wales, United Kingdom.
Correspondence Address:
Lindsey Bulleid
Department of Neurosurgery, University Hospital of Wales, Cardiff, South Wales, United Kingdom.
DOI:10.25259/SNI_625_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lindsey Bulleid1, Tom Hughes2, Paul Leach1. Mollaret’s triangle: An important neuroanatomical territory for all clinicians. 08-Mar-2021;12:94
How to cite this URL: Lindsey Bulleid1, Tom Hughes2, Paul Leach1. Mollaret’s triangle: An important neuroanatomical territory for all clinicians. 08-Mar-2021;12:94. Available from: https://surgicalneurologyint.com/surgicalint-articles/10629/
Abstract
Background: Hypertrophic olivary degeneration is a rare condition caused by damage within the triangle of Guillain and Mollaret. We discuss the anatomical, radiological, and clinical history of this rare condition.
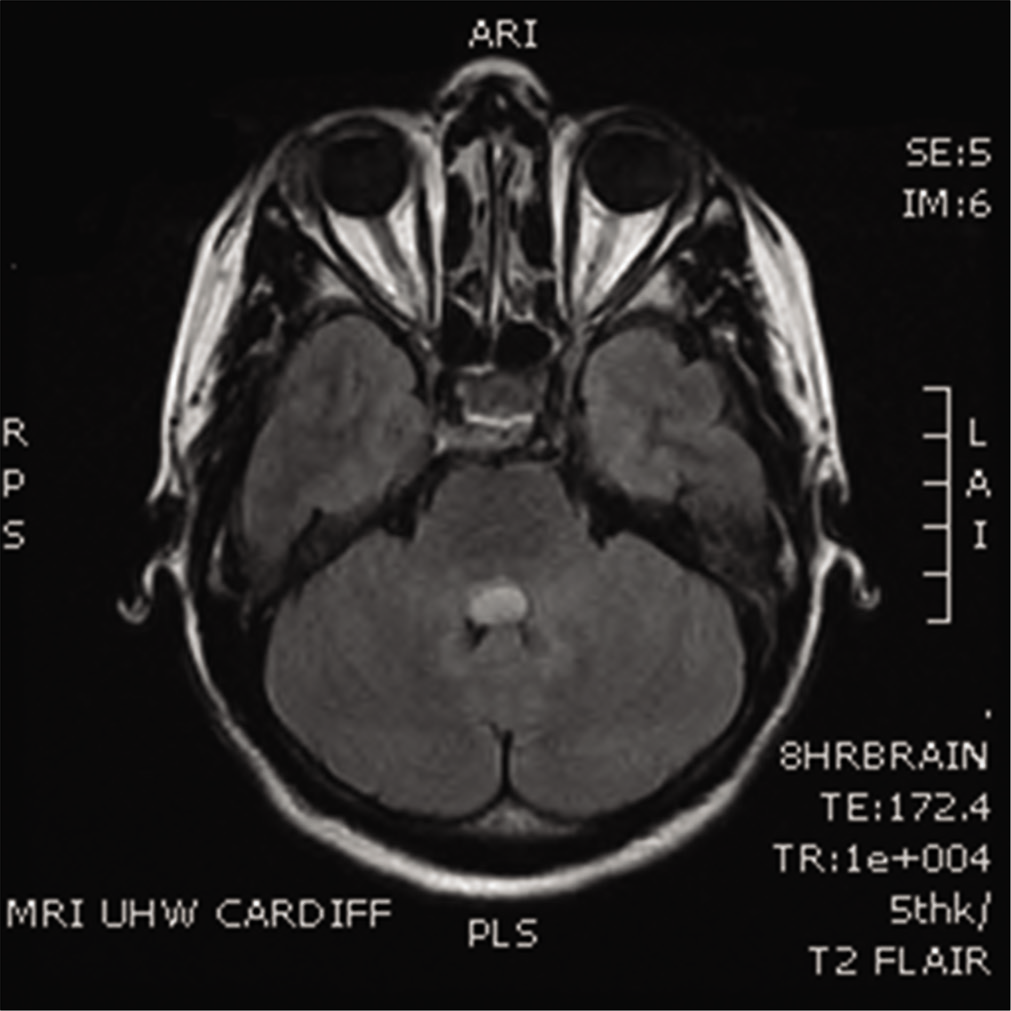
Case Description: A 32-year-old lady presented with sub-acute headache, photophobia, and dizziness. She also described facial tingling and itching over her nose, and a thirty-minute episode of slurred speech. Magnetic resonance imaging revealed a 12.1 × 11 × 7.3 mm lesion arising from the floor of the fourth ventricle [
Conclusion: An awareness of this complication is of importance to all clinical neuroscience to prevent misdiagnosis with the occurrence of new symptoms.
Keywords: Cervical myoclonus, Fourth ventricular tumor, Hypertrophic olivary degeneration, Oscillopsia, Palatal myoclonus, Triangle of Guillain and Mollaret
INTRODUCTION
Hypertrophic olivary degeneration is a rare condition caused by damage within the triangle of Guillain and Mollaret. We describe a clinical case where this occurred and discuss the anatomical, radiological and clinical history of this rare condition.
CASE SUMMARY
A 32-year-old female presented with sub-acute headache, photophobia, and dizziness. Magnetic resonance imaging revealed a 12.1 × 11 × 7.3 mm lesion arising from the floor of the fourth ventricle [
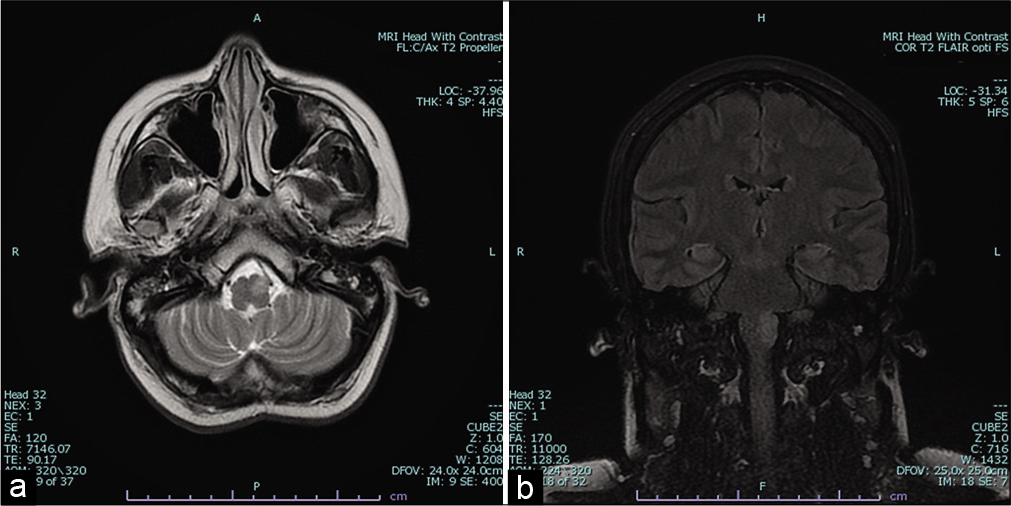
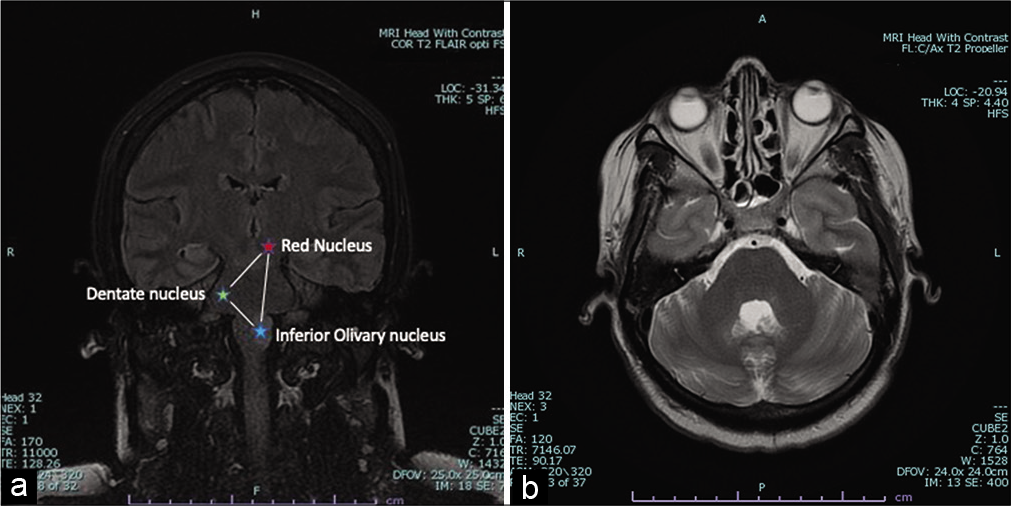
Figure 2:
(a) Axial T2-weighted magnetic resonance image showing signal increase in the anterior medulla oblongata (more pronounced on the left) consistent with hypertrophic olivary degeneration. (b) Coronal T2 FLAIR magnetic resonance image showing hyperintensity over the region of the inferior olivary nucleus.
DISCUSSION
Hypertrophic olivary degeneration is a rare condition caused by damage within the triangle of Guillain and Mollaret.[
Olivary hypertrophy develops within 6 months of the initial event and resolves within 3–4 years.[
The most common clinical presentation is of palatal or oculopalatal myoclonus, weeks to months after the initial insult.[
CONCLUSION
This case provides an opportunity to review clinical anatomy, radiological change and neurology, and is an interesting illustration of a rare complication of fourth ventricular surgery. It demonstrates the intricacy of brainstem function and the variable relationship between radiological hypertrophy of the olivary nucleus and clinical symptoms, providing an important reminder of key functional anatomy and pathology.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cosentino C, Velez M, Nuñez Y, Palomino H, Quispe D, Flores M. Bilateral hypertrophic olivary degeneration and holmes tremor without palatal tremor: An unusual association. Tremor Other Hyperkinet Mov (N Y). 2016. 6: 400
2. Goyal M, Versnick E, Tuite P, Cyr JS, Kucharczyk W, Montanera W. Hypertrophic olivary degeneration: Metaanalysis of the temporal evolution of MR findings. AJNR Am J Neuroradiol. 2000. 21: 1073-7
3. Khoyratty F, Wilson T. The dentato-rubro-olivary tract: Clinical dimension of this anatomical pathway. Case Rep Otolaryngol. 2013. 2013: 934386
4. Manzano-Lopez Gonzalez D, Conesa Bertran G, Lafuente Baraza J. Unusual case of posterior fossa syndrome and bilateral hypertrophic olivary degeneration after surgical removal of a large fourth ventricle ependymoma in an adult. Acta Neurochir (Wien). 2015. 157: 1271-3
5. Martins WA, Marrone LC, Soder RB, da Costa JC. Hypertrophic olivary degeneration: Unveiling the triangle of Guillain-Mollaret. Arq Neuropsiquiatr. 2016. 74: 426-7






Ellen Tribuci
Posted January 5, 2023, 7:08 am
Hi. I think this is the first article I found about Guillain Mollaret, that my mom was diagnosed in 2018, and at that time, we didn´t have anything to understand.
In this study or even in this forum, is there some treatment for this? Even to avoid the degeneration that affects her balance, could stop or even return to normal?
I would appreciate it if someone could give me some hope because it seems that it starting to be more complicated for her to walk alone.