- Department of Surgery, Faculty of Medicine, Prince of Songkla University, Songklanagarind Hospital, Hat Yai, Songkhla, Thailand.
- Department of Otolaryngology Head and Neck Surgery, Faculty of Medicine, Prince of Songkla University, Songklanagarind Hospital, Hat Yai, Songkhla, Thailand.
- Department of Radiology, Faculty of Medicine, Prince of Songkla University, Songklanagarind Hospital, Hat Yai, Songkhla, Thailand.
- Department of Anesthesiology, Faculty of Medicine, Prince of Songkla University, Songklanagarind Hospital, Hat Yai, Songkhla, Thailand.
Correspondence Address:
Anukoon Kaewborisutsakul, Department of Surgery, Faculty of Medicine, Prince of Songkla University, Songklanagarind Hospital, Hat Yai, Songkhla, Thailand.
DOI:10.25259/SNI_506_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Thakul Oearsakul1, Anukoon Kaewborisutsakul1, Kitti Jantharapattana2, Rujimas Khumtong3, Asamaporn Puetpaiboon4, Burapat Sangthong1. Multidisciplinary management of a penetrating cerebellar injury by a fishing speargun: A case study and literature review. 03-Aug-2021;12:391
How to cite this URL: Thakul Oearsakul1, Anukoon Kaewborisutsakul1, Kitti Jantharapattana2, Rujimas Khumtong3, Asamaporn Puetpaiboon4, Burapat Sangthong1. Multidisciplinary management of a penetrating cerebellar injury by a fishing speargun: A case study and literature review. 03-Aug-2021;12:391. Available from: https://surgicalneurologyint.com/surgicalint-articles/11010/
Abstract
Background: Fishing spearguns are a rare cause of nonmissile penetrating brain injuries (PBIs). Discussion of their injury patterns and treatments has been published only sporadically. Here, we report a case of a self-inflicted PBI caused by this type of weapon and present an extensive review of previous case reports to help ascertain the appropriate surgical approach.
Case Description: A 26-year-old man with a preexisting psychiatric illness was transferred to our hospital after a self-inflicted shot with a fishing speargun through his mouth. The ensuing injuries included the impalement of a spear intracranially through the soft palate and posterior oropharyngeal wall. The spear was surgically accessed by the otolaryngology team by splitting the soft palate and was removed by the neurosurgery team in the retrograde direction. Cerebral angiographies were done pre- and postoperatively, and these did not detect any vertebrobasilar arterial system injuries. The patient’s postoperative care was uneventful, and he was followed up by a psychiatrist for his long-term care.
Conclusion: This example of a complicated case of nonmissile PBI caused by an uncommon type of weapon shows how this type of medical emergency can be managed successfully with effective teamwork using a multidisciplinary approach.
Keywords: Foreign body, Harpoon, Neurotrauma, Penetrating brain injury, Systematic review
INTRODUCTION
Penetrating brain injury (PBI) is serious, with a high mortality and morbidity rate.[
Intracranial injuries due to a fishing speargun or harpoon are rare. In the past, injuries from such weapons were often accidental[
This report discusses the case of a patient who attempted suicide with a fishing speargun and sustained an infratentorial injury. Moreover, we review previous case reports of PBIs using this weapon to analyze and summarize the most effective treatment strategy for the optimal management of this type of injury.
CASE DESCRIPTION
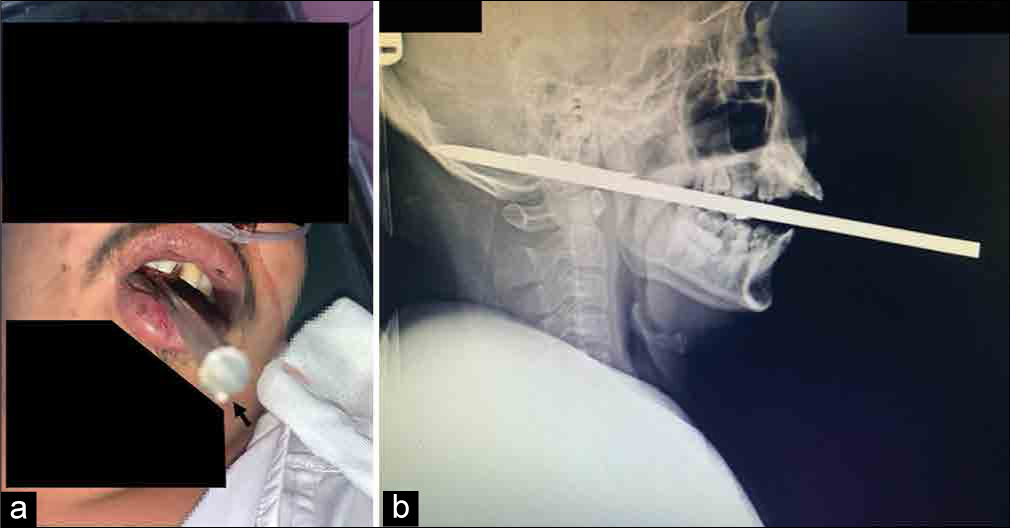
This case involved a 26-year-old man who was being treated for a psychiatric disorder. On the day of presentation, his relatives found him lying on the bedroom floor. There was a speargun rod in his mouth, and he was bleeding, including from his nose. On inquiring the history, we learned that the patient had shot himself with a rubber band speargun. At the scene, the patient was conscious and showed no weakness; hence, the relatives took him to the nearest community hospital.
According to the patient’s treatment history at that hospital, the spear was cut short, just approximately 10 cm off the edge of the patient’s lips. He was calm, breathed well, and had normal vital signs without any neurological deficits. The patient received oxygen through a nasal cannula and was administered tetanus toxoid and intravenous antibiotics. In addition, he underwent cranial X-ray [
At our hospital, a multidisciplinary team of neurosurgeons, trauma surgeons, otolaryngologists, interventional neurologists, and anesthesiologists was established urgently to assess the patient. Initially, the patient’s vital signs and symptoms were normal. In addition, no bleeding was observed in the upper aerodigestive tract. On physical examination, an 8 mm diameter round iron spear was found to have penetrated through his soft palate and the posterior oropharyngeal wall.
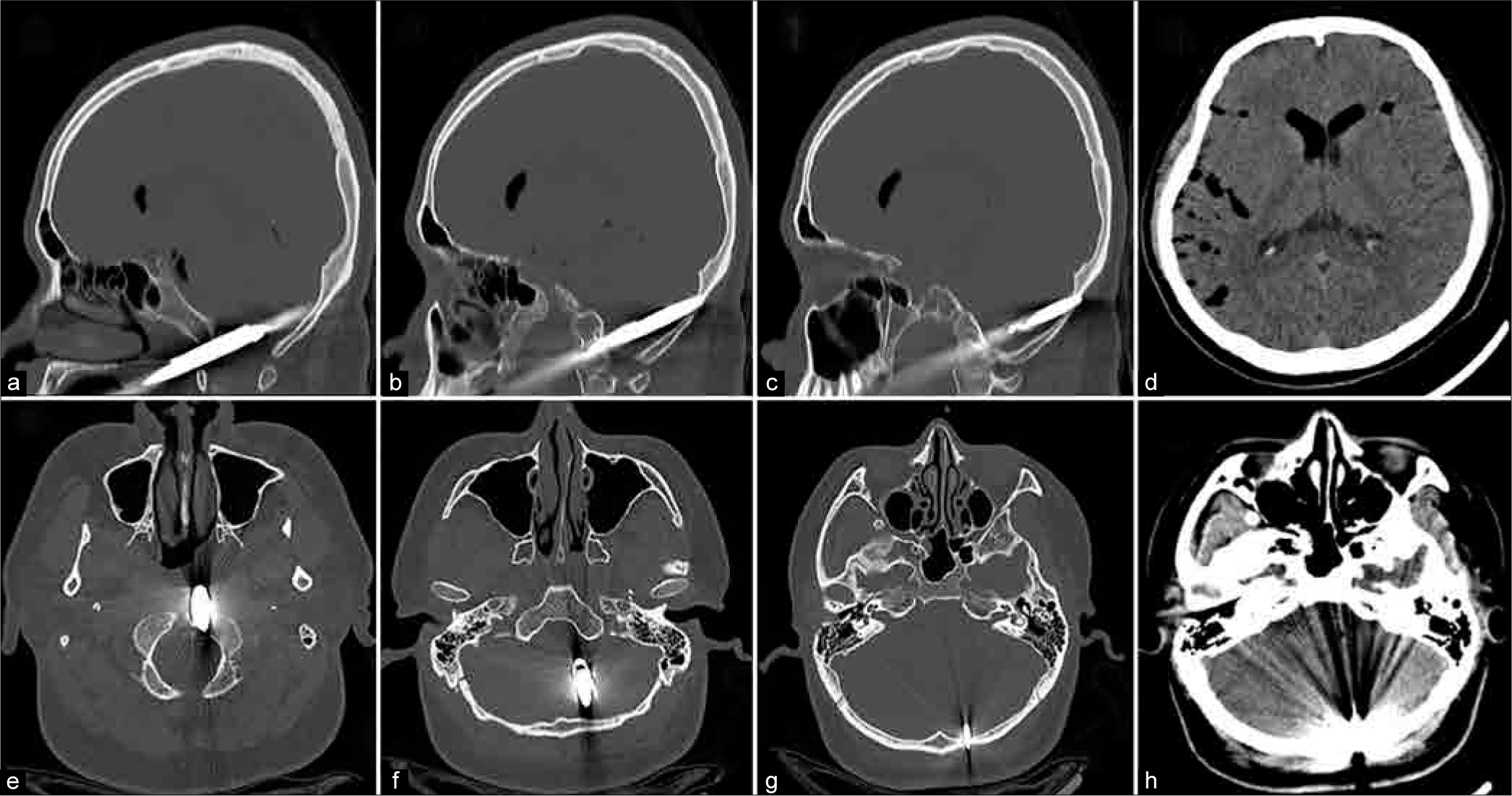
Cranial computed tomography (CT) scan showed a metallic rod that had penetrated through the oropharynx, the left side of the clivus, and the left lateral part of the posterior fossa. The rod was positioned slightly above the foramen magnum and ended in the left cerebellar hemisphere. The spear’s tip was located at the inner cortex of the left side of the occipital bone [
Figure 2:
Cranial computed tomography (CT). Sagittal views (a-c) and axial views (e-g) of bone window showing the spear trajectory – entrance, path, and end of spear tip. Axial views of plain CT, soft-tissue window showing multiple pneumocephali along cerebral sulci and pneumoventricles in the frontal horns of lateral ventricles (d). No cerebellar hemorrhage observed (h).
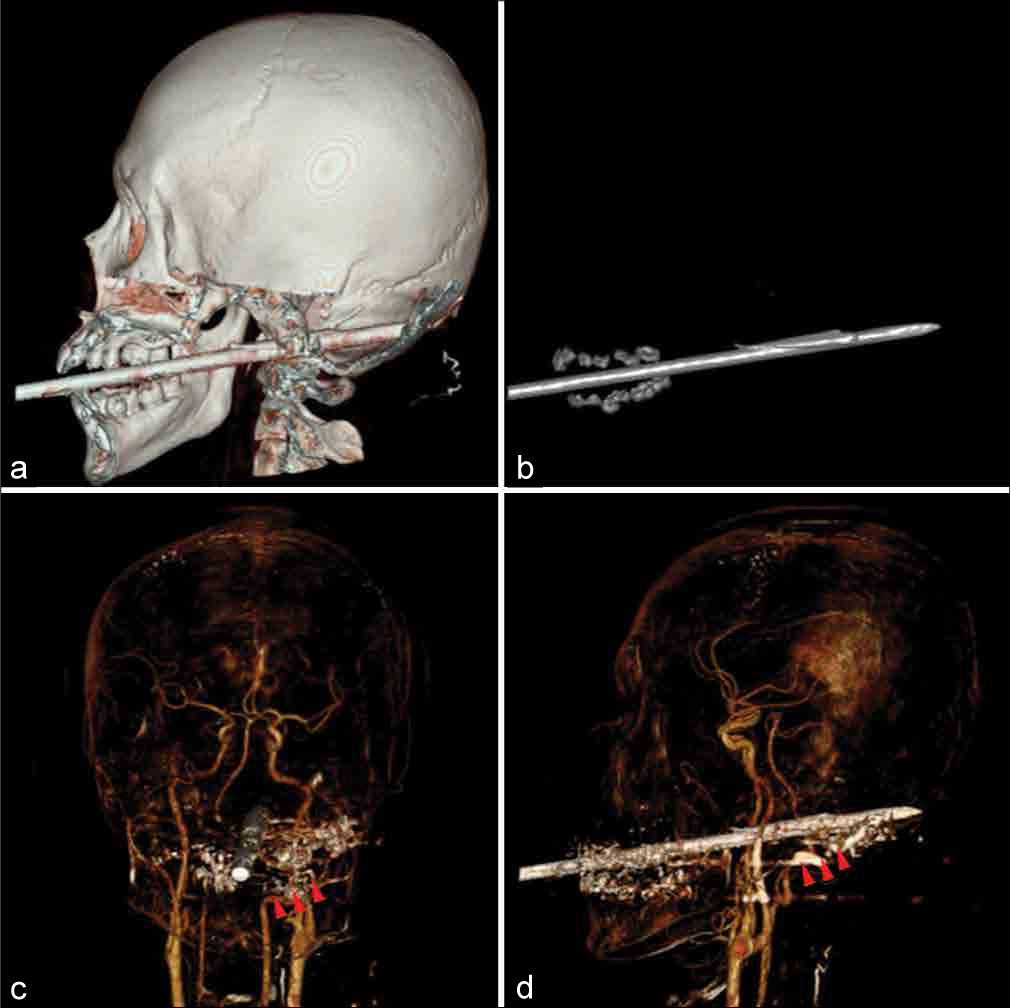
Three-dimensional (3D) CT reconstruction images revealed the details of the spear; it had a harpoon (or flapper), with the most convex part of the metallic tip of the spear acting as a hinge. This section was located within the clivus bone, with the end of the flapper having partially penetrated the intracranial cavity [
Figure 3:
(a) Cranial 3D computed tomography scan (3D-CT), lateral view, demonstrating the spear direction passing the clivus to the occipital bone. (b) The spear characteristics were revealed after subtracting skull out corresponding with “one-flapper type” of spear’s tips. (c and d) Computed tomography angiography reconstruction on AP (c) and lateral (d) views revealing the trajectory of the spear is close to the left vertebral artery with multiple metallic artifacts (head arrows).
Treatment began with airway management. The patient could open his mouth only one finger wide. Therefore, the anesthesiologist performed nasotracheal intubation using the awake fiber-optic technique during which the patient cooperated well [
Figure 4:
Intraoperative photographs showing (a) the patient position after fiber-optic intubation, and (b) the application of the Dingman mouth retractor to open the patient’s mouth and the splitting of the soft palate. The spear is shown entering the posterior oropharyngeal wall. (c) Photograph showing the spear after removal; it had a one flapper (harpoon) tip and was 26 cm in length.
Figure 5:
Diagnostic digital subtraction angiography (DSA) demonstrating a normal left vertebral artery located just adjacent to the spear on anterior-posterior (AP) (a) and oblique views (b). A 3D DSA was subsequently done and confirm no visualized injuries of the left vertebral artery and surrounding vessels (not shown). The arrow is pointing the spear abutting the left vertebral artery before removal (a and b). The AP (c) and lateral views (d) of a left vertebral angiography after spear removal showing normal vessels without secondary false aneurysms or developed extravasations.
Otolaryngologists operated on the patient starting with a tracheostomy because the nasotracheal tube obstructed the surgical spear removal path. Then, the surgeon opened the patient’s mouth with a Dingman retractor and separated the soft palate as well as the posterior pharyngeal wall at the median. The neurosurgery team further exposed the soft tissue surrounding the spear until the end of the flapper could be located. Under a microscope, the team members then drilled the clivus bone that surrounded and covered the flapper. When the spear was gently pulled out, slight bleeding occurred from the clivus bone, which was successfully stopped using bone wax.
There was fortunately no continuous intracranial bleeding. A thorough rinsing was performed with a large amount of saline solution, and all visible bleedings were coagulated. Then, the dural defect was repaired with a dural substitute and tissue sealant. Finally, the posterior pharynx was closed tightly; the soft palate was repaired and reapproximated.
After removing the spear, angiographic findings concerning the intracranial arteries were found to be normal, both immediately [
The patient also underwent psychiatric evaluation and was diagnosed with adjustment disorder, which was treated with medications and emotional support. He was finally discharged on postoperative day 19. His mental state was normal, and he no longer had any suicidal ideation.
DISCUSSION
The patient had a good outcome because of the effectively planned treatment by the interdisciplinary medical team and the appropriate use of the available medical resources.
Fishing spearguns are a cause of nonmissile PBIs. The first such case was reported by Paillas and Legre in 1956.[
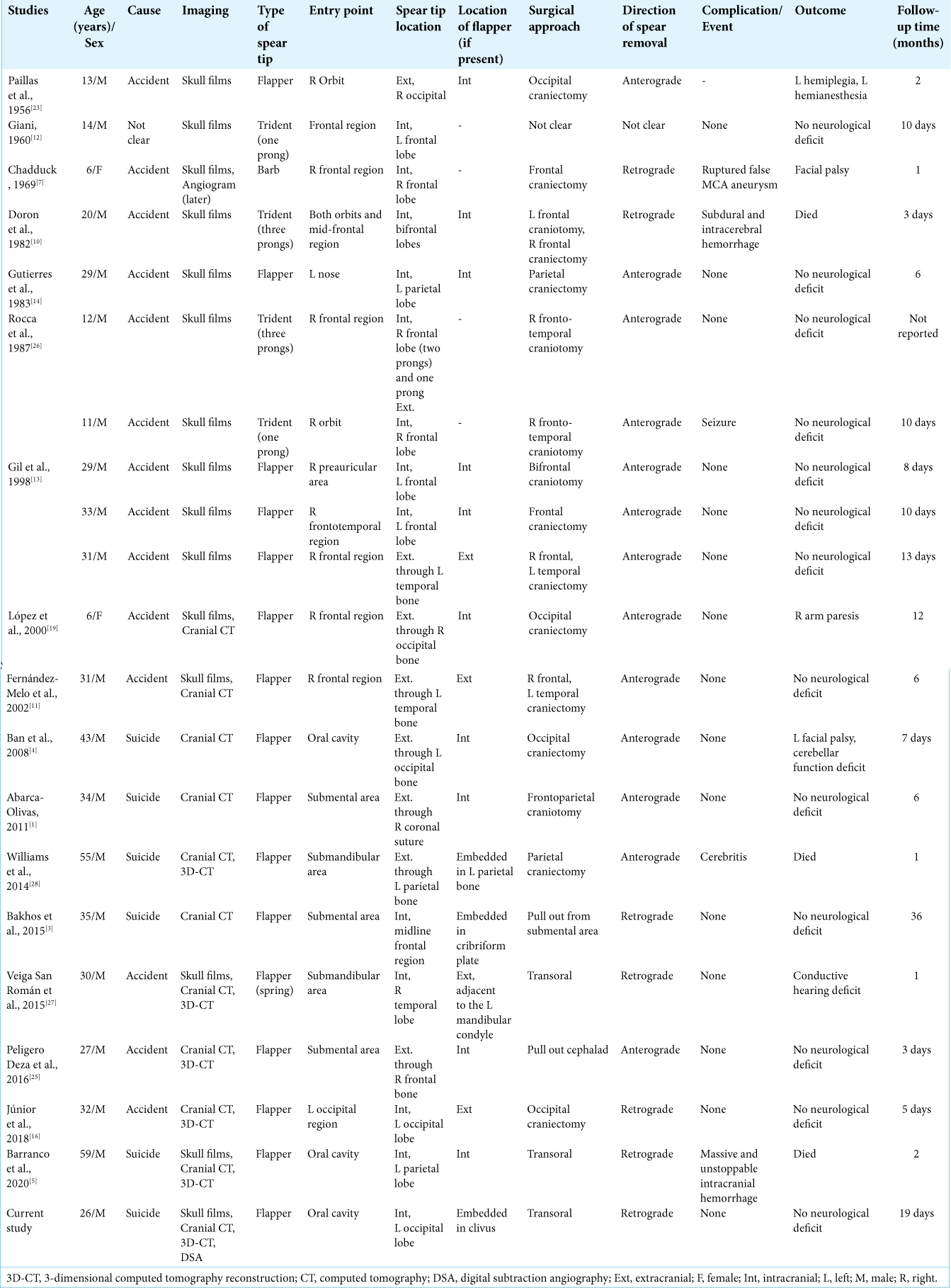
To provide a better quality of care for those injured from this type of weapon, we searched the PubMed database from 1977 until May 2021 for fishing speargun injuries using the search terms “fishing,” “speargun,” “harpoon,” “trauma,” and “brain injury,” which were combined in various ways using the “OR” and “AND” search strategy. We included studies published in all languages. A citation within relevant articles was also further reviewed. However, studies with postmortem and forensic studies[
Most of these injuries occur in males between the ages of 6 and 55 years, and the most common cause is an accident occurring while fishing. The second most common cause is suicide attempts.[
For surgical planning, spear trajectory, injured organs (e.g., brain and blood vessels), and spear tip characteristics and position are important aspects that need to be considered. In addition, concomitant injuries and the patient’s preinjury health status should be taken into account.
The spear trajectory is directly related to the location of the brain injury. Locations that are near major arteries or venous sinuses increase the risk of vascular injury.[
According to the PBI guidelines,[
Studying the composition of weapons is an important issue in surgical planning involving such cases, particularly the spear tip characteristics. In general, there are two types of spears – single rods and tridents. The tip of a single rod spear is generally attached to a hinged device called a harpoon or flapper tip, which may have 1–2 flappers; in some cases, it can have a spring flapper. A trident has three prongs that usually have no hinges, and the tips of the prongs have barbs.[
We propose a surgical approach guided by the type of spear tip and its location. For barbed tips, the spear can be pulled out either in line with the trajectory, that is, in the anterograde direction or in the opposite line of the trajectory, that is, in the retrograde direction. In addition to the position of the tip’s end, the direction of removal depends on the closeness of the tip to the surface of the adjacent cortex. In the case of flapper tips, the flapper is characterized by a hinge that can be unfolded when a substantial amount of tissue is blocking the flapper end; it is designed in this manner to prevent the fish escaping from the spear while fishing. The flapper position is an important point, particularly for cases in which the flapper is entirely intracranial or penetrates outside the cranium. Therefore, it is recommended to pull the spear out in the anterograde direction because pulling the spear in the retrograde direction can cause the flapper to spread and cause further brain parenchymal tearing.[
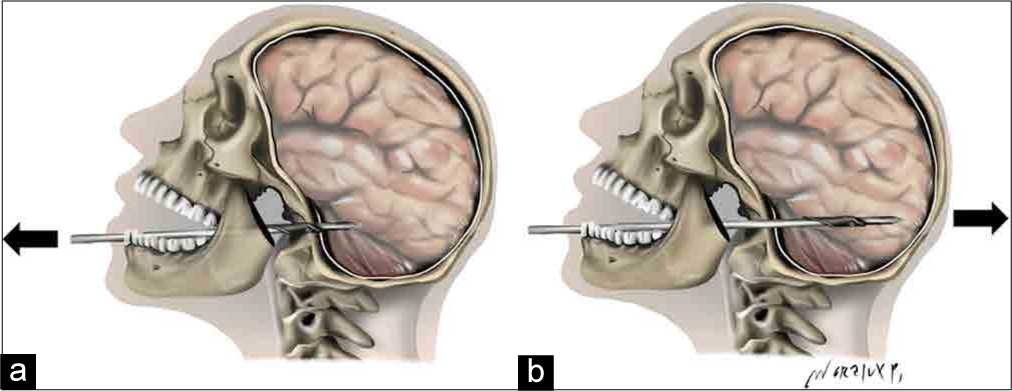
Figure 6:
The proposed direction of spear removal in a flapper type speargun injury. (a) The flapper is embedded within the skull base. The authors suggest removing the spear in a retrograde direction (arrow). (b) The flapper is embedded within the intracranial compartment. The authors suggest removing the spear in an anterograde direction (arrow).
Antibiotics and antiepileptic drug treatments were used in most previous reports. However, varied practices were followed regarding the choice of drugs, their dosage, and duration of use.
With respect to airway management, procedures to secure airway should be planned thoroughly as a team approach, which comprised anesthesiologists and otolaryngologists in the present case. Instruments involving airway procedures should be prompt in diminishing the risk of airway loss, which can prove fatal. At least one or more back up plans for airway retrieval should be prepared for patient safety.
Finally, assessing mental status and providing adequate treatment for the underlying medical problems of suicide survivors are important for enhancing both the patient’s quality of life and ongoing care.[
CONCLUSION
The management of nonmissile PBI is challenging due to unfamiliarity with this type of injury because of its rarity and the fact that it involves both the intracranial and extracranial organs. When the fishing speargun is used as a weapon for suicide, it is associated with high mortality. In such cases, surgical planning for foreign body removal is critical. This planning depends on the injured organs, spear trajectory, and the type and position of the spear tip. A multidisciplinary team is required to overcome the challenges posed by this unique emergency.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful for the excellent manuscript editing and proofreading by Mr. Edmond Subashi, Faculty of Medicine, Prince of Songkla University, and for the beautiful illustration by Woralux Phusoongnern, Neurosurgeon, Neurosurgical unit, Chiangmai Neurological Hospital, Chiangmai, Thailand.
References
1. Abarca-Olivas J, Concepción-Aramendía LA, Baño-Ruiz E, Caminero-Canas MA, Navarro-Moncho JA, Botella-Asunción C. Perforating brain injury from a speargun. A case report. Neurocirugia (Astur). 2011. 22: 271-5
2. Alper M, Totan S, Cankayali R, Songur E. Maxillofacial spear gun accident: Report of two cases. J Oral Maxillofac Surg. 1997. 55: 94-7
3. Bakhos D, Villeneuve A, Kim S, Lebrun H, Dufour X. Head spear gun injury: An atypical suicide attempt. J Craniofac Surg. 2015. 26: e547-8
4. Ban LH, Leone M, Visintini P, Blasco V, Antonini F, Kaya JM. Craniocerebral penetrating injury caused by a spear gun through the mouth: Case report. J Neurosurg. 2008. 108: 1021-3
5. Barranco R, Caputo F, Pinto SL, Drommi M, Ventura F. Unusual suicide by a speargun shot: Case report. Medicine (Baltimore). 2020. 99: e22308
6. Bonsignore A, Bernucci LV, Canepa M, Ventura F. Suicide due to four speargun shots: A case report. Am J Forensic Med Pathol. 2013. 34: 201-4
7. Chadduck WM. Traumatic cerebral aneurysm due to speargun injury. Case report. J Neurosurg. 1969. 31: 77-9
8. Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, Large MM. Suicide rates after discharge from psychiatric facilities: A systematic review and meta-analysis. JAMA Psychiatry. 2017. 74: 694-702
9. Costantinides F, Russo V, Altamura BM. Speargun injuries: A case of wilful murder. Acta Med Leg Soc (Liege). 1989. 39: 73-6
10. Doron Y, Gruszkiewicz J, Peyser E. Penetrating cranio-cerebral injuries due to unusual foreign bodies. Neurosurg Rev. 1982. 5: 35-40
11. Fernández-Melo R, Morán AF, López-Flores G, BouzaMolina W, García-Maeso I, Benavides-Barbosas J. Trauma craneoencefálico perforante por arpón. Precentación de un caso y revisión de la literatura [Penetrating head injury from harpoon, Case report]. Neurocirugia (Astur). 2002. 13: 397-400
12. Giani E. Injury of the left cerebral hemisphere by the trident from an underwater fishing gun. Riforma Med. 1960. 74: 589-90
13. Gil CJ, Acosta RC, Felipe MA, Alemán A, Pérez VF. Consideraciones y proceder quirúrgico en las heridas craneocerebrales por arpón. Rev Cuba Med Mil. 1998. 27: 133-40
14. Gutierrez A, Gil L, Sahuquillo J, Rubio E. Unusual penetrating craniocerebral injury. Surg Neurol. 1983. 19: 541-3
15. Harrington BM, Gretschel A, Lombard C, Lonser RR, Vlok AJ. Complications, outcomes, and management strategies of non-missile penetrating head injuries. J Neurosurg. 2020. 19: 1-9
16. Júnior SR, Cohen MI, Chaves RA, Teixeira MA, Ellakkis RF, Meguins LC. Unusual penetrating cranioencephalic injury by a harpoon in a Brazilian man. J Bras Neurocir. 2018. 23: 342-5
17. Kataria R, Singh D, Chopra S, Sinha VD. Low velocity penetrating head injury with impacted foreign bodies in situ. Asian J Neurosurg. 2011. 6: 39-44
18. Li XS, Yan J, Liu C, Luo Y, Liao XS, Yu L. Nonmissile penetrating head injuries: Surgical management and review of the literature. World Neurosurg. 2017. 98: 873.e9-25
19. López F, Martínez-Lage JF, Herrera A, Sánchez-Solís M, Torres P, Palacios MI. Penetrating craniocerebral injury from an underwater fishing harpoon. Childs Nerv Syst. 2000. 16: 117-9
20. McGuire M. Spearfishing Manual: Insider Secrets Revealed. Available from: https://www.overdrive.com/search?q=30b2f3b5-ed9d-4908-bcd7-0da6984210bb [Last accessed on 2021 Apr 01].
21. . Neuroimaging in the management of penetrating brain injury. J Trauma. 2001. 51: S7-11
22. Nouma Y, Krimi S, Regaieg K. Unusual suicide by a speargun shot through the mouth: A case report. Am J Forensic Med Pathol. 2018. 39: 73-7
23. Paillas JE, Legre J. Un corps étranger intracranien peu banal; blessure par flèche de harpon sous-marin [Unusual intracranial foreign body; wound by submarine harpoon spear]. Presse Med. 1956. 64: 977-8
24. . Part 2: Prognosis in penetrating brain injury. J Trauma. 2001. 51: S44-86
25. Peligero Deza J, Marín Zaldivar C, García Aguirre L, Casans Francés R. Traumatismo craneoencefálico severo por arpón de pesca [Severe head trauma by speargun]. Rev Esp Anestesiol Reanim. 2016. 63: 186-7
26. Rocca A, Casu G, Sechi CS. Penetrating craniocerebral injuries. Report of two unusual cases. J Neurosurg Sci. 1987. 31: 19-21
27. Veiga San Román P, Sánchez PM, Garcia MG, Bergada MV, San Vicente VV, Tovar TP. Traumatismo penetrante facial por arpón. A propósito de un caso. Rev Esp Cir Oral Maxilofac. 2015. 37: 27-31
28. Williams JR, Aghion DM, Doberstein CE, Cosgrove GR, Asaad WF. Penetrating brain injury after suicide attempt with speargun: Case study and review of literature. Front Neurol. 2014. 5: 113