- Department of Neurosurgery, Federal University of Ceará, Brazil.
- Department of Neurosurgery, North Regional Hospital, Sobral, Ceará, Brazil.
Correspondence Address:
Joaquim Francisco Cavalcante-Neto
Department of Neurosurgery, Federal University of Ceará, Brazil.
DOI:10.25259/SNI_105_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Joaquim Francisco Cavalcante-Neto1, Lúcio Soares e Silva-Neto1, Paulo Roberto Lacerda Leal2, Cláudio Henrique Souza Moreira2, Espártaco Moraes Lima Ribeiro1, Gerardo Cristino-Filho2, Keven Ferreira da Ponte2. Multiple extradural spinal arachnoid cysts: A case report. 17-Mar-2021;12:101
How to cite this URL: Joaquim Francisco Cavalcante-Neto1, Lúcio Soares e Silva-Neto1, Paulo Roberto Lacerda Leal2, Cláudio Henrique Souza Moreira2, Espártaco Moraes Lima Ribeiro1, Gerardo Cristino-Filho2, Keven Ferreira da Ponte2. Multiple extradural spinal arachnoid cysts: A case report. 17-Mar-2021;12:101. Available from: https://surgicalneurologyint.com/surgicalint-articles/10650/
Abstract
Background: Extradural spinal arachnoid cysts (SACs) rarely cause neural compression and disability.
Case Description: A 38-year-old female presented with a history of two episodes of falling due to transient weakness in the lower limbs. The neurological examination showed normal motor and sensory function, but hyperreflexia. The thoracic magnetic resonance imaging revealed multiple extradural SACs between the T3-L1 levels. Following complete surgical resection of the most symptomatic cyst, she did well. The histopathological examination confirmed a Type I extradural SAC.
Conclusion: Here, we discussed one case and reviewed the literature on the diagnosis and treatment of multiple extradural SACs.
Keywords: Extradural cyst, Extradural spinal arachnoid cyst, Spinal cord, Spinal meningeal cyst
INTRODUCTION
Arachnoid cysts are lesions characterized as collections of cerebrospinal fluid (CSF) lined by arachnoid-like cells (i.e., a diverticulum from a CSF leak). They rarely occur in the spinal region. Although they originate from the arachnoid, these cysts most often occupy the extradural compartment.
There are only 31 cases of multiple extradural spinal arachnoid cysts (SACs) in the literature; of these, only 7 were treated with a partial removal. Here, we present a case of multiple extradural SACs occurring in an adult and discuss the diagnosis (i.e., presentation with spinal cord/root compression) and treatment of these lesions.
CASE PRESENTATION
A 38-year-old female presented with chronic middle back pain, since 2016. She also reported two episodes of transient weakness in the lower extremities accompanied by falls within the last year. Her neurological examination revealed bilateral patellar hyperreflexia, but there was no evidence of any motor or sensory deficits.
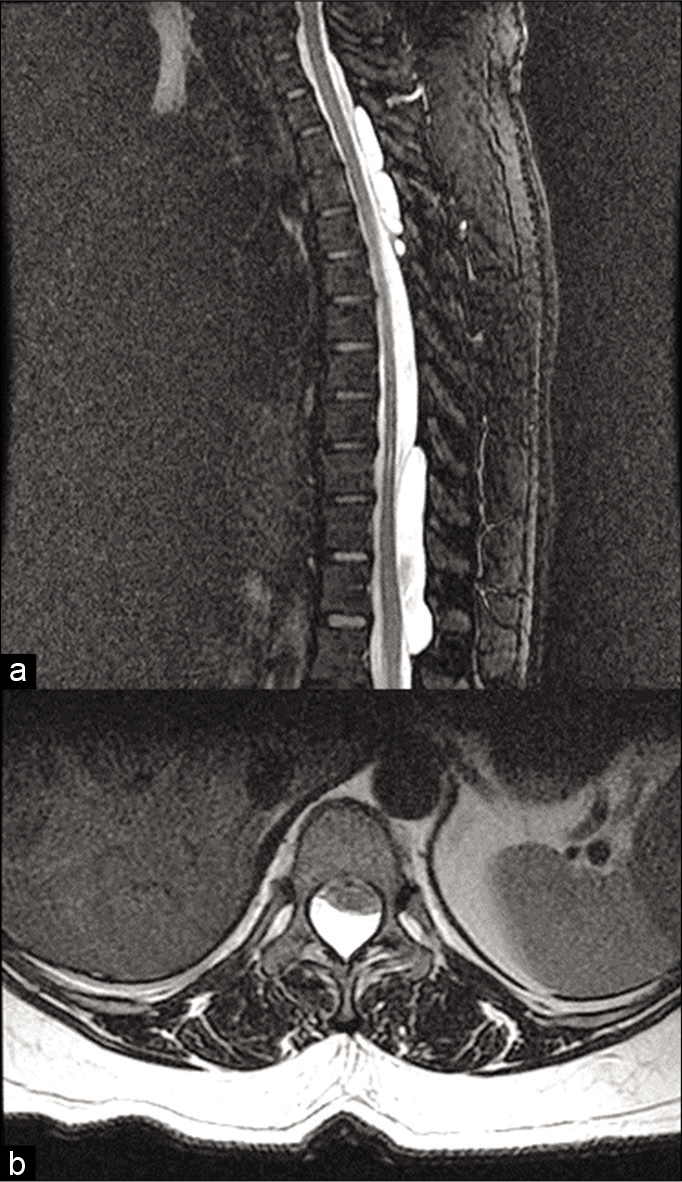
Magnetic resonance imaging (MRI) examinations of the entire spine revealed multiple cystic-appearing lesions dorsal to the spinal cord at the T3-T5 and T10-L1 levels [
Figure 1:
Preoperative imaging. (a) Mid-sagittal T2WI with fat suppression magnetic resonance imaging (MRI) demonstrating multiple (4) extradural spinal arachnoid cysts at T3-T5 and T10-L1 levels. (b) Axial T2 MRI demonstrating the surgically approached cyst at the T11 level, with spinal cord compression.
Surgery
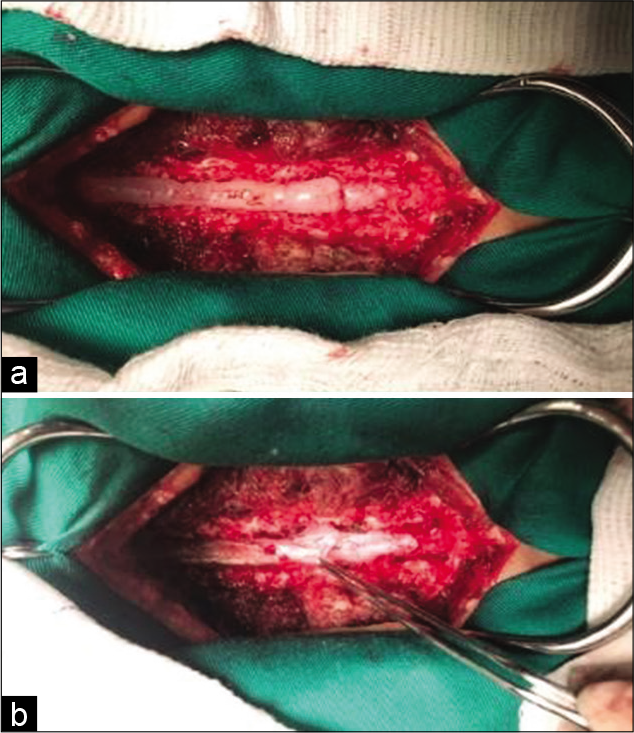
The patient underwent a laminectomy at the T10/11 level for a complete cyst resection [
Histopathology
The histopathological examination confirmed the diagnosis of an arachnoid cyst (Type I extradural SAC). It described the presence of a fibrous wall and absence of neoplasia or dysplasia signs. The cyst measured 3.2 × 2.1 × 0.4 cm.
Postoperative course
After a 3-month follow-up, the back pain significantly improved and the neurological exam normalized. As the partial removal was successful, the patient warranted and continues to require clinical and radiological follow-up for the cephalad untreated cysts.
DISCUSSION AND LITERATURE REVIEW
The most common site of SACs is the posterior aspect of the spinal cord (80%) and the thoracic region (70%), possibly because of the thoracic cord length and its narrower spinal canal. [
Their pathogenesis remains unclear and there are various theories: a diverticulum or congenital dural malformation with arachnoid herniation, the genesis of a septum posticum diverticulum, or a collection of arachnoid granulations with CSF production.[
Nabors et al.[
Multiple SACs
Multiple (>1) extradural SACs are even less frequently encountered expansile spinal cord lesions with only 31 cases found in the literature and rarely contribute to spinal cord or nerve root compression. There is a female preponderance (57%). Cloward [
The clinical manifestations can include pain, gait ataxia, paresthesia, urinary and/or intestinal incontinence, and spastic/flaccid paralysis. Doita et al. [
Diagnostic studies
MRI
MRI is the most recommended exam for a location-based classification. T1- and T2-weighted sagittal sequences are analyzed mainly, and in both, the CSF is as isointense as the arachnoid cyst. Gradient echo and short-tau inversion recovery, MRI sequence parameters, allow artifact reduction and a distinction between spinal cyst and adipose tissue, respectively. [
Computerized tomography (CT)/myelo-CT
CT is a low yield examination because of poor visualization of the spinal cord, but the CT myelogram is efficient at verifying dural leaks or the mass effect from the cyst.[
Surgery
Surgery consisting of a posterior approach by laminectomy or laminoplasty with en bloc cyst excision is the treatment of choice. It is recommended in case of cyst expansion, bony/ neural compression, and/or evolution of a cauda equina syndrome. Partial surgical resection of the most symptomatic lesions appears to be a good therapeutic option. [
CONCLUSION
Although rare, it is important to be aware of and understand the possible presentation of multiple extradural SACs.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Carrillo R. Lumbar cerebrospinal fluid drainage for symptomatic sacral nerve root cysts: An adjuvant diagnostic procedure and/or alternative treatment? Technical case report. Neurosurgery. 1998. 42: 952-3
2. Choi SW, Seong HY, Roh SW. Spinal extradural arachnoid cyst. J Korean Neurosurg Soc. 2013. 54: 355-8
3. Cloward RB. Congenital spinal extradural cysts: Case report with review of literature. Ann Surg. 1968. 168: 851-64
4. Doita M, Nishida K, Miura J, Takada T, Kurosaka M, Fujii M. Kinematic magnetic resonance imaging of a thoracic spinal extradural arachnoid cyst: An alternative suggestion for exacerbation of symptoms during straining. Spine (Phila Pa 1976). 2003. 28: E229-33
5. Eroglu U, Bozkurt M, Kahilogullari G, Dogan I, Ozgural O, Shah KJ. Surgical management of spinal arachnoid cysts in adults. World Neurosurg. 2019. 122: e1146-52
6. Li L, Ali M, Menezes AH, Dlouhy BJ. Intracranial extradural arachnoid cyst in a child. Childs Nerv Syst. 2017. 33: 2201-4
7. Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988. 68: 366-77
8. Simgen A. Spinal cysts: Diagnostic workup and therapy. Radiologe. 2018. 58: 113-9
9. Yu J, Chen S, Zhang J, Wu Q, Xu J. Should we resect all multiple intraspinal extradural arachnoid cysts? A case report. Turk Neurosurg. 2012. 22: 465-8