- Service de Neurochirurgie, Centre Hospitalier Universitaire Vaudois (CHUV) and University of Lausanne, Lausanne, Switzerland
- Department of Clinical Neurosciences and Department of Oncology, Centre Hospitalier Universitaire Vaudois, University of Lausanne, Lausanne, Switzerland
Correspondence Address:
Daniele Starnoni
Service de Neurochirurgie, Centre Hospitalier Universitaire Vaudois (CHUV) and University of Lausanne, Lausanne, Switzerland
DOI:10.4103/2152-7806.195588
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daniele Starnoni, Yves Yamgoué, Andreas Hottinger, Viktor Bartanusz. Multilevel severe radiculopathy from an extraneural glioblastoma cervical metastasis. 12-Dec-2016;7:
How to cite this URL: Daniele Starnoni, Yves Yamgoué, Andreas Hottinger, Viktor Bartanusz. Multilevel severe radiculopathy from an extraneural glioblastoma cervical metastasis. 12-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/multilevel-severe-radiculopathy-from-an-extraneural-glioblastoma-cervical-metastasis/
Keywords: Extraneural metastases, glioblastoma multiforme, vertebral metastases
In march 2016, a 42-year-old man presented at our institution with complaints of insidious neck pain irradiating to the right shoulder and a progressive weakness of the right upper limb.
In 2012, the patient had undergone a total resection of an isolated occipital lesion histologically reported as glioblastoma multiforme (GBM), with wild-type IDH1 and O-6-methylguanine-DNA methyltransferase (MGMT) methylation. He had received concurrent adjuvant local radiotherapy (60 Gy) and chemotherapy (temozolomide). Because of local recurrence, two successive total resections were performed in May 2014 and July 2015 followed by chemotherapy (Temozolomide). In October 2015, a new local recurrence invading the superior sagittal sinus was diagnosed and treated with cyber Knife radiosurgery and concurrent introduction of Bevacizumab and rindopepimut, an investigational immunotherapy that targets the tumor specific oncogene EGFRvIII, followed by a rapid regression in size of the lesion.
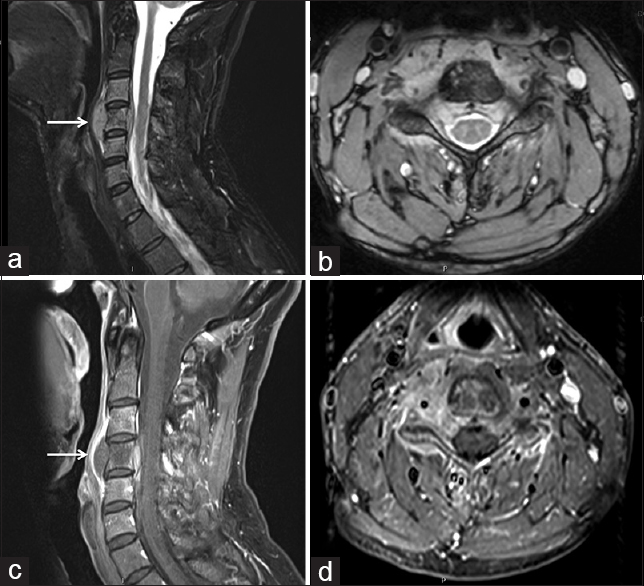
At current admission, the neurological examination revealed a severe paresis of the proximal right upper limb associated with deltoid and biceps atrophy. Spine magnetic resonance imaging revealed a slightly enhanced tumor infiltration of the third and fourth vertebra extending into the prevertebral and epidural space through the right C5 and C6 foramina [
Figure 1
Sagittal (a) and axial (b) T2-weighted and sagittal (c) and axial (d) gadolinium-enhanced magnetic resonance imaging showing a T2 hyperintense vertebral tumor infiltration of the fourth cervical vertebra with invasion into the spinal canal through the intervertebral foramina with an hourglass feature. Larger tumor masses are found in the prevertebral space (arrow). The tumor showed a partially contrast enhancing (c and d)
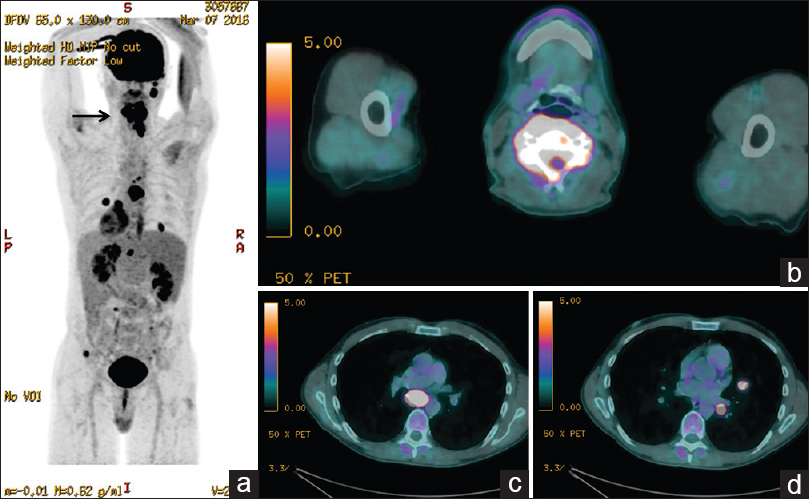
Figure 2
18F fluorodeoxyglucose-positron emission tomography showing a highly hypermetabolic nature of the cervical vertebral mass (SUVbw maximum: 17.9 g/ml) (arrow in a and b) associated with a hypermetabolic infracarinal ganglion (SUVbw maximum: 14.3 g/ml) (c) and multiple hypermetabolic pulmonary nodules (SUVbw maximum: 15.6 g/ml) (d)
DISCUSSION
GBM extraneural metastases occur in only approximately 0.2–0.4% of patients[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Beauchesne P. Extra-neural metastases of malignant gliomas: Myth or reality?. Cancers. 2011. 3: 461-77
2. Goodwin CR, Liang L, Abu-Bonsrah N, Hdeib A, Elder BD, Kosztowski T. Extraneural Glioblastoma Multiforme Vertebral Metastasis. World Neurosurg. 2016. 89: 578-82
3. Piccirilli M, Brunetto GM, Rocchi G, Giangaspero F, Salvati M. Extra central nervous system metastases from cerebral glioblastoma multiforme in elderly patients. Clinico-pathological remarks on our series of seven cases and critical review of the literature. Tumori. 2008. 94: 40-51